Skill 71
Subcutaneous Injections
Subcutaneous injections involve depositing medication into the loose connective tissue underlying the dermis. Because subcutaneous tissue does not contain as many blood vessels as muscles, medications are absorbed more slowly than with intramuscular (IM) injections. Physical exercise or application of hot or cold compresses influences the rate of drug absorption by altering local blood flow to tissues. Any condition that impairs blood flow is a contraindication for subcutaneous injections.
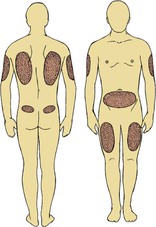
You give subcutaneous medications in small doses of less than 2 mL that are isotonic, nonirritating, nonviscous, and water soluble. The best subcutaneous injection sites include the outer aspect of the upper arms, the abdomen from below the costal margins to the iliac crests, and the anterior aspects of the thighs (Fig. 71-1).
Most patients manage type 1 diabetes mellitus with injections. Anatomical injection site rotation is no longer necessary because newer human insulins carry a lower risk for hypertrophy. Patients choose one anatomical area (e.g., the abdomen) and systematically rotate sites within that region, which maintains consistent insulin absorption from day to day. Absorption rates of insulin vary based on the injection site. Insulin is most quickly absorbed in the abdomen and most slowly in the thighs (Lehne, 2010).
Heparin therapy provides therapeutic anticoagulation to reduce the risk for thrombus formation by suppressing clot formation. Therefore patients receiving heparin are at risk for bleeding, including bleeding gums, hematemesis, hematuria, or melena.
Delegation Considerations
The skill of administering subcutaneous injections cannot be delegated to nursing assistive personnel (NAP). The nurse directs the NAP about:
Equipment
▪ Proper size syringe with engineered sharps injury protection (SESIP) needle:
• Subcutaneous syringe (1 to 3 mL) and needle (25 to 27 gauge,  to
to  inch)
inch)
• Subcutaneous U-100 insulin: insulin syringe (1 mL) with preattached needle (28 to 31 gauge,  to
to  inch)
inch)
• Subcutaneous U-500 insulin: 1-mL tuberculin (TB) syringe with needle (25 to 27 gauge,  to
to  inch)
inch)
▪ Medication administration record (MAR) or computer printout
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree