The onset of symptoms may not always be immediate; sometimes they may be delayed by several hours, as is the case with certain vesicants and pulmonary agents (Table 5-2). Exposure to these agents can cause serious injury and death, and thus rapid detection of the chemical is critical to the protection of first responders and emergency medical personnel, as well as to the effective treatment of victims.
| AGENT CATEGORY | RESPIRATORY | NEUROLOGICAL | SKIN/EYES | OTHER |
|---|---|---|---|---|
| Nerve | Gasping Bronchoconstriction | Seizures Twitching | Tearing Eye irritation Blurred vision | Drooling Sweating Muscle weakness |
| Biotoxin (aerosolized ricin) | Cough Dyspnea Chest pain | Nausea Fever | ||
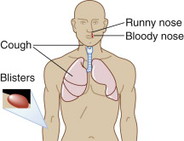
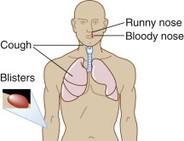
| Vesicants | Coughing Severe respiratory irritation | Itching Burning Blistering | ||
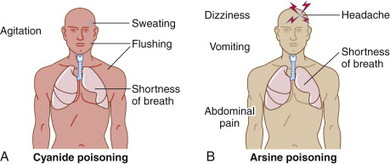
| Tissue (blood) | Hyperventilation, shortness of breath | Dizziness Convulsions Loss of consciousness | Flushing | Nausea |
| Pulmonary | Coughing Runny nose Throat irritation Dyspnea Pulmonary edema | Headache | Tearing Eye irritation and pain Blurred vision | |
| Riot control | Chest tightness Cough | Eye irritation Tearing |
CHEMICAL AGENTS: HOW TO PROTECT YOURSELF
At the scene, nurses should not be first responders, unless they are trained members of a hazardous materials (Hazmat) or fire response team. Nurses should remain outside the response zones to avoid becoming a victim. Table 5-3 refers to nurses working as first receivers at the hospital.
| AGENT CATEGORY | RESPIRATORY PROTECTION | SKIN/OCULAR PROTECTION |
|---|---|---|
| Nerve | Pressure-demand SCBA or wall-mounted air supply or PAPR with appropriate cartridge for that chemical | • Chemical-protective clothing • Butyl rubber gloves • Chemical goggles and face shield • Tychem BR or Responder CSM chemical-protective clothing • Full face-piece respirator provides eye protection • Personal protective equipment • Butyl rubber chemical protective gloves • Chemical goggles and face shield |
| Biotoxin (aerosolized ricin) | ||
| Vesicants | ||
| Tissue (blood) agents | Arsine/phosphine: Chemical-protective clothing is not generally required because arsine gas is not absorbed through skin and does not cause skin irritation. However, contact with the liquid (compressed gas) can cause frostbite injury to skin or eyes. Cyanides: Chemical-protective clothing is recommended because both hydrogen cyanide vapor and liquid can be absorbed through skin to produce systemic toxicity. Face shield or eye protection should also be worn. | |
| Pulmonary | Pressure-demand SCBA or wall-mounted air supply or PAPR with appropriate cartridge for that chemical | • Chemical-protective clothing • Chemical goggles and face shield Phosphides: Chemical-protective clothing is not generally required because phosphine gas is not absorbed through skin and skin irritation is unlikely. Use rubber gloves and aprons with victims exposed to phosphides. |
| Riot control | • Chemical-protective clothing is not generally required • Eye protection may be necessary to avoid eye irritation |
CHEMICAL AGENT DESCRIPTIONS
The following sections discuss each agent category in more detail. For each agent category, the following information is provided:
• Overview
• Recognition
• Exposure route(s) and associated onset of symptoms
• Duration and mortality
• Patient assessment
• Clinical diagnostic tests
• Patient management
• Therapy (includes information on antidotes if available)
• Personal safety risk
• Precautions
• PPE
• Family safety
• Public health reporting
NERVE AGENTS
CHEMICAL AGENT DESCRIPTION: NERVE AGENTS
OVERVIEW
Nerve agents are highly toxic compounds that inhibit the body’s normal functions. They are the most toxic of the known chemical warfare agents, which makes them a danger to humans and potential weapons in the hands of terrorists.
Nerve agents can be dispersed as aerosols/vapors or liquids. Nerve agent vapors are readily absorbed by inhalation and ocular contact and result in immediate local and systemic effects. The liquid form of the agent is also readily absorbed through the skin.
Nerve agents are divided into two categories: G agents and V agents. Examples of both follow:
• G agents: sarin (GB), soman (GD), tabun (GA)
• V agents: VX
RECOGNIZING NERVE AGENTS
Table 5-4 shows how to recognize nerve agents by appearance and odor.
| AGENT | APPEARANCE | ODOR |
|---|---|---|
| Sarin | Clear, colorless | Odorless |
| Soman | Clear, colorless | Slight camphor odor (e.g., Vicks Vapo-Rub) or rotting fruit odor |
| Tabun | Clear, colorless | Faint fruity odor |
| VX | Clear, amber-colored | Odorless |
EXPOSURE TYPES AND ONSETS
Table 5-5 indicates the onset of symptoms for each type of possible exposure.
| EXPOSURE | ONSET |
|---|---|
Inhalation Ingestion Skin/eye | Immediate onset of symptoms Readily absorbed Onset depends on concentration; can be delayed by several hours |
DURATION AND MORTALITY
Recovery may take several months. Permanent damage to the central nervous system is possible after exposure to a high dose. G agents are lethal within 1 to 10 minutes and V agents are generally lethal within 4 to 18 hours, depending on dose and route of entry.
PATIENT ASSESSMENT
 |
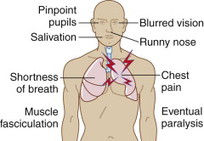
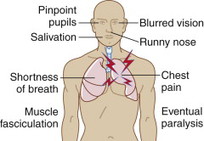
Muscle fasciculations and eventual paralysis may occur. Symptoms usually occur within seconds of exposure to a nerve agent but may take several hours when exposure is only transdermal.
Effects and time of onset of a nerve agent are dependent upon the concentration of the agent and the amount of time exposed, as well as the route of exposure.
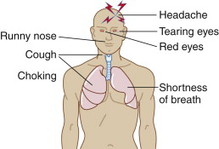
• Mild inhalational exposure: rapid onset of miosis, blurry vision, runny nose, chest tightness, dyspnea, and possible wheezing.
• Severe inhalational exposure: sudden coma, seizures, flaccid paralysis with apnea, miosis, diarrhea, and a victim who is “wet” (lacrimation, salivation, urination, sweating, copious upper and lower respiratory tract secretions).
• Mild dermal exposure: sweating and muscle fasciculations localized to the area of exposure, nausea, vomiting, diarrhea, and possible miosis.
• Severe dermal exposure: sudden coma, seizures, flaccid paralysis with apnea, miosis, diarrhea, and a victim who is “wet” (lacrimation, salivation, urination, sweating, copious upper and lower respiratory tract secretions). Onset of symptoms may be delayed by 30 minutes following exposure as the agents transit the skin.
Victims of a terrorist attack will usually have both inhalational and dermal exposures. Hours after treatment/decontamination, the agent, still in transit through the skin, may produce sudden and severe symptoms.
CLINICAL DIAGNOSTIC TESTS
Red blood cell or serum cholinesterase level.
PATIENT MANAGEMENT
• Do not approach contaminated victims unless wearing proper personal protective equipment.
• Supportive therapy and assisted ventilation as needed.
THERAPY
 Antidote: atropine and pralidoxime. Additional treatment (Table 5-6) would include benzodiazepines for seizures (not true antidote).
Antidote: atropine and pralidoxime. Additional treatment (Table 5-6) would include benzodiazepines for seizures (not true antidote).| Source: CDC at http://www.bt.cdc.gov/chemical/. | |
| ∗Mark I kits contain atropine 2 mg and 2-PAMCI 600 mg in separate auto-injectors. | |
| EXPOSURE | TREATMENT |
|---|---|
| Inhalation | • If severe signs, immediately administer, in rapid succession, all three nerve agent antidote kit(s), Mark I∗ injectors (or atropine if directed by physician). • If signs and symptoms are progressing, use injectors at 5-20 minute intervals; use no more than three injections. • Give artificial respiration if breathing has stopped or is difficult; do not use mouth-to-mouth if face is contaminated. |
| Skin | • Decontaminate using soap and water. |
| Eyes | • Immediately flush eyes with water for 10-15 minutes. • Don respiratory protective mask. |
| Ingestion | |
PERSONAL SAFETY RISK
 High, because of off-gassing vapor. However, if the patient is fully decontaminated, the risk is low.
High, because of off-gassing vapor. However, if the patient is fully decontaminated, the risk is low.PRECAUTIONS
• Maximum: standard, airborne, droplet, and contact precautions.
• Nerve agents are rapidly absorbed through the skin and may cause systemic toxicity.
PPE
See Table 5-7 for recommended PPE for nerve agents.
| PROTECTION | DESCRIPTION |
|---|---|
| Respiratory | Pressure-demand SCBA is recommended in response situations that involve exposure to any nerve agent vapor or liquid. However, at a hospital as a first RECEIVER only PAPR WITH APPROPRIATE filter is OK. |
| Skin/ocular | Chemical-protective clothing and butyl rubber gloves are recommended when skin contact is possible because nerve agent liquid is rapidly absorbed through skin and may cause systemic toxicity. |
| Wear chemical goggles and face shield. |
FAMILY SAFETY
 Low: Shower and change clothes before going home.
Low: Shower and change clothes before going home.NERVE AGENTS IN CHILDREN: GUIDELINES
See Table 5-8 for treatment guidelines for children exposed to nerve agents.
| SYMPTOMS | TRIAGE LEVEL: DISPOSITION | ATROPINE (CORRECT HYPOXIA BEFORE IV USE [RISK OF TORSADES, VFib]) | PRALIDOXIME | DIAZEPAM MAY USE OTHER BENZODIAZEPINES (e.g., MIDAZOLAM) |
|---|---|---|---|---|
| Asymptomatic | Delayed: observe | None | None | None |
| Miosis, mild rhinorrhea | Delayed: admit or observe prn | None | None | None |
| Miosis and any other symptom | Immediate to moderate: admit | 0.05 mg/kg IV or IMRepeat as needed q5-10min until respiratory status improves | 25-50 mg/kg IV or IM; may repeat every hour Watch for: Muscle rigidity Laryngospasm Tachycardia | For any neurological effect: 30 days to 5 years: 0.05-0.3 mg/kg IV to max of 5 mg/dose 5 years and older: 0.05-0.3 mg/kg IV to max of 10 mg/dose May repeat q15-30min |
| Apnea, convulsions, cardiopulmonary arrest | Immediate to severe: admit intensive care status | 0.05-0.1 mg/kg IV, IM, per ETT No maximum Repeat q5-10min as above | 25-50 mg/kg IV or IM as above | See above |
BIOTOXINS (RICIN)

CHEMICAL AGENT DESCRIPTION: BIOTOXINS (RICIN)
OVERVIEW
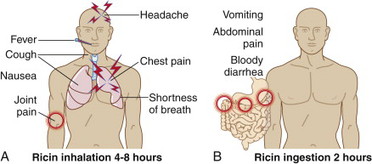
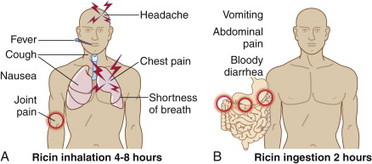
Ricin is derived from the castor bean (Ricin communis) and can be ingested, injected, or aerosolized for inhalation. Ricin is less toxic than some other biological agents but is very stable. A similar agent, abrin (derived from rosary peas) is about 25 times more toxic, but less common. Intoxication occasionally occurs in children who ingest castor beans or rosary peas.
The CDC has designated ricin as a category B bioterrorism agent. Ricin was developed as a biological weapon by the United States and its allies during World War II. Extracting the toxin is relatively easy, and Iraq and several terrorist groups are known to have produced ricin. A terrorist attack would be by aerosol release. The mortality rate of ricin is variable and largely route specific. Mortality from ricin poisoning can be high depending on the dose and route of exposure.
HOW YOU COULD BE EXPOSED TO RICIN
• It would take a deliberate act to make ricin and use it to poison people—accidental exposure to ricin is highly unlikely, but happens when people eat/chew castor beans!
• People can inhale ricin mist or powder and be poisoned.
• Ricin can also get into water or food and then be swallowed.
• Pellets of ricin, or ricin dissolved in a liquid, can be injected into the body.
• Depending on the route of exposure (such as injection or inhalation), as little as 500 micrograms of ricin could be enough to kill an adult. A 500-microgram dose of ricin would be about the size of the head of a pin. If the ricin were ingested, however, a greater amount would likely be needed to cause death.
RECOGNIZING BIOTOXINS
Table 5-9 shows how to identify ricin by appearance and odor.
| BIOTOXIN | APPEARANCE | ODOR |
|---|---|---|
| Ricin | Liquid, crystalline, dry powder | Odorless |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


