Learning outcomes
By the end of this section, you should know how to:
▪ prepare the patient for this procedure
▪ collect and prepare the equipment
▪ assist the medical practitioner during bone marrow aspiration
▪ monitor the patient for the adverse effects of bone marrow aspiration.
Background knowledge required
Revision of the anatomy and physiology of the blood, with special reference to the source and development of the red blood corpuscles
Indications and rationale for bone marrow aspiration
Soft tissue found in the inner cavities of the bones, which is responsible for the formation of blood cells, is known as ‘red marrow’. Bone marrow aspiration is the removal of a sample of this fluid, and may be indicated for the following:
▪ to confirm the diagnosis of some anaemias, leukaemias and lymphomas
▪ to evaluate the effectiveness of treatment during the course of a disease
▪ to identify the source of a pyrexia of unknown origin
▪ to assess a person’s ability to store iron.
Outline of the procedure
Bone marrow aspiration is carried out by a medical practitioner or a specially trained nurse. The procedure may take place as a day patient in an outpatient setting, or as an inpatient in hospital. It is considered best practice to obtain written consent, as bone marrow aspiration is an invasive procedure. The medical practitioner should ensure that the patient has received sufficient information about the procedure to make an informed decision (Department of Health 2001).
Positioning the patient
The position of the patient for the procedure is dependent on the site chosen for aspiration:
Posterior superior iliac crest
This is the preferred site, the patient is positioned in a right or left lateral position with knees flexed.
Anterior superior iliac crest
The patient can be positioned prone or on their side.
The patient is required to lie supine with one pillow under the head.
Sternal aspiration should only be attempted in adults, since there is a higher incidence of complications in infants and children. Care is required to prevent cardiac injury, therefore the iliac crest should be considered as first choice as there are no vital organs near the puncture site.
Tibia
Aspiration of the anteromedial surface of the tibia is performed only in children under 18 months of age. The patient is positioned on their back.
Bone marrow aspiration is an aseptic procedure and takes approximately 20–30 minutes. The patient may be given a sedative prior to the procedure, to help them relax. Following correct hand-washing procedures the medical practitioner will administer a local anaesthetic into the chosen site and then apply sterile gloves. The skin over the aspiration site is cleansed using an antiseptic, a small stab incision is made, and the aspiration needle inserted through the skin and rotated until it penetrates the cortex, or outer covering of the bone, into the red bone marrow cavity.
The needle is specially designed and fitted with an adjustable protective guard to control its level of penetration (Fig. 7.1), thus preventing injury to the underlying vital organs. The stilette of the needle is removed and the syringe attached to the hub of the marrow needle.
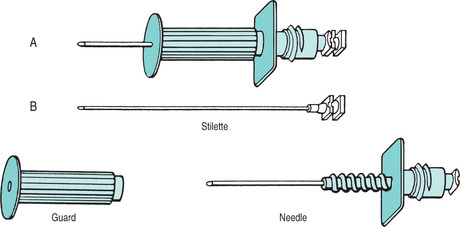 |
| FIGURE 7.1Bone marrow aspiration needle (disposable) showing the adjustable guard A Complete needle B Needle taken apart |
Approximately 2.5 ml of bone marrow is aspirated, if additional marrow is needed the needle is repositioned, and a new syringe attached. The specimen of marrow is transferred from the syringe to the microscopic slides. Following the aspiration, the syringe is disconnected, the stilette replaced and the needle withdrawn. The slides are smeared with a preservative, allowed to dry, and sent to the laboratory for testing.
As the microscope slides are prepared, pressure should be applied to the puncture site until bleeding ceases. The puncture site should be covered with a sterile adhesive dressing.
Serious problems from a bone marrow aspiration are not common, however problems may include:
▪ excessive bleeding from the biopsy site. People with clotting problems may have a higher chance of this occurring
▪ infection of the bone at the biopsy site
▪ injury to the heart, lung or major blood vessel if the sample is taken from the sternum. A cardiac tamponade can develop when bleeding from a ruptured blood vessel in the myocardium causes pressure on the pericardial sac (Lewis et al 2004).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


