Section Seven Inhalation Therapy
PROCEDURE 36 Nebulizer Therapy
Nebulizer therapy is also known as neb, updraft, SVN (small-volume nebulizer), and acorn neb.
CONTRAINDICATION AND CAUTIONS
1. A metered-dose inhaler (MDI) with a spacer is preferred over a nebulizer, even for administering bronchodilators during severe asthma exacerbations (GINA & NHLBI, 2005). Nebulizers are not preferred for maintenance treatment either because they are expensive, not very portable, more difficult to use and maintain, and do not provide precise drug delivery unless equipped with a dosimeter (GINA & NHLBI, 2005).
2. Patients who are in distress, confused, or who cannot cooperate with the procedure, or whose history-taking requires talking while receiving treament will benefit from an aerosol mask fitted closely to the face with corrugated mist tubing extensions placed in the exhalation ports. Commonly referred to as horns, whiskers, or tusks, these act as a reservoir for aerosolized medication that would otherwise have been wasted to the atmosphere. The constant flow and the looseness of the mask prevent CO2 rebreathing.
3. Patients with chronic obstructive pulmonary disease should generally receive nebulizer treatments with compressed air instead of oxygen. Supplemental oxygen dosing may be individualized without alteration by the rapid flow of the nebulizer. The nebulizer can be adapted to the side port of a Venturi mask providing fixed oxygen concentrations.
4. Nebulized medications are contraindicated in the presence of absent or severely diminished breath sounds unless the nebulized medication is delivered through an endotracheal tube that uses positive pressure. A patient with decreased air exchange may not be able to move the medication adequately into the respiratory tract.
5. Many bronchodilators are catecholamines and should be used with caution in patients with cardiac irritability. When inhaled, catecholamines increase the cardiac rate and may precipitate dysrhythmias.
EQUIPMENT
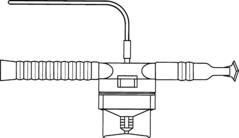
Nebulizer and connecting tubing (Figure 36-1)
Compressed gas source (oxygen or air) or air compressor
Table 36-1 MEDICATIONS COMMONLY ADMINISTERED VIA NEBULIZER
| Generic Name | Type of Medication | Trade Name |
|---|---|---|
| Albuterol | Bronchodilator | Ventolin, Proventil |
| Ipratropium bromide | Anticholinergic bronchodilator | Atrovent |
| Albuterol + ipratropium | Combination of bronchodilators | DuoNeb |
| Levalbuterol HCl | Bronchodilator | Xopenex |
| Metaproterenol | Bronchodilator | Alupent |
| Racemic epinephrine | Bronchodilator | Vaponefrin |
| Cromolyn sodium | Mast cell stabilizer, antiasthmatic | Intal |
PATIENT PREPARATION
1. Place the patient in an upright position (40 to 90 degrees), which allows deep ventilation and maximal diaphragmatic movement.
2. Assess the breath sounds, pulse rate, respiratory status, oxygen saturation (see Procedure 21), and peak flow (see Procedure 23), if possible, before administering the medication.
3. Assess the heart rate during the treatment. If the heart rate increases by 20 beats per minute, stop the nebulizer treatment. In pregnant patients, the fetal heart rate should also be assessed (see Procedure 108).
4. Instruct the patient take slow deep breaths through the mouth and hold at end inspiration.
PROCEDURAL STEPS
1. Place the patient on supplemental oxygen (see Procedure 25), with the device and flow rate determined by the patient’s condition, pulse oximetry, and/or arterial blood gases.
2. Assemble the nebulizer and the tubing and instill the medication into the nebulizer.
3. Add normal saline diluent to the nebulizer if required (2.5 ml is a common amount of diluent). Most medications come prediluted with saline.
4. Attach the nebulizer to a source of compressed gas. Oxygen (6 to 8 L/min) can be used, but room air via an air compressor increases the humidity of the inhaled gas because of the water vapor content in room air. Adjust the flow rate until a light mist is created. If too forceful a stream is generated, the medication may be wasted.
5. Attach the corrugated tubing to the nebulizer. Some references place the tubing between the nebulizer and the mouthpiece to allow large droplets to “rain out” into the tubing; this decreases deposition of these droplets on the tongue and may reduce side effects. Other sources place the tubing on the opposite side of the nebulizer to serve as a reservoir.
6. Give the patient the mouthpiece or place the mask on the patient. Emphasize avoiding spillage of the medicine and avoiding wasted medicine due to talking or otherwise interrupting the treatment.
7. Coach the patient in the correct breathing technique to improve the effectiveness of the treatment. Instruct the patient to breathe slowly in and out through the mouthpiece or mask. Keep the lips sealed around the mouthpiece.
8. Tap the sides of the nebulizer occasionally to cause condensation droplets to return to the pool from which it is nebulized.
9. Continue treatment until nebulizer no longer delivers medicine mist or droplets.
10. Reassess breath sounds, pulse rate, oxygen saturation, respiratory rate, and peak flow.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree