Cellulitis, 682.9
Dermatitis medicamentosa (drug eruption), 693.0
Herpes zoster (shingles), 053.9
Integumentary disorders, 709.9
I. History
A. Presenting complaint
1. Presenting lesion
2. Onset and progression
B. Past and present systemic disorders
C. Family history
1. Blood relatives (genetic or infectious diseases)
2. Are household contacts affected similarly?—Include information regarding pets in the home environment.
D. Drug history (Table 68-1)
1. Question carefully about medications that have been taken within the past month, as well as commonplace routine medications taken on a regular basis that otherwise may be forgotten.
2. Question about which treatments have already been tried, including over-the-counter remedies, and how successful they were.
| Disorder | Drugs |
|---|---|
| Acne | Corticosteroids, isoniazid |
| Bullous lesions | Barbiturate overdose, penicillamine, sulfonamides |
| Eczematous dermatitis | Antibiotics, methyldopa, phenylbutazone, sulfonamides |
| Erythema multiforme | Barbiturates, hydantoins, penicillin, salicylates, sulfonamides, sulfonylureas |
| Erythema nodosum | Contraceptives, sulfonamides |
| Exfoliative dermatitis | Allopurinol, gold, indomethacin, phenylbutazone |
| Lichenoid eruption | Chloroquine, chlorpropamide, mepacrine, quinidine, quinine, thiazides |
| Photosensitivity | Amiodarone, nalidixic acid, sulfonamides, tetracycline |
| Pigmentation | Chloroquine, heavy metals, mepacrine |
| Psoriasiform rash | Gold, methyldopa |
| Purpura | Cytotoxic drugs, meprobamate, quinidine, quinine |
| Systemic lupus erythematosus | Hydralazine, isoniazid, penicillamine, procainamide |
| Urticaria | Aspirin, imipramine, penicillin, serum, toxoid, vaccines |
E. Occupation and leisure activities, in particular any activities that have been adopted recently or near the time of onset of symptoms
F. Travel—within or outside of the country
II. Morphology
A. Skin lesions are categorized according to the configuration of the lesions or identifying characteristics (Fig. 68-1).
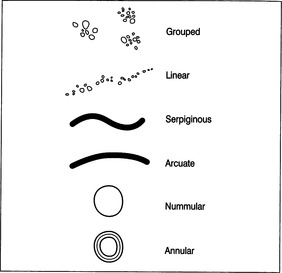 |
| FIGURE 68-1Various configurations of skin lesions.(From Mir MA: Atlas of clinical skills, Philadelphia, 1997, W.B. Saunders.) |
B. Various terms are applied to skin changes (Table 68-2).
| Bulla | Large vesicle, more than 0.5 cm in diameter |
| Comedone | Plug of keratin and sebum wedged in a dilated pilosebaceous orifice |
| Crust | Accumulated dried exudate |
| Excoriation | Superficial (epidermal) abrasion caused by scratching |
| Lichenification | Area of increased epidermal thickening with exaggerated skin markings, caused by constant rubbing (e.g., atopic eczema) |
| Macule | Flat, circumscribed area of skin discoloration |
| Nodule | Circumscribed, palpable area of the skin that is more than 0.5 cm diameter and appears in part or wholly within the dermis |
| Papule | Circumscribed, palpable elevation of the skin, less than 1 cm in diameter |
| Patch | Large macule, more than 2 cm in diameter |
| Plaque | Circumscribed, disk-shaped elevated area of the skin, more than 1 cm |
| Purpura | Extravasation of blood in the skin that causes macules and (about 2 mm in diameter); larger spots are called ecchymoses |
| Pustule | Visible collection of pus |
| Scales | Visible and often palpable, whitish flakes due to aggregation of dried/diseased shed epidermal cells |
| Scar | Area of fibrous tissue that replaces the lost epidermis |
| Stria | Streaklike, linear, atrophic, pink, purple, or white lesion caused by stretching of the skin |
| Telangiectasia | Visible dilatation of a small cutaneous blood vessel |
| Ulcer | Loss of epidermis and part or whole of the dermis |
| Vesicle | Visible accumulation of fluid beneath the epidermis (less than 0.5 cm in diameter) |
| Weal | Circumscribed, elevated area of cutaneous edema |
C. Skin eruptions or exanthems are divided into three groups
2. Vesicular or bullous lesions
3. Pustular, petechial, or purpuric lesions
4. Figure 68-2 describes various types and shapes of skin lesions.
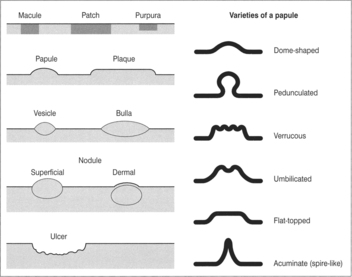 |
| FIGURE 68-2Various types and shapes of skin lesions.(From Mir MA: Atlas of clinical skills, Philadelphia, 1997, W.B. Saunders.) |
III. Physical examination
A. It is necessary to examine the entire skin, including nails, scalp, palms, soles, and mucous membranes. The patient is examined undressed in an area with good lighting.
C. Identify morphology, configuration, and distribution of any lesions.
D. Use a magnifying glass to view the surfaces of lesions.
E. Examine for secondary changes of skin lesions: comedones, crusting, excoriation, lichenification, scales, scarring.
DERMATITIS MEDICAMENTOSA (DRUG ERUPTION)
I. Definition
A. Also referred to as adverse cutaneous drug reaction
1. Drug eruptions are caused by immunologic or nonimmunologic mechanisms.
2. Eruptions are provoked by systemic or topical administration of a drug.
B. True allergic drug reactions involve prior exposure to the offending drug and require minimal doses to elicit a reaction.
C. Most allergic reactions have skin manifestations.
II. Incidence/predisposing factors
A. See Table 68-1 for reactions associated with particular drug classes.
B. Classification of adverse cutaneous drug reactions
1. Type I—immediate-type immunologic reaction
a. Immunoglobulin (Ig)E mediated
b. Manifested by urticaria and angioedema of skin or mucosa, edema of other organs, and fall in blood pressure (anaphylactic shock)
2. Type II—cytotoxic reaction
a. Drug or causative agent causes lysis of cells such as platelets or leukocytes, or may, by combination with another drug, produce antibodies (immune complexes) that cause lysis or phagocytosis.
3. Type III—serum sickness, drug-induced vasculitis
a. IgG or, less commonly, IgM antibodies are formed against a drug.
b. Manifested by vasculitis, urticaria-like lesion, arthritis, nephritis, alveolitis, hemolytic anemia, thrombocytopenia, and agranulocytosis
4. Type IV—morbilliform (exanthematous) reaction
a. Cell-mediated immune reaction
b. Sensitized lymphocytes react with the drug, releasing cytokines that bring on a cutaneous inflammatory response.
C. Beta-lactams cause the most common allergic skin reactions.
D. Cephalosporins are associated with reactions in 5% to 15% of penicillin-sensitive patients. Third-generation cephalosporins may be less likely to react than first-generation cephalosporins.
E. “Red man” syndrome associated with vancomycin often responds to slowing of infusion rate.
F. ACE inhibitors are associated with chronic cough and angioedema.
G. Beta blockers can precipitate asthma and should not be given to patients at risk for anaphylaxis because beta blockers may block the action of epinephrine.
I. Radiocontrast media and opioids may simulate mast cell histamine release through a non–IgE-mediated mechanism. Only 20% to 30% have repeat reactions.
III. Subjective findings
A. Abrupt onset
B. Usually with bright confluent erythema
C. May have facial edema or central facial involvement
D. May have swelling of the tongue
E. Often with itching
F. May have fever
G. Skin reaction usually symmetric in distribution
H. May have arthralgias or symptoms of arthritis
I. May have accompanying shortness of breath, wheezing, hypotension
J. False history of drug reaction may be due to patient misunderstanding, such as
1. Specific drug reactions are not inherited.
2. Undetermined reactions of childhood may not be reproducible in adult life.
3. Common adverse effects such as nausea or weight gain may be mistaken for allergy.
4. When a true allergic reaction has not actually occurred, the patient’s records should be corrected.
K. A detailed, accurate account of a drug reaction should be documented.
IV. Physical findings
A. Bright confluent erythema is the common presentation.
B. Urticaria and angioedema imply mast cell degranulation. If an IgE-mediated mechanism was the cause, a repeat reaction is likely.
C. May have morbilliform (exanthematous) eruptions—the most common type of cutaneous drug reaction. May develop exfoliative dermatitis, especially if drug is not discontinued
D. May have eczematoid rash
E. May have photodermatitis
F. Reactions involving other systems may include
1. Hemolytic anemia
2. Liver or kidney dysfunction
3. Serum sickness (rash, fever, malaise)
V. Laboratory/diagnostic findings
A. Diagnosis is usually made on the basis of clinical findings alone.
B. Routinely ordered blood work is usually of no value in diagnosis.
C. Eosinophil count greater than 1000 per microliter: lymphocytosis with atypical lymphocytes
D. Consider ordering the following:
1. Liver function tests (not usually done)
2. Skin biopsies (may be of value in confirming diagnosis)
4. Patch and photo testing (may reveal contact or photodermatitis—not commonly done)
5. Challenge dosing, preferably orally, if an anaphylactic reaction seems unlikely.
6. Serum level and hepatic/renal monitoring when indicated
VI. Management
A. Withdrawal of the drug may be the only treatment necessary.
B. Treatment is aimed at symptoms.
C. Epinephrine 1:1000, 0.3-0.5 ml given subcutaneously, may provide rapid temporary relief from urticaria and angioedema. Dosage may be repeated after 20 minutes. In severe cases, epinephrine 1:1000, 0.5-1 ml given intravenously or subcutaneously, may be used as an emergency measure.
D. Give oral or IV antihistamine. Diphenhydramine (Benadryl), 25-50 mg, may follow epinephrine.
E. Corticosteroids are generally not indicated if the offending agent is discontinued. When indicated, prednisone, 70 mg, tapered by 10 mg or 5 mg daily over 1 to 2 weeks
F. Wheezing may be treated with the use of inhaled bronchodilators.
G. Treatment of dermatitis varies according to the stage of presentation, ranging from topical application comfort measures to hospitalization for extensive blistering eruptions, such as toxic epidermal necrolysis, which may result in erosions and superficial ulcerations that require hospitalization as for burns.
H. For more serious anaphylactoid reactions, see Chapter 75, Management of the Patient in Shock.
I. Morbilliform rashes and serum sickness may require 1 to 2 weeks of treatment with antihistamines or systemic corticosteroids.
J. Corticosteroid use in Stevens-Johnson syndrome is controversial. Extensive blistering that results in erosions or ulcerations requires hospital admission and care similar to that provided for burn patients.
K. Prevention of drug reactions
1. Use alternative drug in a different class.
2. Premedication does not prevent true IgE-mediated reactions but may be successful for non–IgE-mediated reactions, for example,
a. Prednisone 50 mg at 13 hours, 7 hours, and 1 hour before radiocontrast media
b. Diphenhydramine 1 mg/kg 1 hour before drug
c. Some sources indicate cimetidine 4 mg/kg or ephedrine 25 mg 1 hour before
3. Desensitization may be successful but may be temporary.
L. Follow-up
1. Patient education: A written list of drugs most likely to cause problems should be given to the patient.
3. Medical warning bracelet should be worn by the patient who has a history of life-threatening reactions, and he or she should have an epinephrine injection kit.
CELLULITIS
I. Definition
A. Acute infection of the skin and subcutaneous tissues
B. Infection of the deeper layers of the skin
II. General comments/incidence/predisposing factors




A. A break in the integrity of the skin almost always precedes this infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
