Postpartum
Basic Definitions
attachment: The process by which the parent and infant come to love and accept each other
bonding: A process by which parents, over time, form an emotional relationship with their infant
contraception: The intentional prevention of pregnancy during sexual intercourse
involution: Return of the uterus to a nonpregnant state after birth
Transfer From the Recovery Area
At the end of the fourth stage of labor the woman changes from an intrapartum to a postpartum status. She can remain in the same room with the same care provider or be transferred to a postpartum room in the same or another nursing unit and change care providers. This is an excellent time to review intrapartum events and plan appropriate postpartum care for her and her newborn.
Information that must be communicated to the postpartum nurse includes the following:
 Identity of the primary health care provider
Identity of the primary health care provider
 Duration of labor and time of rupture of membranes
Duration of labor and time of rupture of membranes
 Whether labor was induced or augmented
Whether labor was induced or augmented
 Type of birth (vaginal, operative vaginal [forceps- or vacuum-assisted], cesarean)
Type of birth (vaginal, operative vaginal [forceps- or vacuum-assisted], cesarean)
 Intravenous (IV) infusion of any fluids
Intravenous (IV) infusion of any fluids
 Physiologic status since birth
Physiologic status since birth
 Description of fundus, lochia, bladder, and perineum
Description of fundus, lochia, bladder, and perineum
 Human immunodeficiency virus (HIV) test result (if positive)
Human immunodeficiency virus (HIV) test result (if positive)
 Hepatitis B test result (if positive)
Hepatitis B test result (if positive)
 Syphilis (serology) test result (if positive)
Syphilis (serology) test result (if positive)
 Name of pediatric care provider
Name of pediatric care provider
Most of this information is also documented for the nursing staff in the newborn nursery. Other specific information about the newborn that must be communicated to the nursery staff includes the following:
Management of Physical Needs
Assessment
 Vital signs including blood pressure
Vital signs including blood pressure
 Degree of physical discomfort, hunger, thirst
Degree of physical discomfort, hunger, thirst
 Intake and output assessment (if IV infusion or a urinary catheter is in place)
Intake and output assessment (if IV infusion or a urinary catheter is in place)
 Incisional dressing condition (cesarean birth)
Incisional dressing condition (cesarean birth)
 Ongoing assessment, performed at least once on each shift throughout her hospital stay; the following components should be included in each assessment:
Ongoing assessment, performed at least once on each shift throughout her hospital stay; the following components should be included in each assessment:
 BUBBLE-HE is an acronym for the assessment components.
BUBBLE-HE is an acronym for the assessment components.
B Breasts (soft, filling, firm; include condition of nipples)
U Uterine fundus (location, consistency)
B Bowel function (presence or absence of bowel movement)
B Bladder function (volume, color)
L Lochia
 Lochia rubra—bright or dark red blood—lasts 3 to 4 days
Lochia rubra—bright or dark red blood—lasts 3 to 4 days
 Lochia serosa—pink or brown—lasts up to 2 weeks
Lochia serosa—pink or brown—lasts up to 2 weeks
 Lochia alba—thin, yellow to white, can last 4 to 6 weeks
Lochia alba—thin, yellow to white, can last 4 to 6 weeks
E Emotions
 Signs of potential physiologic complications are listed in the box on p. 208.
Signs of potential physiologic complications are listed in the box on p. 208.
 Hematocrit (on first postpartum day) if ordered
Hematocrit (on first postpartum day) if ordered
 Rubella status (if no results available on admission to the postpartum unit)
Rubella status (if no results available on admission to the postpartum unit)
 Rh status (if no results available on admission to the postpartum unit)
Rh status (if no results available on admission to the postpartum unit)
General Care
Newborn Safety
Prevention of Infection
 Change disposable pads and draw sheets as needed.
Change disposable pads and draw sheets as needed.
 Have the woman avoid walking barefoot to prevent contamination of bed linens when returning to bed.
Have the woman avoid walking barefoot to prevent contamination of bed linens when returning to bed.
 Have all staff members practice conscientious handwashing or use hand sanitizers.
Have all staff members practice conscientious handwashing or use hand sanitizers.
 Practice Standard Precautions.
Practice Standard Precautions.
 Teach the woman proper care of episiotomy and lacerations:
Teach the woman proper care of episiotomy and lacerations:
 Wash hands thoroughly before and after changing perineal pads.
Wash hands thoroughly before and after changing perineal pads.
 Wipe from front to back (urethra to anus) after voiding or defecating.
Wipe from front to back (urethra to anus) after voiding or defecating.
 Cleanse the perineum with plain warm water after each voiding.
Cleanse the perineum with plain warm water after each voiding.
 Change the perineal pad after each time she voids or defecates.
Change the perineal pad after each time she voids or defecates.
Prevention of Excessive Bleeding
 Massage the fundus until it is firm (teach mother how to massage the fundus).
Massage the fundus until it is firm (teach mother how to massage the fundus).
 Assist the woman to void spontaneously on toilet or bedpan by:
Assist the woman to void spontaneously on toilet or bedpan by:
ˆ Having her listen to running water
ˆ Placing her hands in warm water
ˆ Pouring water from a squeeze bottle over her perineum
ˆ Encouraging her to void in the shower or sitz bath
ˆ Administering analgesics if ordered to relieve fear of anticipated pain
 Catheterize the woman if she is unable to void spontaneously.
Catheterize the woman if she is unable to void spontaneously.
Promotion of Comfort and Rest
Comfort
 Nonpharmacologic interventions
Nonpharmacologic interventions
 Narcotics, nonsteroidal antiinflammatory medications, topical anesthetic ointment or sprays
Narcotics, nonsteroidal antiinflammatory medications, topical anesthetic ointment or sprays
Rest
Promotion of Ambulation and Exercise
Promotion of Healthy Nutrition
Promotion of Normal Bowel and Bladder Patterns
Breastfeeding Promotion/Lactation Suppression
Breastfeeding Promotion
During the first 3 days of life the breastfed infant receives colostrum, a very concentrated, high-protein fluid containing enzymes, antiinfective agents, hormones, and growth factors. As the baby adjusts to extrauterine life and the digestive tract is cleared of meconium, intake increases from 15 to 30 ml of colostrum per feeding in the first 24 hours to 60 to 90 ml of milk by the end of the first week.
Assisting with Breastfeeding
Positioning
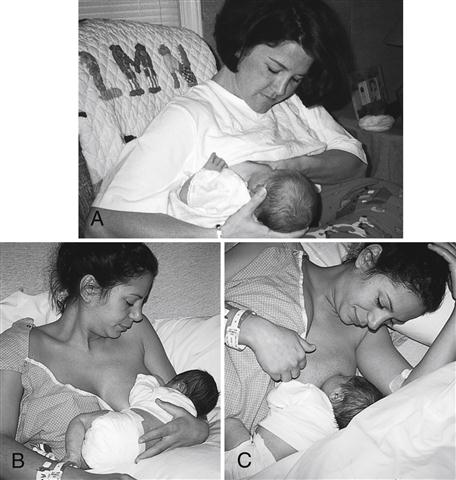
Three of the four basic positions are shown in Figure 5-1.
 Football or clutch hold (under the arm)
Football or clutch hold (under the arm)
 Usually preferred by mothers who gave birth by cesarean
Usually preferred by mothers who gave birth by cesarean
 Most common breastfeeding position for infants who have learned to latch easily and feed effectively
Most common breastfeeding position for infants who have learned to latch easily and feed effectively
 Modified cradle or across the lap
Modified cradle or across the lap
 Works well for early feedings, especially with smaller babies
Works well for early feedings, especially with smaller babies
 Allows the mother to rest while breastfeeding
Allows the mother to rest while breastfeeding
Initially it is best to use the position that most easily facilitates latch while allowing maximal comfort for the mother.
Before discharge from the hospital, assist the mother to try all four positions so that she will feel confident in her ability to vary positions at home.
Regardless of the position used, the mother should be comfortable.
Latch
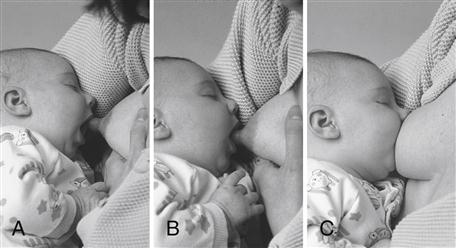
 The latch process is shown in Figure 5-2.
The latch process is shown in Figure 5-2.
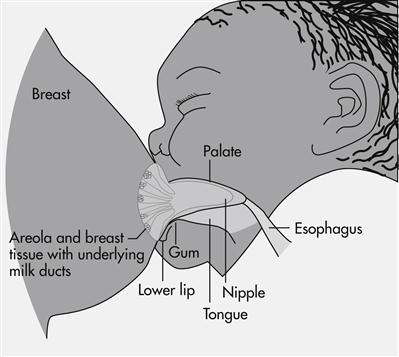
 When latched correctly, the baby’s cheeks and chin are touching the breast. Depressing the breast tissue around the baby’s nose to create breathing space is not necessary (Fig. 5-3).
When latched correctly, the baby’s cheeks and chin are touching the breast. Depressing the breast tissue around the baby’s nose to create breathing space is not necessary (Fig. 5-3).
 When the baby is nursing appropriately, the following occur:
When the baby is nursing appropriately, the following occur:
 Mother reports a firm tugging sensation on her nipples but no pinching or pain.
Mother reports a firm tugging sensation on her nipples but no pinching or pain.
 Baby sucks with cheeks rounded, not dimpled.
Baby sucks with cheeks rounded, not dimpled.
 Baby’s jaw glides smoothly with sucking.
Baby’s jaw glides smoothly with sucking.
 Swallowing is usually audible.
Swallowing is usually audible.
 To prevent nipple trauma as the baby is taken off the breast, instruct the mother to break the suction by inserting a finger in the side of the baby’s mouth between the gums and leaving it there until the nipple is completely out of the baby’s mouth (Fig. 5-4).
To prevent nipple trauma as the baby is taken off the breast, instruct the mother to break the suction by inserting a finger in the side of the baby’s mouth between the gums and leaving it there until the nipple is completely out of the baby’s mouth (Fig. 5-4).
Milk Ejection or Let-down
As the baby begins sucking on the nipple, the milk-ejection, or let-down, reflex is stimulated. The following signs indicate that milk ejection has occurred:
Frequency of Feedings
 Infants should be fed whenever they exhibit feeding-readiness cues, such as the following:
Infants should be fed whenever they exhibit feeding-readiness cues, such as the following:
 Hand-to-mouth or hand-to-hand movements
Hand-to-mouth or hand-to-hand movements
 Do not wait for the baby to cry to indicate hunger; crying is a late sign of hunger.
Do not wait for the baby to cry to indicate hunger; crying is a late sign of hunger.
 At night babies should be placed in a bassinet close to the mother for convenient breastfeeding.
At night babies should be placed in a bassinet close to the mother for convenient breastfeeding.
Duration of Feedings
 Highly variable, because the timing of milk transfer differs for each mother-baby pair
Highly variable, because the timing of milk transfer differs for each mother-baby pair
 Average time for feeding is 30 to 40 minutes, or approximately 15 to 20 minutes per breast.
Average time for feeding is 30 to 40 minutes, or approximately 15 to 20 minutes per breast.
 Rather than teaching mothers to feed for a set number of minutes, teach them to determine when a baby has finished a feeding:
Rather than teaching mothers to feed for a set number of minutes, teach them to determine when a baby has finished a feeding:
 Baby’s suck and swallow pattern has slowed
Baby’s suck and swallow pattern has slowed
 Baby appears content and may fall asleep or release the nipple
Baby appears content and may fall asleep or release the nipple
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree