Section 6 Pharmacology
6.1 Drugs and the law
The Medicines Act 1968
The Medicines and Healthcare Regulatory Agency (MHRA) was set up in 2003 to ensure that medicines and medical devises work and are safe. They have a website at www.mhra.gov.uk. They assess the quality and safety of medicines and authorize their sale in the UK.
The Misuse of Drugs Act 1971
The Care Quality Commission (CQC) is now responsible for ensuring that healthcare providers are creating a safer environment for the management of controlled drugs and further information is available on their website at www.cqc.org.uk.
In hospitals there are regulations controlling these drugs:
 They are stored in a double-locked cupboard of their own.
They are stored in a double-locked cupboard of their own.
 The key must be carried by the nurse in charge.
The key must be carried by the nurse in charge.
 There is a special Controlled Drugs Order Book for those drugs in frequent use which can be kept as stock. The sister in charge must sign each order.
There is a special Controlled Drugs Order Book for those drugs in frequent use which can be kept as stock. The sister in charge must sign each order.
 Each administration of these drugs has to be recorded in the Controlled Drug Book with the patient’s name, the dose of the drug, the time it was given and the signature of the nurse who administers the drug and another who has checked all these details.
Each administration of these drugs has to be recorded in the Controlled Drug Book with the patient’s name, the dose of the drug, the time it was given and the signature of the nurse who administers the drug and another who has checked all these details.
Schedule 2 includes drugs subject to full controlled drug requirements. Examples include:
6.2 Medicines management
In 2007, The Nursing and Midwifery Council (NMC) published their ‘Standards for Medicines Management’. These have been updated in 2010 and are available on the NMC website (www.nmc-uk.org). The standards replaced the NMC’s ‘Guidelines for the Administration of Medicines’ (2004), but do continue to emphasize the importance of the trained nurse using thought and professional judgement when administering medication and so going beyond the mechanistic delivery of the prescribed dose on the treatment sheet. They describe the importance of using local expertise regarding medicines management and refer to the importance of the pharmacist in the role of advisor.
The administration of medicines
The ‘five rights’ act as a simple and basic reminder of some of the essential points of care:
Who can administer medicines in a hospital setting?
Important points
 The nurse should never administer a medication without knowing its therapeutic use, normal dosage, side-effects, precautions and contra-indications. There should always be a copy of the British National Formulary (BNF) available when medicines are administered so that any unfamiliar drugs can be looked up.
The nurse should never administer a medication without knowing its therapeutic use, normal dosage, side-effects, precautions and contra-indications. There should always be a copy of the British National Formulary (BNF) available when medicines are administered so that any unfamiliar drugs can be looked up.
 The nurse must be certain of the identity of the patient to whom the medication is to be administered and should also have knowledge of his planned care.
The nurse must be certain of the identity of the patient to whom the medication is to be administered and should also have knowledge of his planned care.
 Always check that the patient is not allergic to the medicine before administration.
Always check that the patient is not allergic to the medicine before administration.
 The prescription must be very clear and legible. Doctors are asked to print the drug name and in hospital must always use the generic name of the medication and not the trade name. The label on the medicine dispensed should be clear and unambiguous.
The prescription must be very clear and legible. Doctors are asked to print the drug name and in hospital must always use the generic name of the medication and not the trade name. The label on the medicine dispensed should be clear and unambiguous.
 The expiry date of the medicine (if available) should be checked.
The expiry date of the medicine (if available) should be checked.
 If there is any ambiguity or query regarding the drug, the dose or the route of administration, which should all be very clear on the prescription sheet, the nurse must refuse to administer the medication and should contact the prescriber.
If there is any ambiguity or query regarding the drug, the dose or the route of administration, which should all be very clear on the prescription sheet, the nurse must refuse to administer the medication and should contact the prescriber.
 If any contraindications to the prescribed medicine are discovered or where the patient develops a reaction the prescriber should be contacted without delay.
If any contraindications to the prescribed medicine are discovered or where the patient develops a reaction the prescriber should be contacted without delay.
 When a medication has been administered, this must be recorded at the time in a clear and accurate manner and with a signature which is legible. If the patient refuses his medication this should also be recorded and the nurse in charge should assess the situation and contact the prescriber.
When a medication has been administered, this must be recorded at the time in a clear and accurate manner and with a signature which is legible. If the patient refuses his medication this should also be recorded and the nurse in charge should assess the situation and contact the prescriber.
 A medicine must never be charted before it is given. When you sign for that drug you are saying that the client has actually taken it.
A medicine must never be charted before it is given. When you sign for that drug you are saying that the client has actually taken it.
 Always check that the client understands the medication that s/he is receiving and is aware of any important side-effects. Emphasize the importance of the treatment and explain its mode of action in simple terms.
Always check that the client understands the medication that s/he is receiving and is aware of any important side-effects. Emphasize the importance of the treatment and explain its mode of action in simple terms.
 If an error is made in the administration of a medicine, this should immediately be reported to the nurse in charge, who will inform the prescriber.
If an error is made in the administration of a medicine, this should immediately be reported to the nurse in charge, who will inform the prescriber.
 Evaluate the action of the prescribed medication and record any positive or negative effects, informing the prescriber of these.
Evaluate the action of the prescribed medication and record any positive or negative effects, informing the prescriber of these.
6.4 Pharmacology in practice
Drug administration
The aims of administration are:
 To establish optimal drug concentration at the target site.
To establish optimal drug concentration at the target site.
 To maintain optimal concentration for the required period of time.
To maintain optimal concentration for the required period of time.
 To minimize adverse drug reactions due to general distribution.
To minimize adverse drug reactions due to general distribution.
Routes of administration
Oral
The absorption of oral medication is influenced by many factors.
Laxatives also decrease absorption.
The concentration of a drug in the intestine depends on the:
Rectal
Steroid enemas are administered for local action on an inflamed bowel in ulcerative colitis.
The rectal route is especially useful when:
 A drug is irritant to the stomach mucosa.
A drug is irritant to the stomach mucosa.
 The patient is vomiting or nauseated.
The patient is vomiting or nauseated.
 There is difficulty in swallowing.
There is difficulty in swallowing.
Examples of drugs given rectally are:
Topical application
This is for local effect on the skin and mucous membranes:
 Creams – these are emulsions of oil and water that are well absorbed into the skin and may be used for dry and scaly skin or as the base for other drugs, such as steroids in eczema.
Creams – these are emulsions of oil and water that are well absorbed into the skin and may be used for dry and scaly skin or as the base for other drugs, such as steroids in eczema.
 Eye drops – sterile preparations for instillation into the eye. This could be for an infection, e.g. chloramphenicol drops, or to have an effect on the pupil or the drainage system.
Eye drops – sterile preparations for instillation into the eye. This could be for an infection, e.g. chloramphenicol drops, or to have an effect on the pupil or the drainage system.
 Ear drops – these are for application to the external auditory meatus, e.g. Cerumol® which helps to dissolve wax in the ear.
Ear drops – these are for application to the external auditory meatus, e.g. Cerumol® which helps to dissolve wax in the ear.
Inhalation
The drug may be administered as:
 An aerosol, as in salbutamol inhalers used to treat asthma. Aerosols contain particles dispersed in a gas and small enough to remain suspended for a long time.
An aerosol, as in salbutamol inhalers used to treat asthma. Aerosols contain particles dispersed in a gas and small enough to remain suspended for a long time.
 A powder dispensed from a rotary inhaler as in sodium cromoglicate (Intal) for the treatment of asthma.
A powder dispensed from a rotary inhaler as in sodium cromoglicate (Intal) for the treatment of asthma.
 A nebulizer – the machine converts a solution of the drug into an aerosol. These are used in respiratory conditions, e.g. salbutamol for asthma.
A nebulizer – the machine converts a solution of the drug into an aerosol. These are used in respiratory conditions, e.g. salbutamol for asthma.
Injection
 Intradermally – into the skin. Used for allergy testing and diagnostic tests. Less than 0.1 ml may be given.
