Chapter 6 Asthma
INTRODUCTION
Asthma is a common disorder of the respiratory system affecting more than 5 million people in the UK (NAC 2001). Although deaths have been declining steadily, asthma still causes much unnecessary suffering for patients. Overall however, asthma care is greatly improved due to significant improvements in treatment.
RELEVANT ANATOMY AND PHYSIOLOGY
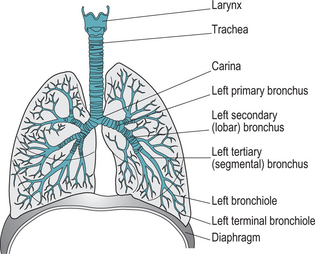
The respiratory system is responsible for providing oxygen to body cells to enable metabolism to take place. It is also responsible for removing carbon dioxide, which is the main waste product of this process. The cardiovascular system is closely associated with this function, as blood is the means by which oxygen and carbon dioxide are transported to and from the cells. Any dysfunction of respiration (or circulation) will result in a disturbance of the homeostatic environment (Box 6.1), which is essential for cellular function. The relevant organs of the respiratory system are shown in Figure 6.1
Ventilation
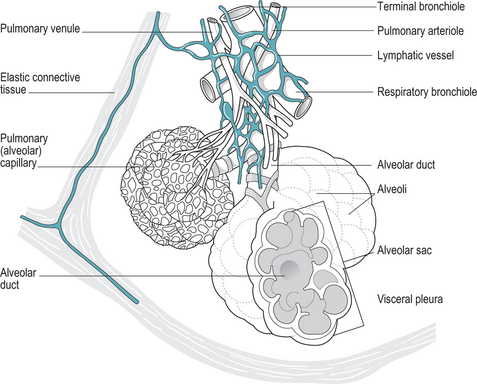
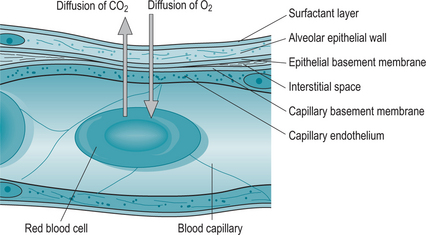
Respiration occurs by the inflation and deflation – ventilation – of the lungs. Air is thus takeninto the alveoli of the lungs where gases are exchanged with the blood circulating in a capillary network surrounding these alveoli (Fig. 6.2). This occurs by simple diffusion across the membranes that separate the lumens of the alveolus and capillary (Fig. 6.3).
Control of ventilation
Factors that influence ventilation:
ASTHMA
Asthma is a chronic inflammatory disease of the airways of the lungs. It is a common condition which is increasing in prevalence around the world (Rees & Kanabar 2000). The term ‘asthma’ comes from an ancient Greek word meaning ‘panting’. The airways become narrowed and inflamed as a result of an inhaled allergen or trigger resulting in cough, wheeze and dyspnoea. An acute asthmatic attack can range in severity from mild shortness of breath to respiratory failure and death (Gutierrez & Peterson 2002). The alveoli themselves are not involved.
Asthma is thought to occur in 15% of children and 6% of adults in the UK (NAC 2001). Asthma that develops in childhood is usually provoked by an identifiable trigger, such as an allergen or by exercise. This is known as extrinsic asthma (Rees & Kanabar 2000). When asthma first develops in adult life, there is often no obvious stimulus other than respiratory tract infection – intrinsic asthma (Box 6.2). Many asthma sufferers however do not fit into either category.
Box 6.2 Occupational asthma
At least 1 in 10 cases of new or recurrent asthma in adults are caused by exposure to substances at work (McDonald 2005). There are many known substances that cause occupational asthma, including isocyanates that are found in many paints, flour and grain dust, animals and latex. Latex is a common product in use in the health services and latex allergies are becoming more common among midwives, as they have regular and prolonged exposure to the substance, mostly in examination gloves. Between 4% and 15% of healthcare workers have a reaction to latex, although this is usually contact dermatitis.
Asthma is commonly considered to go through two primary stages: hyperreactivity and inflammation.
Causes of asthma
The incidence of asthma has risen dramatically worldwide over the past few decades and the reason for this is unclear. Many asthma sufferers also have allergies, but not all people with allergies have asthma. Some forms of asthma do not have an allergic trigger. Evidence to date suggests that asthma is due to a genetic susceptibility along with a variety of environmental triggers such as infection, diet, pollution and allergens (Siddall 2001). There is some evidence to implicate the overuse of antibiotics in early life with the increase in childhood asthma (Shirakawa et al 1997).
Pathophysiology of asthma
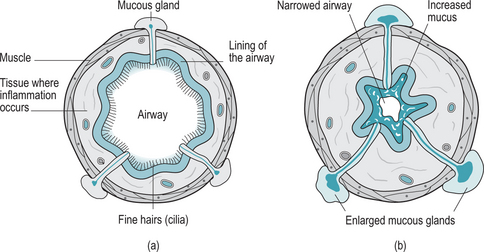
Repeated exposure to an allergen and the initiation of the above process causes permanent pathological changes to the structure and function of the airways resulting in chronic asthma (Fig. 6.4). The epithelial lining of the airways become thinned or destroyed causing increased sensitivity to the allergen on subsequent exposure. The damaged basement membrane of the epithelial layer is replaced with collagen and thus becomes less elastic preventing the airways from responding to the body’s respiratory demands.
This does not solve the problem however. The narrowed airways prevent adequate movement of air out of the lungs however fast the person breathes. Body cells continue to be deprived of oxygen and also suffer from the build up of carbon dioxide causing a respiratory acidosis. Over time, the body cells will be unable to carry out necessary metabolic processes and the individual can become seriously ill. If not quickly treated, the individual will become exhausted with the increased respiratory effort; cells and organs will stop functioning due to lack of oxygen and death may occur.
Signs and symptoms
Between 30–40% of women experience fluctuations in severity associated with their menstrual cycle, which are levelled out by the use of the oral contraceptive suggesting that hormones may have an effect on the condition (Ostrom 2006).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree