Chapter 7 Renal disorders
RELEVANT ANATOMY AND PHYSIOLOGY
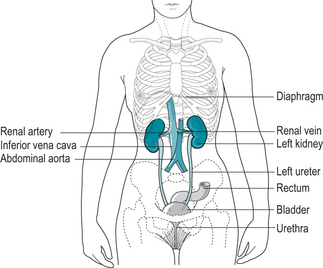
The renal system is composed of (Fig. 7.1):
The kidney contains the functional units of the renal system – the nephrons. These microscopic structures, of which there are approximately 1 million, are responsible for several related functions. They filter and excrete water, electrolytes and nitrogenous waste products and maintain acid-base balance. They also play a major role in blood pressure control via the renin–angiotensin pathway, and produce erythropoietin factor, a substance involved in the production of red blood cells.
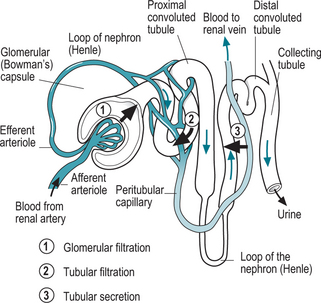
To achieve these major functions, the kidneys receive 20–25% of arterial blood directly fromthe aorta. The majority of this blood is transported directly to the nephrons where urine is produced. The anatomy of the nephron is shown in Figure 7.2. Three major processes are involved in urine production:
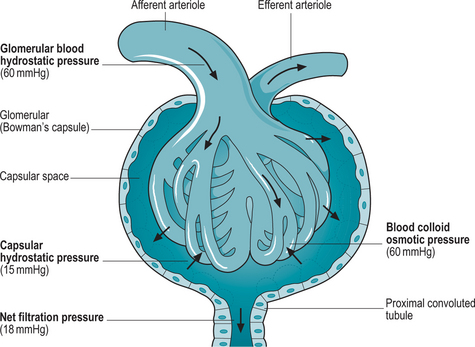
Glomerular filtration
Net filtration pressure is the driving force of this process and is made up of three components: hydrostatic pressure in both the glomerular capillaries and Bowman’s capsule, and osmotic pressure (Fig. 7.3). The filtrate that is produced is very dilute and contains both useful and waste products.
Selective tubular reabsorption
Other functions of the nephron
Blood pressure regulation
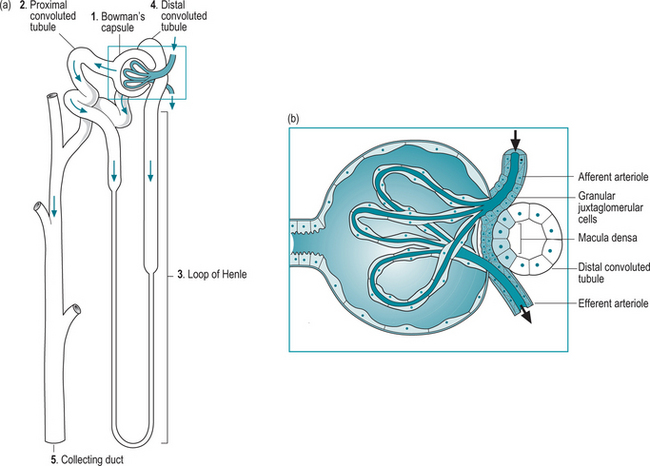
Another physiological process, in which the nephron plays a vital role, is in blood pressure regulation. Anatomically, the final section of the ascending limb of the loop of Henle comes into close proximity with the afferent arteriole of the nephron (Fig. 7.4). At this point, the walls of both structures contain specialized cells forming the juxtaglomerular apparatus. The cells in the nephron make up the macula densa – a compact collection of cells that measure the amount of sodium in the filtrate. The corresponding cells in the arteriole, the juxtaglomerular cells, contain muscle fibres and granules of renin.
PATHOPHYSIOLOGY
Aetiology
Infection
Bacteria from the gastrointestinal tract are the commonest causative agents in urinary tract infection. Often this is Escherichia coli. As a result of the close proximity of the urethral meatus to the anus, contamination of the perineum spreads easily into the urethra particularly if personal hygiene is poor. Abrasion of the urinary meatus during sexual intercourse can also result in entry of pathogens to the renal system. The short length of the urethra then enables infective organisms to reach the bladder easily and proliferate. Infection in the bladder may spread to the ureters and on into the kidney itself causing inflammation, pyelonephritis and possible damage to the nephrons themselves.
Acute renal failure
The kidneys are particularly vulnerable during any event where there is circulatory shut down (Perkins & Kisel 2005). Acute blood loss, toxic shock from overwhelming infection can both lead to acute renal failure as can a urinary obstruction or damage resulting in backflow of urine.
Pathophysiology
Two important processes may be compromised by inflammation in the renal system. Fluid and electrolyte imbalance may occur as the inflamed tubules of the nephron become less efficient at reabsorbing sodium, which is then retained in body tissues and fluids. With retention of sodium, water is also retained, resulting in oedema and/or increased cardiac workload. Acid-base balance will also be affected as secretion of buffering substances is compromised and hydrogen ions are retained in the body (Box 7.1).
Box 7.1 Acid-base balance
Acid-base balance is maintained through three systems:
Chronic renal disease is usually the result of secondary damage to the kidneys as a result of another disease process. Commonly, this is due to hypertension but other causes are polycystic kidneys and glomerulonephritis. Examples of these related to pregnancy are:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree