Section 6 Drug administration
6.1 Pharmacokinetics and pharmacodynamics
Pharmacokinetic processes
Absorption
 Drugs absorbed from the GIT enter the portal circulation and some are extensively metabolized as they pass through the liver.
Drugs absorbed from the GIT enter the portal circulation and some are extensively metabolized as they pass through the liver.
 Drugs that are lipid soluble are readily absorbed orally and rapidly distributed throughout the body.
Drugs that are lipid soluble are readily absorbed orally and rapidly distributed throughout the body.
 Many drugs are bound to albumin and equilibrium forms between the bound and free drug in the plasma. The drug that is bound to albumin does not exert a pharmacological action.
Many drugs are bound to albumin and equilibrium forms between the bound and free drug in the plasma. The drug that is bound to albumin does not exert a pharmacological action.
 Bioavailability is the fraction of the administered dose that reaches the systemic circulation – 100% in drugs administered IV.
Bioavailability is the fraction of the administered dose that reaches the systemic circulation – 100% in drugs administered IV.
Metabolism
1. Phase 1 reaction – the biotransformation of the drug – oxidations are the most common reactions and these are catalysed by mixed function oxidases.
2. Phase II reactions – drugs from phase I cannot be excreted efficiently by the kidneys and are made more hydrophilic by conjugation with compounds in the liver.
Concomitant drug administration may influence metabolism, for example:
 phenytoin can induce liver enzymes by increasing the metabolism of other drugs
phenytoin can induce liver enzymes by increasing the metabolism of other drugs
 cimetidine can inhibit liver enzymes by reducing metabolism.
cimetidine can inhibit liver enzymes by reducing metabolism.
These can have serious consequences if the patient is already on other drug therapies.
Other factors can affect drug metabolism:
 age (including infants/children)
age (including infants/children)
 immaturity of drug-metabolizing enzymes in neonates and infants
immaturity of drug-metabolizing enzymes in neonates and infants
 disease (impaired liver function, dose reduction may be necessary for drugs metabolized in the liver), e.g. chlormethiazole
disease (impaired liver function, dose reduction may be necessary for drugs metabolized in the liver), e.g. chlormethiazole
Pharmacodynamics
 Pharmacological responses are initiated by the molecular interactions of drugs with cells, tissues or other body constituents.
Pharmacological responses are initiated by the molecular interactions of drugs with cells, tissues or other body constituents.
 Drug molecules must exert some chemical influence on one or more cellular constituents to produce a pharmacological response.
Drug molecules must exert some chemical influence on one or more cellular constituents to produce a pharmacological response.
 To affect functioning of cellular molecules, the drug must approach the molecules closely.
To affect functioning of cellular molecules, the drug must approach the molecules closely.
 Another requirement is that the drug must have some sort of non-uniform distribution within the body or the chance of interaction if the drug molecules are distributed at random would be negligible. This means that a drug must bind in some way to constituents of the cell to produce an effect.
Another requirement is that the drug must have some sort of non-uniform distribution within the body or the chance of interaction if the drug molecules are distributed at random would be negligible. This means that a drug must bind in some way to constituents of the cell to produce an effect.
 For most drugs the site of action is at a specific biological molecule – the receptor. A receptor is the primary site of action of a drug.
For most drugs the site of action is at a specific biological molecule – the receptor. A receptor is the primary site of action of a drug.
 Various types of receptor exist, and each responds to a different chemical or hormone, e.g. histamine, acetylcholine, epinephrine (adrenaline) and dopamine.
Various types of receptor exist, and each responds to a different chemical or hormone, e.g. histamine, acetylcholine, epinephrine (adrenaline) and dopamine.
 Many endogenous hormones, neurotransmitters and other mediators exert their effects as a result of high affinity binding or specific macromolecular protein or glycoprotein receptors in plasma membranes or cell cytoplasm.
Many endogenous hormones, neurotransmitters and other mediators exert their effects as a result of high affinity binding or specific macromolecular protein or glycoprotein receptors in plasma membranes or cell cytoplasm.
 When these receptors are bound to a certain chemical, this directs a change to occur in the cell, which then alters an activity of the cell.
When these receptors are bound to a certain chemical, this directs a change to occur in the cell, which then alters an activity of the cell.
The commonest ways in which drugs produce their effects
 Ion channels – physical blocking of channel by the drug molecule – sodium channel blocking by local anaesthetics or by binding to accessory sites to facilitate opening of channels.
Ion channels – physical blocking of channel by the drug molecule – sodium channel blocking by local anaesthetics or by binding to accessory sites to facilitate opening of channels.
 Enzymes – many drugs are targeted in this way:
Enzymes – many drugs are targeted in this way:
 Transport proteins – drugs may interfere with the uptake of ions or small molecules across the cell membrane:
Transport proteins – drugs may interfere with the uptake of ions or small molecules across the cell membrane:
 Other cellular macromolecules – these do not involve regulatory proteins:
Other cellular macromolecules – these do not involve regulatory proteins:
 Agonists – these interact with a receptor mimicking the effect of a natural mediator. Epinephrine (adrenaline) is a beta-receptor agonist, which stimulates the cardiac beta-receptors and increases heart rate.
Agonists – these interact with a receptor mimicking the effect of a natural mediator. Epinephrine (adrenaline) is a beta-receptor agonist, which stimulates the cardiac beta-receptors and increases heart rate.
 Partial agonists – the maximal response falls short of the full response block access of the natural agonist, e.g. pindolol, oxprenolol beta blockers, which are partial agonists.
Partial agonists – the maximal response falls short of the full response block access of the natural agonist, e.g. pindolol, oxprenolol beta blockers, which are partial agonists.
 Antagonists block a receptor to prevent such an effect. Atenolol is a beta-receptor antagonist that slows heart rate by blocking the cardiac beta-receptors and reducing physiological stimulation. They are selective but not specific (they act on more than one receptor and produce side effects). Amitriptyline (tricyclic antidepressant) blocks cholinergic and histamine receptors, which leads to dry mouth, blurred vision, constipation and drowsiness.
Antagonists block a receptor to prevent such an effect. Atenolol is a beta-receptor antagonist that slows heart rate by blocking the cardiac beta-receptors and reducing physiological stimulation. They are selective but not specific (they act on more than one receptor and produce side effects). Amitriptyline (tricyclic antidepressant) blocks cholinergic and histamine receptors, which leads to dry mouth, blurred vision, constipation and drowsiness.
Potency of drugs
 If a drug is potent it produces effects at low concentration.
If a drug is potent it produces effects at low concentration.
 If a drug has a high potency it is a consequence of high affinity for a specific receptor.
If a drug has a high potency it is a consequence of high affinity for a specific receptor.
 Affinity is the tendency to bind to receptors.
Affinity is the tendency to bind to receptors.
 Efficacy is the ability once bound, to initiate changes, which lead to effects.
Efficacy is the ability once bound, to initiate changes, which lead to effects.
 If a drug is specific small changes in drug structure lead to profound changes in potency or causes a change from agonist to antagonist:
If a drug is specific small changes in drug structure lead to profound changes in potency or causes a change from agonist to antagonist:
 Potency is independent of efficacy and efficacy is usually more important than potency when selecting a drug for clinical use.
Potency is independent of efficacy and efficacy is usually more important than potency when selecting a drug for clinical use.
 The lower the potency of a drug and the higher the dose needed, the more likely that sites of action other than the primary one will assume significance:
The lower the potency of a drug and the higher the dose needed, the more likely that sites of action other than the primary one will assume significance:
Mode of action
If the basic mode of action of a drug is via a receptor then it is likely that:
 it will have biological specificity and may produce opposite effects on apparently similar tissue type
it will have biological specificity and may produce opposite effects on apparently similar tissue type
 it will have chemical specificity and changes in the chemical structure of a drug molecule may have a large or small effect on its pharmacological activity
it will have chemical specificity and changes in the chemical structure of a drug molecule may have a large or small effect on its pharmacological activity
 specific antagonists will abolish the effects of the drug on the tissue
specific antagonists will abolish the effects of the drug on the tissue
 if plasma concentration of the drug is too high (outside the therapeutic range) toxicity will occur
if plasma concentration of the drug is too high (outside the therapeutic range) toxicity will occur
 if plasma concentration is too low treatment will fail
if plasma concentration is too low treatment will fail
 the aim of treatment is to keep the plasma concentration within the therapeutic range via blood levels.
the aim of treatment is to keep the plasma concentration within the therapeutic range via blood levels.
Drug interactions
Drugs are chemicals and may interact with one another. When this happens, a drug’s action may be:
The therapeutic action of one drug can interfere with the therapeutic action of another.
Combinations of drugs must be carefully considered to avoid drug interactions.
As the number of medications prescribed for a patient increases (polypharmacy) so does the potential for drug interactions. With so many drugs given at the same time and so many drugs available, it is impossible to predict the interactions that can occur. Any adverse reaction needs to be reported to the appropriate authorities. The British National Formulary (BNF) and the BNF for children website (www.bnf.org/bnf/) contain lists of known interactions, and these should always be consulted before drug mixtures are administered. Some produce minor problems, others can be fatal. The types of drug interactions that occur are:
 outside the body – generally due to storage conditions, too much light, oxygen or moisture, interactions with containers whereby the chemicals contained within the drug are prone to degradation
outside the body – generally due to storage conditions, too much light, oxygen or moisture, interactions with containers whereby the chemicals contained within the drug are prone to degradation
 in the GIT – some food chemicals may react with drugs
in the GIT – some food chemicals may react with drugs
 after absorption – where the most known interactions take place, usually when more than one drug is administered concurrently.
after absorption – where the most known interactions take place, usually when more than one drug is administered concurrently.
Drug calculations
The following are some of the drug calculation formulae that may help you in this role:
Ampicillin 500 mg in diluted in 10 ml, you require 200 mg
Epinephrine comes in strengths of 1:1000 (1 mg/ml) and 1:10 000 (10 mg/ml)
(i) If you require 1.6 mg of 1:1000 strength epinephrine, use the formula
(ii) If you require 2.5 mg of 1:10 000 strength epinephrine, use the formula
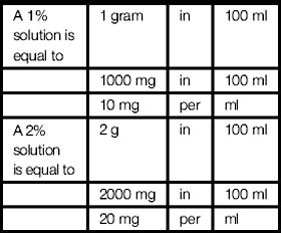
Lidocaine comes in either a 1% solution or a 2% solution; this means that:
There are other drugs used for infusion such as dopamine, epinephrine (adrenaline), dobutamine, noradrenaline (norepinephrine), which require to be calculated in μg/kg/min.
Nurse prescribing
1. The majority of patients continue to receive medicine on an individual patient basis.
2. The current prescribing authority of doctors, dentists, and certain nurses (in respect of a limited list of medicines) continues.
3. New groups of professionals would be able to apply for authority to prescribe in specific clinical areas, where this would improve patient care and patient safety could be assured.
6.2 Medicines management
Safe use of medicines
This includes the clinical, cost effective and safe use of medicines to ensure patients get the maximum benefit from the medicines they need, while at the same time minimizing potential harm or side effects of the drug (www.mhra.gov.uk).
Right medication – check the name of medication against the prescription.
Right patient – check the name against the prescription and verify with parent/carer.
Right dose – check that the dose is correct for the age of the child.
Right route – check that the route is correct for the child and that the correct medication has been prescribed.
Right time and frequency – check that time and frequency of the drug is correct for the child.
The key contributors to the management of medicines are:
The nurses’ role in medicines management:
 interpretation of prescription
interpretation of prescription
 administering the drug prescribed
administering the drug prescribed
 communicating with the child and family, other health care professionals, e.g. doctors and pharmacists
communicating with the child and family, other health care professionals, e.g. doctors and pharmacists
 providing information about the drug to the family, e.g. action and side effects, when to take it
providing information about the drug to the family, e.g. action and side effects, when to take it
 teaching and support for the patient, e.g. being a patient advocate
teaching and support for the patient, e.g. being a patient advocate
 anticipate any potential side effects
anticipate any potential side effects
 monitor the drug for effectiveness, the patient’s response to the medication
monitor the drug for effectiveness, the patient’s response to the medication
 evaluate and review the response to the drug treatment e.g. blood pressure, nausea
evaluate and review the response to the drug treatment e.g. blood pressure, nausea
 record the administration of the drug
record the administration of the drug
 report any changes in the child after administration of the drug
report any changes in the child after administration of the drug
The key priorities influencing and directing medicines management are:
 National standards framework (NSF) – these are national standards for key conditions and diseases, which are central to improving quality of services to patients.
National standards framework (NSF) – these are national standards for key conditions and diseases, which are central to improving quality of services to patients.
 Management of medicines – a resource to support implementation of the wider aspects of medicines management for the NSFs for diabetes, renal services and long-term conditions.
Management of medicines – a resource to support implementation of the wider aspects of medicines management for the NSFs for diabetes, renal services and long-term conditions.
 National Institute for Clinical Excellence (NICE) – provides patients, health professionals and public with guidance on best practice for some medicines and treatments
National Institute for Clinical Excellence (NICE) – provides patients, health professionals and public with guidance on best practice for some medicines and treatments
 The expert patient programme – NHS-based training initiative that provides people with new skills to manage their condition.
The expert patient programme – NHS-based training initiative that provides people with new skills to manage their condition.
 The medicines partnership programme, which supports patients and professionals to enable patients to be more involved in decisions about their medicines.
The medicines partnership programme, which supports patients and professionals to enable patients to be more involved in decisions about their medicines.
Polypharmacy
The reasons for polypharmacy are:
 multiple pathologies – a child may have more than one condition
multiple pathologies – a child may have more than one condition
 multiple prescribers – patients may see several doctors and nurses each of whom may prescribe
multiple prescribers – patients may see several doctors and nurses each of whom may prescribe
 self medication – some children may take over-the-counter, herbal and homeopathic medicines given by their parents or carers
self medication – some children may take over-the-counter, herbal and homeopathic medicines given by their parents or carers
 misuse – there may be confusion following discharge and patients may continue to take their previous regime as well as the new regime
misuse – there may be confusion following discharge and patients may continue to take their previous regime as well as the new regime
 expectations – many patients (parents) expect to leave a consultation with a prescription in their hand.
expectations – many patients (parents) expect to leave a consultation with a prescription in their hand.
There needs to be improvement in this area of medicines management:
 non-compliance with prescribed medications
non-compliance with prescribed medications
 large quantities of unused medicines returned to pharmacies
large quantities of unused medicines returned to pharmacies
 increase in admissions attributed to adverse drug reactions
increase in admissions attributed to adverse drug reactions
 poor control of chronic conditions despite effective medicines being available
poor control of chronic conditions despite effective medicines being available
 unmet patient and carer needs for information concerning treatment
unmet patient and carer needs for information concerning treatment
 patients not tolerating side effects that affect their quality of life.
patients not tolerating side effects that affect their quality of life.
The nurses’ role in improving medicines management:
 Ensuring treatment is evidence based – using the NICE guidelines to ensure consistence of care, involvement of a nurse specialist or nurse prescriber.
Ensuring treatment is evidence based – using the NICE guidelines to ensure consistence of care, involvement of a nurse specialist or nurse prescriber.
 When treatments are stopped – the nurse needs to co-ordinate care to ensure unwanted medicines are not continued to be prescribed.
When treatments are stopped – the nurse needs to co-ordinate care to ensure unwanted medicines are not continued to be prescribed.
 Identify where under treatment is occurring – children may benefit from additional medicines and identify where under treatment is occurring
Identify where under treatment is occurring – children may benefit from additional medicines and identify where under treatment is occurring
 Managing the introduction of new drugs – nurses need to be involved in decisions regarding new treatments, this will involve examining the evidence of effectiveness, the clinical significance of benefit, advantages over existing treatment and cost-effectiveness.
Managing the introduction of new drugs – nurses need to be involved in decisions regarding new treatments, this will involve examining the evidence of effectiveness, the clinical significance of benefit, advantages over existing treatment and cost-effectiveness.
 Monitoring medicine taking – conducting a medication review, encouraging discussion between the health care professional and the child and parent and offer the an opportunity to ask questions such as:
Monitoring medicine taking – conducting a medication review, encouraging discussion between the health care professional and the child and parent and offer the an opportunity to ask questions such as:
 Treatment review – some people have reported not being asked about their medicines by their doctor or other health care professional.
Treatment review – some people have reported not being asked about their medicines by their doctor or other health care professional.
Concordance
Concordance advocates a partnership approach to medicine prescribing and taking, and suggests:
 It must be recognized that children and parents can make their own decisions about whether or not to take a prescribed treatment.
It must be recognized that children and parents can make their own decisions about whether or not to take a prescribed treatment.
 That it must be acknowledged that well-informed children and parents may decline treatment after learning about the relative benefits and risks.
That it must be acknowledged that well-informed children and parents may decline treatment after learning about the relative benefits and risks.
 That a child/parents’ beliefs about their medicines are likely to be the most important consideration in whether to take their medications or not.
That a child/parents’ beliefs about their medicines are likely to be the most important consideration in whether to take their medications or not.
Compliance
 difficulty in taking the medication
difficulty in taking the medication
 child and parents make a conscious decision not to take the medicine
child and parents make a conscious decision not to take the medicine
 treatment regime is complicated, instructions and purpose of medication unclear
treatment regime is complicated, instructions and purpose of medication unclear
 unpleasant taste, side effects are perceived to be risky
unpleasant taste, side effects are perceived to be risky
 child and parents are having difficulty coming to terms with the diagnosis
child and parents are having difficulty coming to terms with the diagnosis
 certain health beliefs of the family
certain health beliefs of the family
 a child and families support network
a child and families support network
 breakdown in communication between services e.g. hospital and home
breakdown in communication between services e.g. hospital and home
6.3 Classification of drugs used in children
The classification of drugs (Table 6.1) is massive and is thus too huge to do it all justice. The classes of drugs outlined in this section are brief. However, there are many texts (Neal 2004, Galbraith et al 2007, BNF for children updated twice per year) that go into much more detail regarding the drugs used in children. For further information it is recommended that you use these and/or others for more in-depth information.
| Class of drug | Action of drug class |
|---|---|
| Anti-emetic | Nausea, vomiting |
| Anti-coagulant | Prevent or reduce clotting of the blood in blood vessels, e.g. heparin or warfarin |
| Antiplatelet | Decrease platelet aggregation – aspirin and dipyridamole |
| Antihypertensive | Used to reduce blood pressure – examples are beta-adrenergic antagonists (beta blockers) such as atenolol, ACE inhibitors such as captopril, calcium channel blockers, e.g. nifedipine and diuretics such as bendrofluazide |
| Analgesic | Relieves pain |
| Hypnotic | Induces sleep – dependency producing, e.g. triazolam. |
| Anxiolytic | Relieves anxiety – used to alleviate acute and severe anxiety states, e.g. diazepam |
| Anaesthetic | Insensible stimuli – loss of sensation Local anaesthesia – sensory nerve impulses are blocked and the patient remains alert General anaesthesia – loss of consciousness and patient is unaware of and unresponsive to painful stimulation, can be maintained by inhalation of anaesthetic gases |
| Antibiotic | Anti-bacterial: length of treatment depends on the nature of the infection and the response to treatment, e.g. penicillin, ampicillin, erythromycin, metronidazole and vancomycin |
| Antacids | Neutralize the acidity of the gastric juice, given in dyspepsia, gastritis, peptic ulcer and oesophageal reflux |
| Anti-arrhythmic | Given to prevent or reduce cardiac irregularities of rhythm, e.g. digoxin, amiodarone |