The Newborn
Care Management: From Birth Through The First 2 Hours
Apgar Score
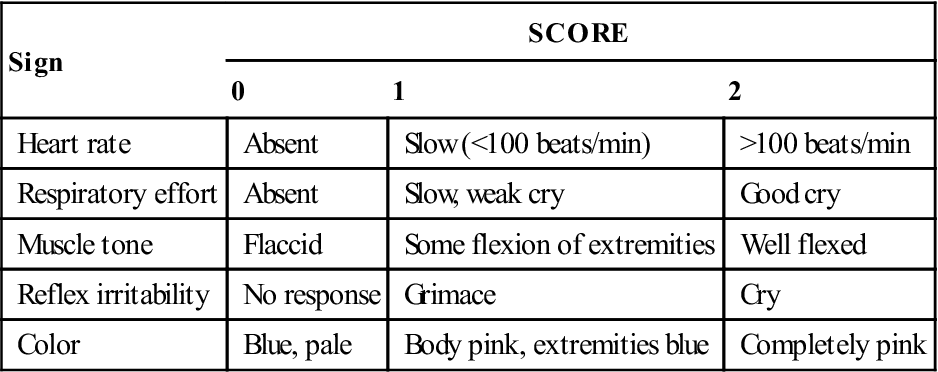
 The nurse usually assigns the Apgar score at 1 and 5 minutes after birth. The Apgar score permits a rapid assessment of the newborn’s transition to extrauterine life based on five signs (Table 7-1). Scores of 0 to 3 indicate severe distress; scores of 4 to 6 indicate moderate difficulty; and scores of 7 to 10 indicate that the infant is having no difficulty adjusting to extrauterine life. If resuscitation is required, it should be initiated before the 1-minute Apgar score.
The nurse usually assigns the Apgar score at 1 and 5 minutes after birth. The Apgar score permits a rapid assessment of the newborn’s transition to extrauterine life based on five signs (Table 7-1). Scores of 0 to 3 indicate severe distress; scores of 4 to 6 indicate moderate difficulty; and scores of 7 to 10 indicate that the infant is having no difficulty adjusting to extrauterine life. If resuscitation is required, it should be initiated before the 1-minute Apgar score.
TABLE 7-1
| Sign | SCORE | ||
| 0 | 1 | 2 | |
| Heart rate | Absent | Slow (<100 beats/min) | >100 beats/min |
| Respiratory effort | Absent | Slow, weak cry | Good cry |
| Muscle tone | Flaccid | Some flexion of extremities | Well flexed |
| Reflex irritability | No response | Grimace | Cry |
| Color | Blue, pale | Body pink, extremities blue | Completely pink |
Initial Physical Assessment
 The initial physical assessment includes a brief review of systems:
The initial physical assessment includes a brief review of systems:
 An assessment of newborn reflexes (Table 7-2) and a more comprehensive physical assessment (Table 7-3) are completed within 24 hours of birth.
An assessment of newborn reflexes (Table 7-2) and a more comprehensive physical assessment (Table 7-3) are completed within 24 hours of birth.
TABLE 7-2
Assessment of Newborn’s Reflexes
| Reflex | Eliciting the Reflex | Characteristic Response | Comments |
| Rooting and sucking | Touch infant’s lip, cheek, or corner of mouth with nipple | Infant turns head toward stimulus, opens mouth, takes hold, and sucks | Response difficult if not impossible to elicit after infant has been fed; if response weak or absent, consider prematurity or neurologic defect Parental guidance: avoid trying to turn head toward breast or nipple, allow infant to root; response disappears after 3-4 mo∗ but can persist upto 1 yr |
| Swallowing | Feed infant; swallowing usually follows sucking and obtaining fluids | Swallowing usually coordinated with sucking and usually occurs without gagging, coughing, or vomiting | If response is weak or absent, may indicate prematurity or neurologic defect Sucking and swallowing often uncoordinated in preterm infant |
| Grasp: | |||
| Palmar | Place finger in palm of hand | Infant’s fingers curl around examiner’s fingers Toes curl downward | Palmar response lessens by 3-4 mo; parents enjoy this contact with infant; plantar response lessens by 8 mo |
| Plantar | Place finger at base of toes | Toes curl downward | |
| Extrusion | Touch or depress tip of tongue | Newborn forces tongue outward | Response disappears about fourth mo of life |
| Glabellar (Myerson) | Tap over forehead, bridge of nose, or maxilla of newborn whose eyes are open | Newborn blinks for first four or five taps | Continued blinking with repeated taps consistent with extrapyramidal disorder |
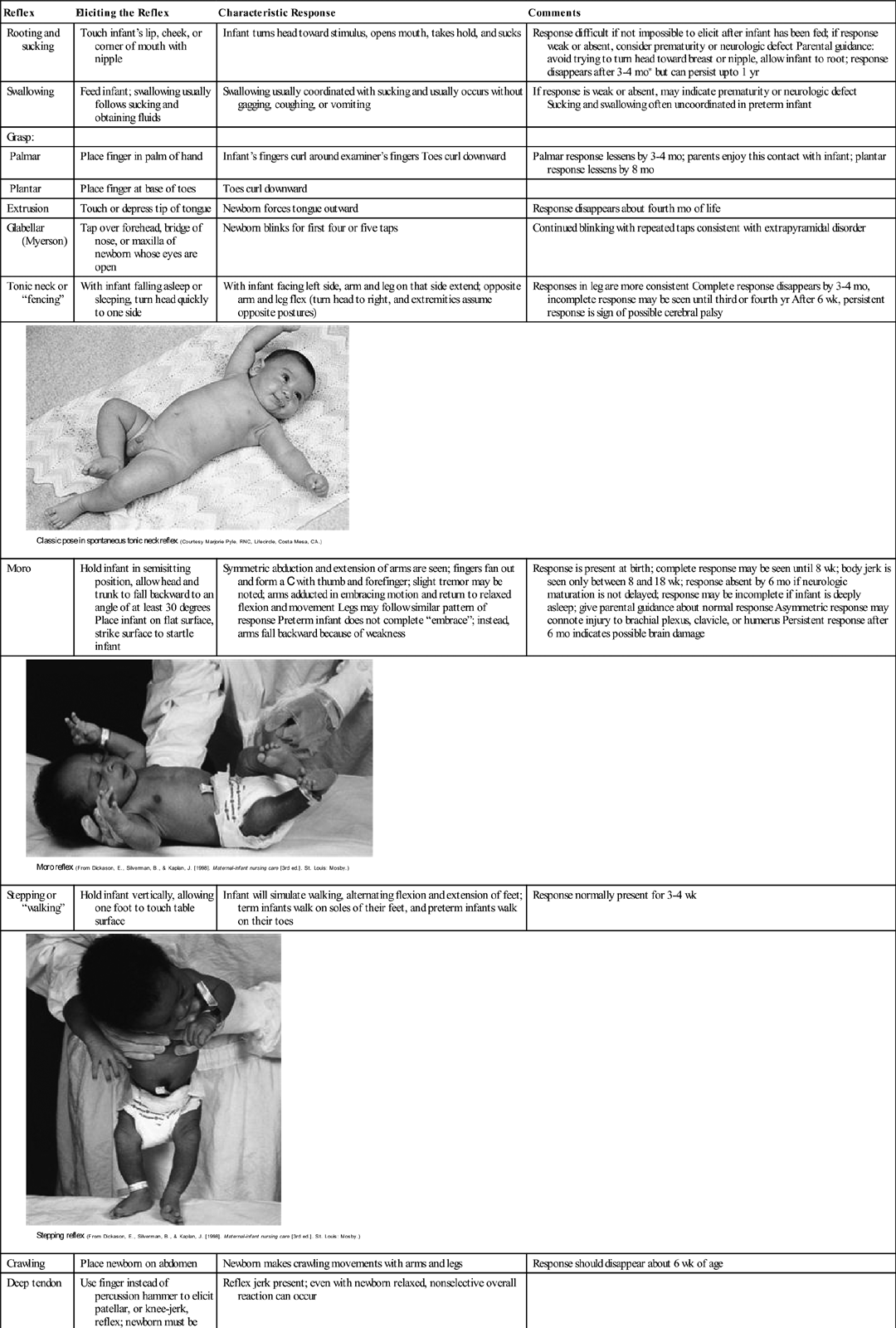
| Tonic neck or “fencing” | With infant falling asleep or sleeping, turn head quickly to one side | With infant facing left side, arm and leg on that side extend; opposite arm and leg flex (turn head to right, and extremities assume opposite postures) | Responses in leg are more consistent Complete response disappears by 3-4 mo, incomplete response may be seen until third or fourth yr After 6 wk, persistent response is sign of possible cerebral palsy |
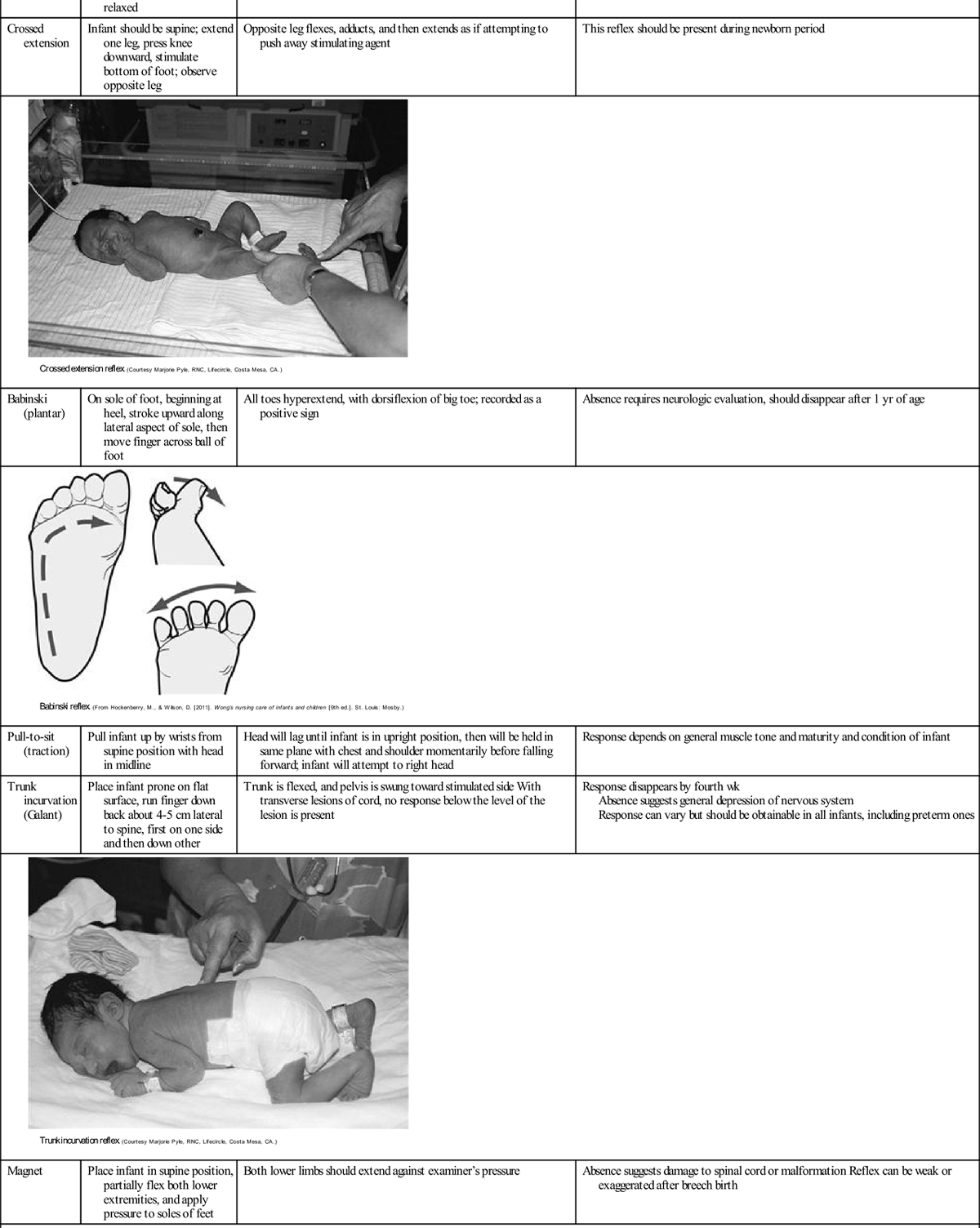
| Moro | Hold infant in semisitting position, allow head and trunk to fall backward to an angle of at least 30 degrees Place infant on flat surface, strike surface to startle infant | Symmetric abduction and extension of arms are seen; fingers fan out and form a C with thumb and forefinger; slight tremor may be noted; arms adducted in embracing motion and return to relaxed flexion and movement Legs may follow similar pattern of response Preterm infant does not complete “embrace”; instead, arms fall backward because of weakness | Response is present at birth; complete response may be seen until 8 wk; body jerk is seen only between 8 and 18 wk; response absent by 6 mo if neurologic maturation is not delayed; response may be incomplete if infant is deeply asleep; give parental guidance about normal response Asymmetric response may connote injury to brachial plexus, clavicle, or humerus Persistent response after 6 mo indicates possible brain damage |
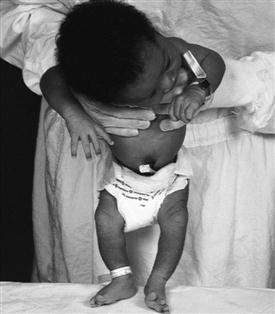
| Stepping or “walking” | Hold infant vertically, allowing one foot to touch table surface | Infant will simulate walking, alternating flexion and extension of feet; term infants walk on soles of their feet, and preterm infants walk on their toes | Response normally present for 3-4 wk |
| Crawling | Place newborn on abdomen | Newborn makes crawling movements with arms and legs | Response should disappear about 6 wk of age |
| Deep tendon | Use finger instead of percussion hammer to elicit patellar, or knee-jerk, reflex; newborn must be relaxed | Reflex jerk present; even with newborn relaxed, nonselective overall reaction can occur | |
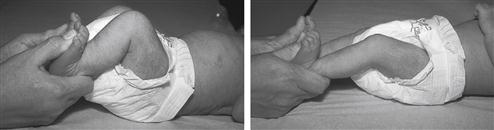
| Crossed extension | Infant should be supine; extend one leg, press knee downward, stimulate bottom of foot; observe opposite leg | Opposite leg flexes, adducts, and then extends as if attempting to push away stimulating agent | This reflex should be present during newborn period |
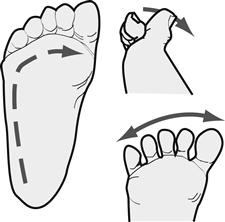
| Babinski (plantar) | On sole of foot, beginning at heel, stroke upward along lateral aspect of sole, then move finger across ball of foot | All toes hyperextend, with dorsiflexion of big toe; recorded as a positive sign | Absence requires neurologic evaluation, should disappear after 1 yr of age |
| Pull-to-sit (traction) | Pull infant up by wrists from supine position with head in midline | Head will lag until infant is in upright position, then will be held in same plane with chest and shoulder momentarily before falling forward; infant will attempt to right head | Response depends on general muscle tone and maturity and condition of infant |
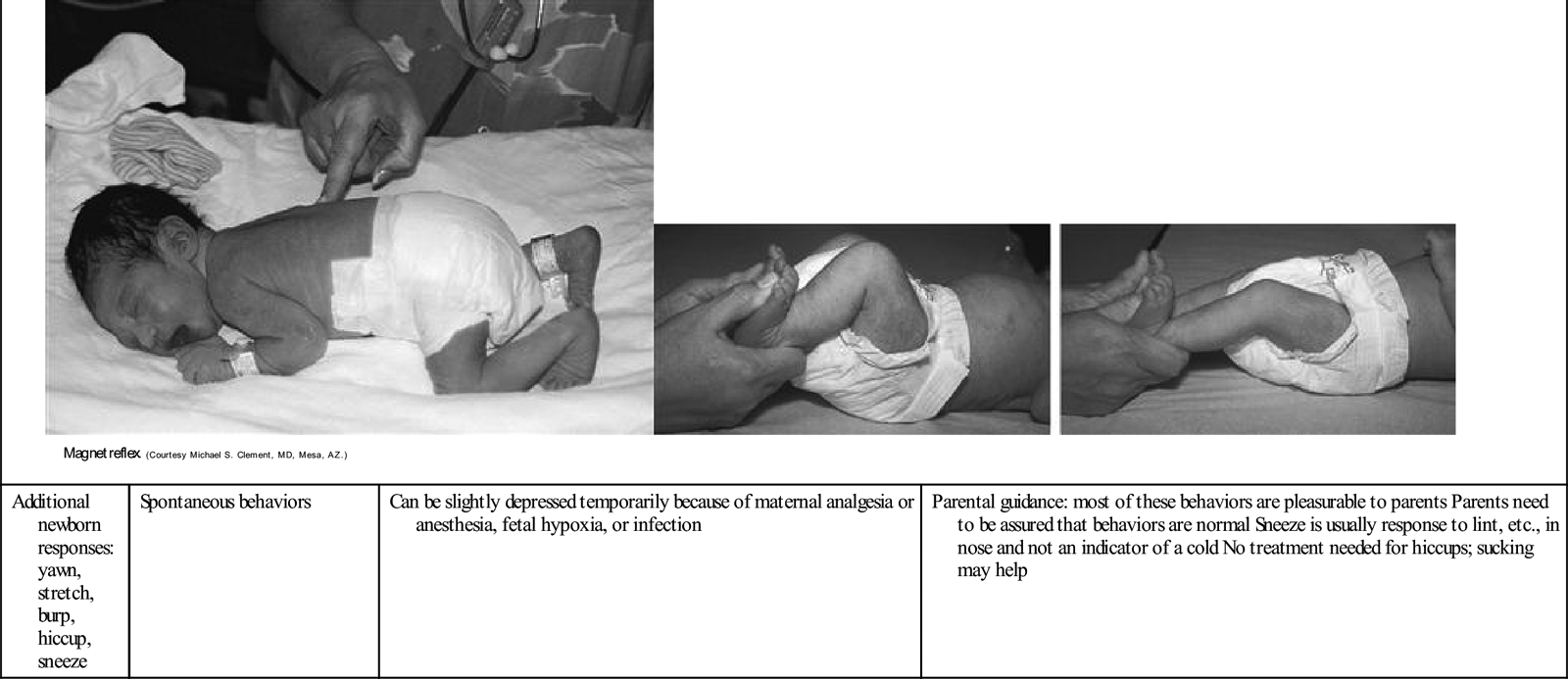
| Trunk incurvation (Galant) | Place infant prone on flat surface, run finger down back about 4-5 cm lateral to spine, first on one side and then down other | Trunk is flexed, and pelvis is swung toward stimulated side With transverse lesions of cord, no response below the level of the lesion is present | Response disappears by fourth wk Absence suggests general depression of nervous system Response can vary but should be obtainable in all infants, including preterm ones |
| Magnet | Place infant in supine position, partially flex both lower extremities, and apply pressure to soles of feet | Both lower limbs should extend against examiner’s pressure | Absence suggests damage to spinal cord or malformation Reflex can be weak or exaggerated after breech birth |
| Additional newborn responses: yawn, stretch, burp, hiccup, sneeze | Spontaneous behaviors | Can be slightly depressed temporarily because of maternal analgesia or anesthesia, fetal hypoxia, or infection | Parental guidance: most of these behaviors are pleasurable to parents Parents need to be assured that behaviors are normal Sneeze is usually response to lint, etc., in nose and not an indicator of a cold No treatment needed for hiccups; sucking may help |
∗All durations for persistence of reflexes are based on time elapsed after 40 wk of gestation; that is, if this newborn was born at 36 wk of gestation, add 1 mo to all time limits given.
TABLE 7-3
Physical Assessment of Newborn
| Area Assessed | Normal Findings | Deviations From Normal Range | Etiology |
| POSTURE | |||
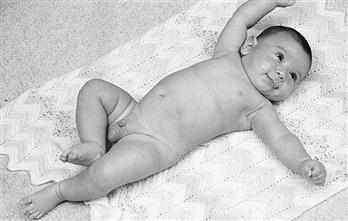
| Inspect newborn before disturbing | Arms, legs in moderate flexion; fists clenched | Hypotonia | Prematurity or hypoxia in utero, maternal medications |
| Normal spontaneous movement bilaterally; asynchronous but equal extension in all extremities | Hypertonia | Drug dependence, central nervous system (CNS) disorder | |
| Opisthotonos | CNS disturbance | ||
| Frank breech: legs straighter and stiff | |||
| Limitation of motion in any of extremities | |||
| VITAL SIGNS | |||
| Heart rate and pulses: | |||
| Sounds distant, poor quality, extra | Pneumomediastinum | ||
| Heart on right side of chest | Dextrocardia, often accompanied by reversal of intestines | ||
| Peripheral pulses: femoral, brachial, popliteal, posterior tibial | |||
| Temperature: axillary method of choice | Axillary: 36.5°-37.2° C | Subnormal | Prematurity, infection, low environmental temperature, inadequate clothing, dehydration |
| Increased | Infection, high environmental temperature, excessive clothing, proximity to heating unit or in direct sunshine, drug addiction, diarrhea and dehydration | ||
| Temperature stabilized by 8-10 hr of age | Temperature not stabilized by 6-8 hr after birth | If mother received magnesium sulfate, maternal analgesics | |
| Check respiratory rate and effort when infant is at rest Count respirations for full min | Apneic episodes: >15 sec | Preterm infant: “periodic breathing,” rapid warming or cooling of infant | |
| Subnormal | Bradypnea: <25/min | Maternal narcosis from analgesics or anesthetics, birth trauma | |
| Breath sounds loud, clear | Tachypnea: >60/min | Narrowing of bronchi, RDS, congenital diaphragmatic hernia, transient tachypnea of the newborn | |
| Crackles may be heard after birth | Fluid in lungs | ||
| 80-90/40-50 (mm Hg) | Difference between upper and lower extremity pressures | Coarctation of aorta | |
| Hypotension | Sepsis, hypovolemia | ||
| Hypertension | Coarctation of aorta, renal involvement, thrombus | ||
| WEIGHT∗ | |||
| Weigh at same time each day | Weight <2500 g | Prematurity, small for gestational age, rubella syndrome | |
| Second baby weighs more than first | Weight ≥4000 g | Large for gestational age, maternal diabetes, heredity—normal for these parents | |
| Birth weight regained within first 2 wk | Weight loss >10%-15% | Dehydration | |
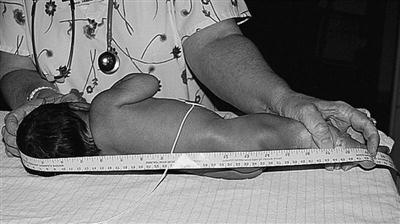
| LENGTH | |||
| Length from top of head to heel | 45-55 cm | <45 cm or >55 cm | Chromosomal abnormality, heredity—normal for these parents |
| HEAD CIRCUMFERENCE | |||
| Occipito-frontal circumference | Small head, <32 cm: microcephalyHydrocephaly: sutures widely separated, circumference ≥4 cm more than chest circumference | Prematurely, maternal rubella, toxoplasmosis, cytomegalic inclusion disease, fused cranial sutures (craniosynostosis) | |
| Maldevelopment, infection | |||
| Increased intracranial pressure | Hemorrhage, space-occupying lesion | ||
| CHEST CIRCUMFERENCE | |||
| Measure at nipple line | 2-3 cm less than head circumference, averages between 30 and 33 cm | <30 cm | Prematurity |
| SKIN | |||
| Color | Generally pink | Dark red | Prematurity, polycythemia |
| Varying with ethnic origin | Gray | Hypotension, poor perfusion | |
| Pallor | Cardiovascular problem, CNS damage, blood dyscrasia, blood loss, twin-to-twin transfusion, nosocomial infection | ||
| Cyanosis | Hypothermia; infection; hypoglycemia; cardiopulmonary diseases; cardiac, neurologic, or respiratory malformations | ||
| Petechiae over presenting part | Petechiae over any other area | Clotting factor deficiency, infection | |
| Ecchymoses from forceps in vertex births or over buttocks, genitalia, and legs in breech births | Ecchymoses in any other area | Hemorrhagic disease, traumatic birth | |
| Jaundice | None at birth | Jaundice within first 24 hr | Increased hemolysis, Rh isoimmunization, ABO incompatibility |
| Physiologic jaundice in up to 50% of term infants in first wk of life | |||
| Birthmarks | Mongolian spots: | ||
| Check condition | No skin edema | Edema on hands, feet; pitting over tibia | Overhydration |
| Opacity: few large blood vessels visible indistinctly over abdomen | Texture thin, smooth, or of medium thickness; rash or superficial peeling visible | Prematurity, postmaturity | |
| Numerous vessels very visible over abdomen | Prematurity | ||
| Postmaturity | |||
| Papules, pustules, vesicles, ulcers, maceration | Impetigo, candidiasis, herpes, diaper rash | ||
| Gently pinch skin between thumb and forefinger over abdomen and inner thigh to check for turgor | After pinch released, skin returns to original state immediately | Prematurity, postmaturity, dehydration: fold of skin persisting after release of pinch | |
| Tense, tight, shiny skin | Edema, extreme cold, shock, infection | ||
| Normal weight loss after birth: 7 to 10% of birth weight | Lack of subcutaneous fat, prominence of clavicle or ribs | Prematurity, malnutrition | |
| Possibly puffy | |||
| Vernix caseosa: color and odor | Whitish, cheesy, odorless; usually more found in creases, folds | Absent or minimal | Postmaturity |
| Excessive | Prematurity | ||
| Green color | Possible in utero release of meconium or presence of bilirubin | ||
| Odor | Possible intrauterine infection | ||
| Lanugo | Over shoulders, pinnae of ears, forehead | Absent | Postmaturity |
| Excessive | Prematurity, especially if lanugo abundant and long and thick over back | ||
| HEAD | |||
| Inspect palpate | |||
| Fontanels: open vs. closed | Anterior fontanel 5-cm diamond, increasing as molding resolves | Full, bulging | Tumor, hemorrhage, infection |
| Large, flat, soft | Malnutrition, hydrocephaly, retarded bone age, hypothyroidism | ||
| Posterior fontanel triangle, smaller than anterior | |||
| Sutures | |||
| Hair | Silky, single strands lying flat; growth pattern toward face and neck, variation in amount | Fine, woolly | Prematurity |
| Unusual swirls, patterns, or hairline or coarse, brittle | Endocrine or genetic disorders | ||
| EYES | |||
| Eyeballs | Both present and of equal size, both round, firm | Agenesis or absence of one or both eyeballs | |
| Epicanthal folds when present with other signs | Chromosomal disorders, such as Down, cri du chat syndromes | ||
| Symmetric in size, shape | Small eyeball | Rubella syndrome | |
| Blink reflex | Lens opacity or absence of red reflex | Congenital cataracts, possibly from rubella | |
| Subconjunctival hemorrhage | Lesions: coloboma (absence of part of iris) | ||
| Pink color of iris | Albinism | ||
| Jaundiced sclera | Hyperbilirubinemia | ||
| Pupils | Present, equal in size, reactive to light | Pupils: unequal, constricted, dilated, fixed | Intracranial pressure, medications, tumors |
| Eyeball movement | Increased intracranial pressure | ||
| Sunset | Increased intracranial pressure | ||
| Eyebrows | Distinct (not connected in midline) | Connection in midline | Cornelia de Lange syndrome |
| NOSE | |||
| Copious drainage, with or without regular periods of cyanosis at rest and return of pink color with crying | Choanal atresia, congenital syphilis, chromosomal disorder | ||
| Slight deformity (flat or deviated to one side) from passage through birth canal | Malformed | Congenital syphilis | |
| Flaring of nares | Respiratory distress | ||
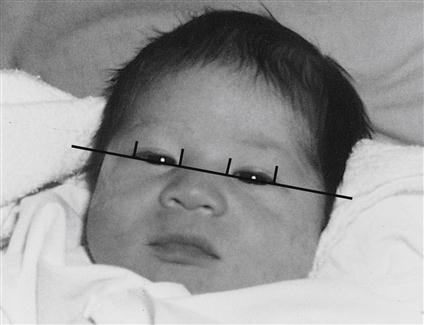
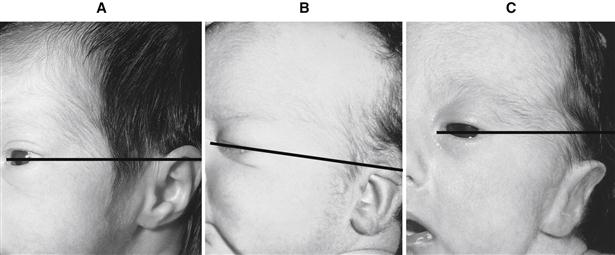
| EARS | |||
| Pinna | Correct placement: line drawn through inner and outer canthi of eyes reaching to top notch of ears (at junction with scalp) | Agenesis | |
| Well-formed, firm cartilage | |||
| Hearing | Responds to voice and other sounds | No response to sound | Deaf, rubella syndrome |
| State (e.g., alert, asleep) influences response | |||
| FACIES | |||
| Observe overall appearance of face | “Normal” appearance, well-placed, proportionate, symmetric features | Infant appearance “odd” or “funny” | Hereditary, chromosomal aberration |