Intradermally – into the skin. Used for allergy testing and diagnostic tests. Less than 0.1 ml may be given.
 Subcutaneously – under the skin. Used for insulin and heparin administration where slow and steady release is needed. Up to 2 ml may be administered. Sites for subcutaneous injection are shown in Figure 6.1. Absorption of the drug does depend on local blood supply and may be more rapid with exercise. The needle was traditionally inserted at a 45º angle but with the advent of shorter specialist needles the recommendation for insulin injection is an angle of 90º.
Subcutaneously – under the skin. Used for insulin and heparin administration where slow and steady release is needed. Up to 2 ml may be administered. Sites for subcutaneous injection are shown in Figure 6.1. Absorption of the drug does depend on local blood supply and may be more rapid with exercise. The needle was traditionally inserted at a 45º angle but with the advent of shorter specialist needles the recommendation for insulin injection is an angle of 90º.
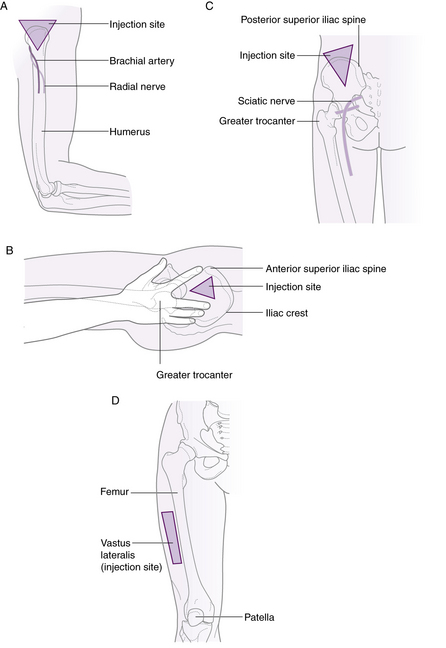
 Intramuscularly – into a muscle. Up to 4 ml may be given into well-developed muscle. The sites used are shown in Figure 6.2 and detailed below. Again, absorption is variable dependent on the site and the state of the circulatory system.
Intramuscularly – into a muscle. Up to 4 ml may be given into well-developed muscle. The sites used are shown in Figure 6.2 and detailed below. Again, absorption is variable dependent on the site and the state of the circulatory system.
 Intravenously – into the venous circulation. This route may only be used by doctors and registered nurses who have done a course in intravenous drug administration.
Intravenously – into the venous circulation. This route may only be used by doctors and registered nurses who have done a course in intravenous drug administration.
 Intrathecally – into the spinal theca.
Intrathecally – into the spinal theca.
 Intraosseous – into the bone marrow cavity. A route more commonly used in paediatrics but also in adults when intravenous access cannot be obtained.
Intraosseous – into the bone marrow cavity. A route more commonly used in paediatrics but also in adults when intravenous access cannot be obtained.
 Into various body cavities, e.g. the peritoneum and the pleura.
Into various body cavities, e.g. the peritoneum and the pleura.
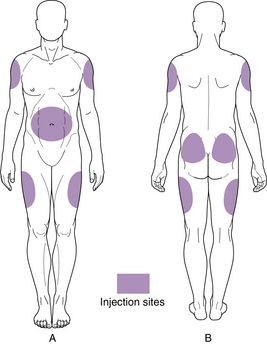
Fig. 6.1 Sites used for subcutaneous injection. A. Anterior aspect. B. Posterior aspect.
From Jamieson/Clinical Nursing Practices, 3rd edn, reproduced with permission.
Some advantages of intravenous administration
 The drug is delivered into the bloodstream and so is able to act immediately.
The drug is delivered into the bloodstream and so is able to act immediately.
 There is no reliance on absorption and the whole dose of the drug reaches the bloodstream, enabling better calculation of the amount the patient actually receives.
There is no reliance on absorption and the whole dose of the drug reaches the bloodstream, enabling better calculation of the amount the patient actually receives.
 A continuous infusion allows the rate of administration to be controlled and the action of the drug thus modified.
A continuous infusion allows the rate of administration to be controlled and the action of the drug thus modified.