Learning outcomes
By the end of this section, you should be able to:
▪ demonstrate an understanding of the rationale for this practice
▪ prepare the patient for this nursing practice
▪ collect and prepare the equipment
▪ measure and record the body temperature at the axilla, in the oral cavity, ear canal or in the rectum, in both a community and a hospital setting.
Background knowledge required
Revision of the anatomy and physiology of the skin in relation to the control of body temperature and the temperature-regulating centre, and of the related body mechanisms associated with heat production and heat loss.
Revision of the anatomy of the area where the temperature is to be measured.
Indications and rationale
Body temperature can be considered as the balance of heat lost from the body and heat gained by the body. Both behavioural and physiological mechanisms maintain core body temperature at 37°C ± 1°C. Abnormal body temperature recordings may be an indication that your patient has an infection, is becoming unwell or is experiencing an abnormal reaction to transfused blood products. The normal range of body temperature is 36–37.5°C, but this may vary, by as much as 0.6°C, according to the site used for measurement and from individual to individual. Factors naturally influencing the patient’s body temperature include the ingestion of fluids and food, hormonal changes, smoking and a number of conditions that interfere with thermoregulation (Neno 2005). It is also important, where possible, to establish your patient’s normal temperature at rest. The following terms are used to describe abnormal temperature ranges:
▪ Mild hypothermia (32–35°C)
▪ Moderate hypothermia (28–32°C)
▪ Severe hypothermia (below 28°C)
▪ Mild pyrexia (depending on your patient’s normal baseline temperature, 37.2–38.9°C)
▪ Hyperthermia (above 40.6°C).
The upper and lower limits of survival are not precisely known but are thought to be a body temperature of 44°C and 27°C respectively.
The recording of body temperature may be required:
▪ to establish a baseline temperature, for example when patients are admitted to the hospital or clinic
▪ to monitor fluctuations in temperature, as may occur during the postoperative period, as temperature fluctuations can indicate developing infection or the presence of a deep venous thrombosis
▪ to monitor the temperature of patients being treated for an infection
▪ to monitor the temperature of patients recovering from hypothermia
▪ to monitor temperature during and following invasive diagnostic procedures.
The frequency of measurement will be dependent upon your patient’s condition and recorded temperature.
 Equipment
Equipment1. Tray
2. Appropriate thermometer, e.g.
—disposable thermometer
—electronic thermometer plus probe and disposable cover
—tympanic thermometer and disposable cover
3. Alcohol-impregnated swabs
4. Watch with a second hand
5. Black pen
6. Observation chart
7. Tissues
8. Receptacle for disposable items.
The nature of this practice means that there is a risk of cross infection if the nurse does not adequately clean the thermometers between different patients. Digital electronic probes as well as tympanic thermometers with sheaths/covers still require cleaning with a swab containing 70% isopropyl after patient use to prevent the spread of infection (Carroll 2000).
Disposable thermometers
A variety of disposable thermometers are available for purchase, two of the more common ones being the chemical dot thermometer and the liquid crystal heat-sensitive synthetic strip (Fig. 6.1). These are for single use only, and the manufacturer’s instructions for use must be followed to ensure an accurate recording. These thermometers tend to be used in a community or domestic setting.
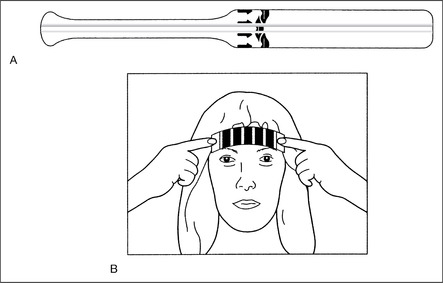 |
| FIGURE 6.1A Disposable chemical dot thermometer B Liquid crystal disposable thermometer |
Electronic thermometers
Electronic thermometers (Fig. 6.2) have replaced traditional mercury glass thermometers as one of the most popular methods of measuring body temperature in hospitals. The electronic thermometer can be used both orally and axillary and some may have a separate probe for rectal use. In addition to this, the electronic thermometer may require that the correct mode of use, e.g. oral or rectal is selected prior to use. Regardless of which site is selected, research indicates that the accuracy of the recording is dependent upon correct probe placement and the cleanliness of the equipment itself (Carroll 2000). The thermometer will automatically give out an audible signal when the temperature has been recorded. As an accountable nurse it is your personal responsibility that you know how to operate equipment and referral to the manufacturer’s instructions is essential.
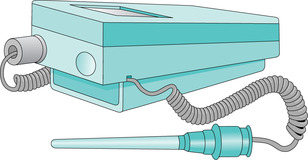 |
| FIGURE 6.2Example of an electronic thermometerFrom Torrance & Semple 1998. Copyright Emap Public Sector Ltd 1998. Reproduced by permission of Nursing TimesEmap Public Sector Ltd |
Now in widespread use, tympanic thermometers (FIGURE 6.3 and FIGURE 6.4) have a probe with a disposable cover that is inserted into the ear canal. They detect infrared energy that is emitted from the tympanic membrane at the end of the ear canal and surrounding tissue, this then being displayed digitally as a temperature reading. Literature suggests that tympanic thermometers represent a more accurate picture of actual body temperature due to the fact that the tympanic membrane shares the same arterial blood supply as the hypothalamus (the temperature regulating centre within the brain; Gallimore 2004).
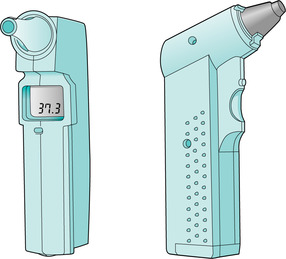 |
| FIGURE 6.3Example of a tympanic thermometerFrom Torrance& Semple 1998. Copyright Emap Public Sector Ltd 1998. Reproduced by permission of Nursing TimesEmap Public Sector Ltd |
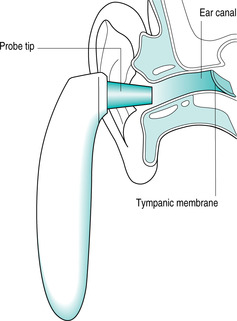 |
| FIGURE 6.4Tympanic membrane thermometer; insertion of probe into ear canalFrom Gallimore 2004. Copyright Emap Public Sector Ltd 2004. Reproduced by permission of Nursing TimesEmap Public Sector Ltd |
The thermometer must be covered by a disposable cover in order to function, and the detection window must be kept clean in order to obtain an accurate result. False readings may arise from incorrect technique, a damaged lens or an inaccurate timing between measurements (Jevon& Jevon 2001).
The patient should be assessed carefully to identify the most appropriate site for temperature measurement, which will ensure an accurate and safe result. Once chosen, the same site should be used for consistent measurement.
Axilla
The axillary site is inappropriate in patients where peripheral circulation is shut down, such as patients with hypothermia (Stevenson 2004). In addition to this the axillary site is the least accurate site in reflecting core body temperature. In elderly patient groups there may be insufficient lean body mass to ensure that the probe is surrounded by skin tissue. The presence of surgical wounds around the site should indicate the avoidance of the site as a means of temperature measurement.




▪ wash the hands and clean thermometer to prevent cross-infection (Carroll 2000)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access

