I. Definition
A. Pain is a word used to describe a subjective perception of distress
B. The physiologic process of pain begins with a series of neurologic steps that begin with stimulation of peripheral nerves and transmission through the spinal cord tracts to the brain, where impulses are interpreted and experienced as pain
C. Because pain historically has been undertreated, many new patient education publications have been developed that include a list of rights for patients with pain
D. The American Pain Society has created the phrase “Pain: The 5th Vital Sign”™ to elevate awareness of pain treatment among health care professionals; if pain were assessed with the same zeal as other vital signs are, the chance that appropriate treatment would be provided for pain would be much greater
II. Types of pain
A. Acute pain
1. Generally caused by tissue damage
2. Duration usually short (less than 6 months)
3. Normally subsides with appropriate interventions and as healing or resolution of tissue damage occurs
B. Chronic pain
1. Generally prolonged (longer than 6 months)
2. May be continual or episodic
3. Usually produces significant negative changes in an individual’s life
4. Treatment is designed to improve or stabilize the patient’s status
5. Frequent reevaluation is required
6. Combination therapy is usually used
III. Pain location
A. Cutaneous
1. Localized on skin or body surface
B. Visceral
1. Poorly localized
2. Originating in internal organs
C. Somatic
1. Nonlocalized
2. Originating in muscle, bone, nerves, blood vessels, and supporting tissue
D. Neuropathic
1. May be referred to as somatic
2. Specifically caused by nerve injury or spinal cord compression
3. Frequently caused by a tumor
IV. Subjective findings
A. The most reliable indicator of the existence and intensity of acute pain is the patient’s self-report
1. Pain can be perceived only by the person who is experiencing it
2. Pain is what the experiencing person says it is
B. Many times, the experience of pain is expressed on a continuum from using descriptive words to moaning, groaning, facial grimacing, crying, and screaming
C. Pain can be described in many ways ranging from sharp, knifelike pain to dull, prolonged pain
D. Intensity can be mild to severe; pain can be constant or intermittent
E. Psychological and cultural factors can influence a person’s interpretation of and response to pain
V. Physical examination findings
A. Elevated heart rate, respiratory rate, blood pressure (in particular systolic), and temperature (over time)
B. Decreased O2 saturation
C. Guarding a particular area or tenderness to palpation
D. Acute tissue damage, such as trauma, burns, or surgery
VI. Diagnostic tests
A. Tests may include the following:
1. CBC, electrolytes
2. Biochemical tests for liver, kidney, and pancreatic function
3. ECG
5. Biopsy
VII. Pain assessment
A. Comprehensive approach to pain assessment requires evaluation of the following:
1. Patient’s self-report
2. Physiologic and behavioral responses
B. Consider asking the patient who is experiencing pain the following questions:
1. What are the location, intensity, and quality of the pain? Describe its onset, duration, and variations or rhythms.
2. What relieves the pain and causes the pain?
3. What effects has the pain had on your life?
4. What other comments about your pain have not been discussed?
C. Three self-report pain assessment tools that are frequently used with adults and children are
1. Numerical rating scale (NRS) of 0 to 10, with 0 being “no pain” and 10 being “worst possible pain” (Fig. 73-1)
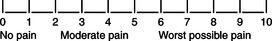 |
| FIGURE 73-10 to 10 numeric pain intensity scale. |
2. Visual analog scale (VAS) with a horizontal line that represents the continuum of no pain to worst possible pain (Fig. 73-2)
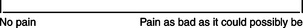 |
| FIGURE 73-2Visual analog scale (VAS). |
3. Adjective rating scale (ARS) that includes descriptive words chosen by the patient to indicate type and intensity of pain (Fig. 73-3)
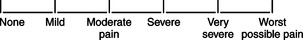 |
| FIGURE 73-3Simple descriptive pain intensity scale. |
4. Wong-Baker Faces Pain Rating Scale for pediatric patients ages 3 to 7 (Fig. 73-4)
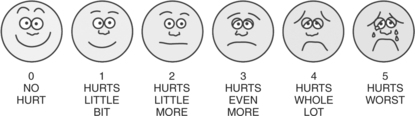 |
| FIGURE 73-4The Wong Baker Faces Scale for rating pain in patients ages 3 to 7.(From Hockenberry-Eaton MJ, Wilson D, Winkelstein ML: Wong’s essentials of pediatric nursing, ed 7, St. Louis, 2005, p 1259. Used with permission. Copyright Mosby.) |
6. Neonatal pain assessment is as important in assessment of the infant as it is in the older patient; many health care providers in neonatal care units use the following criteria for rating:
a. Facial expression
b. Eye squeeze
c. Brow bulge
d. Nasolabial furrow
e. Vocal expression
D. Pain should be assessed and documented
1. Routinely at regular intervals, as determined by pain severity
2. At a suitable interval after each analgesic intervention (30 minutes after parenteral drug therapy and 1 hour after oral analgesics)
3. The Quality of Care Committee of the American Pain Society guidelines conclude that quality assurance programs to improve short- and long-term cancer pain treatment should include five key elements:
a. Ensuring that a report of unrelieved pain raises a “red flag” that attracts the clinician’s attention
b. Making information about analgesics convenient when orders are written
c. Promising patients responsive analgesic care and urging them to communicate about pain
d. Implementing policies and safeguards on the use of modern analgesic technologies
e. Coordinating and assessing implementation of these measures
4. Tiny premature infants feel pain
a. Recent studies of developmental neurobiology of pain indicate that neonates have considerable maturation of afferent pain transmission by 26 weeks’ gestation, and they respond to pain with specific behaviors and with autonomic, hormonal, and metabolic signs of stress and distress
5. The American Academy of Pediatrics and the American Pain Society jointly issued the following statement to emphasize the obligation to treat acute pain in children: “Because of the diversity and complexity of the clinical issues present, pain treatment, including choice of drug, dosage, and route, must be tailored to the individual patient, and analgesia given in the overall context of what is best for the patient.”
E. Short-term effects of inadequate pain management are numerous and involve
1. Significant fluctuations in heart rate, blood pressure, intracranial pressure, and oxygen level
2. Biochemical changes (hormonal response)
a. Increased catecholamine level
b. Increased glucagon level
c. Increased cortisol level
d. Increased aldosterone level
3. Metabolic responses to pain
a. Hyperglycemia
b. Utilization of fat stores/ketones
c. Protein breakdown
4. Sleep disturbances, agitation, crying
F. Long-term effects of inadequate pain management include
1. More frequent clinical complications with inadequate surgical pain management
2. Prolonged hospitalization time and higher mortality rates
3. Behavioral and psychological sequelae
VIII. Pain management




A. Each institution should develop the resources needed to provide the best and most modern pain relief appropriate to its patients and should designate who or which departments are responsible for the required activities
B. Recognizing pain as a major health problem, The Joint Commission has developed standards that create new expectations for the assessment and management of pain in accredited hospitals and other health care settings. These standards have been endorsed by the American Pain Society.
C. Hospitals, home care agencies, nursing homes, behavioral health facilities, outpatient clinics, and health plans will be called upon to
1. Recognize the right of patients to appropriate assessment and management
2. Assess the existence and the nature and intensity of pain
3. Record the results of assessment in a way that facilitates regular reassessment and follow-up
4. Determine and ensure staff competency in pain assessment and management
6. Educate about effective pain management
7. Address patient needs for symptom management in the discharge planning
D. Optimal application of pain control methods depends on cooperation among different members of the health care team throughout the patient’s course of treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