| Positional deformities | Usually accompanied by other features, such as low-set ears, other structural disorders | ||
| MOUTH | |||
| Gums | Teeth: predeciduous or deciduous | Hereditary | |
| Tongue | |||
| Palate (soft, hard): | |||
| Arch | Soft and hard palates intact | Cleft, hard or soft palate | |
| Uvula | Uvula in midline | ||
| Epstein pearls | |||
| Chin | Distinct chin | Micrognathia | Pierre Robin sequence or other syndrome |
| Saliva | Mouth moist | Excessive saliva | Esophageal atresia, tracheoesophageal fistula |
| Reflexes: | Absent | Prematurity | |
| NECK | |||
| Sternocleidomastoid muscles | Short, thick, surrounded by skin folds; no webbing | Webbing | Turner syndrome |
| Thyroid gland | Thyroid not palpable | Masses | Enlarged thyroid |
| Distended veins | Cardiopulmonary disorder | ||
| CHEST | |||
| Thorax | Almost circular, barrel shaped | Bulging of chest, unequal movement | Pneumothorax, pneumomediastinum |
| Tip of sternum possibly prominent | Malformation | Funnel chest—pectus excavatum | |
| Respiratory movements | Symmetric chest movements, chest and abdominal movements synchronized during respirations | Retractions with or without respiratory distress, seesaw respirations | Prematurity, RDS |
| Occasional retractions, especially when crying | |||
| Clavicles | Clavicles intact | Fracture of clavicle; crepitus | Trauma |
| Ribs | Rib cage symmetric, intact; moves with respirations | Poor development of rib cage and musculature | Prematurity |
| Nipples | Prominent, well formed; symmetrically placed | Supernumerary, along nipple line Malpositioned or widely spaced | |
| Breast tissue | Breast nodule: approximately 3-10 mm in term infant | Lack of breast tissue | Prematurity |
| Secretion of witch’s milk | Maternal hormones | ||
| ABDOMEN | |||
| Umbilical cord | Two arteries, one vein | One artery | Renal anomalies |
| Whitish gray | Meconium stained | Intrauterine distress | |
| Definite demarcation between cord and skin, no intestinal structures within cord | Bleeding or oozing around cord | Hemorrhagic disease | |
| Redness or drainage around cord | Infection, possible persistence of urachus | ||
| Dry around base, drying | Herniation of abdominal contents into area of cord (e.g., omphalocele); defect covered with thin, friable membrane, possibly extensive | ||
| Odorless | |||
| Cord clamp in place for 24 hr | |||
| Reducible umbilical hernia | |||
| Rounded, prominent, dome shaped because abdominal musculature not fully developed | Gastroschisis: fissure of abdominal cavity | ||
| Some diastasis of abdominal musculature | |||
| Liver possibly palpable 1-2 cm below right costal margin | |||
| No other masses palpable | |||
| No distention | Distention at birth | Ruptured viscus, genitourinary masses or malformations: hydronephrosis, teratomas, abdominal tumors | |
| Mild | Overfeeding, high gastrointestinal tract obstruction | ||
| Marked | Lower gastrointestinal tract obstruction, imperforate anus | ||
| Intermittent or transient | Overfeeding | ||
| Partial intestinal obstruction | Stenosis of bowel | ||
| Visible peristalsis | Obstruction | ||
| Malrotation of bowel or adhesions | |||
| Sepsis | Infection | ||
| Bowel sounds | Sounds present within minutes after birth in healthy term infants | Scaphoid, with bowel sounds in chest and respiratory distress | Diaphragmatic hernia |
| Stools | Meconium stool passing within 24-48 hr after birth | No stool | Imperforate anus |
| Color | Linea nigra possibly apparent | Hormone influence during pregnancy | |
| Movement with respiration | Respirations primarily diaphragmatic, abdominal and chest movement synchronous | Decreased abdominal breathing | Intrathoracic disease, phrenic nerve palsy, diaphragmatic hernia |
| “Seesaw” | Respiratory distress | ||
| GENITALIA | |||
| Female | |||
| General appearance | Female genitalia | Ambiguous genitalia—enlarged clitoris with urinary meatus on tip, fused labia | Chromosomal disorder, maternal drug ingestion |
< div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |||