Care of Postoperative Surgical Patients
Objectives
1. Describe the care of the patient in the postanesthesia care unit (PACU).
2. Identify points the PACU nurse should cover in report to the floor nurse.
3. Formulate a plan of care for a postoperative patient returning from the PACU.
4. Determine assessment factors for each potential postoperative complication.
2. Prepare to perform an immediate postoperative assessment when a patient returns to the nursing unit.
3. Apply interventions to prevent postoperative complications.
4. Assess for postoperative pain and provide comfort measures and pain relief.
5. Promote early ambulation and return to independence in activities of daily living.
6. Perform discharge teaching necessary for postoperative home self-care.
Key Terms
anaphylaxis (ă-nă-fă-LĂK-sĭs, p. 93)
atelectasis (ă-tĕ-LĔK-tă-sĭs, p. 84)
dehiscence (dĕ-HĬS-ĕntz, p. 91)
embolus (ĔM-bō-lŭs, p. 88)
evisceration (ē-vĭs-ĕr-Ā-shŭn, p. 91)
hematoma (hē-mă-TŌ-mă, p. 89)
malignant hyperthermia (MH) (hī-pĕr-THĔR-mē-ă, p. 93)
paralytic ileus (păr-ă-LĬT-ĭk ĬL-ē-ŭs, p. 87)
pneumonia (nū-MŌ-nē-ă, p. 86)
purulence (PŪ-rū-lĕns, p. 89)
seroma (sĕ-RŌ-mă, p. 89)
thrombophlebitis (thrŏm-bō-flĕ-BĪ-tĭs, p. 85)
thrombosis (thrŏm-BŌ-sĭs, p. 85)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Immediate Postoperative Care
Postanesthesia Care Unit
When surgery with general anesthesia is completed, the patient is usually transferred to the postanesthesia care unit (PACU) adjacent to the surgical suites (Figure 5-1). Patients who have had spinal anesthesia for a major procedure go to the PACU also. Very critically ill patients, such as those recovering from open heart surgery, are often taken directly to the intensive care unit for anesthesia recovery. Surgical patients who had procedural sedation or a local or regional anesthetic are usually recovered in the ambulatory surgery area. The PACU nurse receives a verbal report from the anesthesia care provider about the procedure, blood loss, anesthesia administered, fluids infused, medications administered, and any problems encountered.
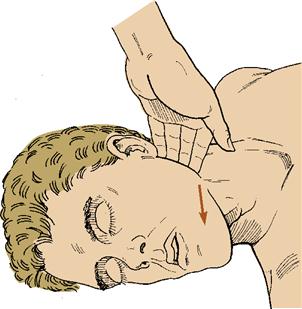
The patient is immediately attached to the cardiac and pulse oximeter monitors, and oxygen is usually administered if the patient had general anesthesia. Oxygen helps eliminate the anesthetic gases and helps meet the increased metabolic demand for oxygen caused by surgery. Any respiratory problems are immediately addressed, as maintenance of airway and adequate ventilation takes priority. An oral airway may be in place because the anesthesia medications often cause the tongue to occlude the airway. Alternatively, the airway can be opened by moving the jaw forward (Figure 5-2). Suction is on and readily available to clear secretions. If needed, mechanical ventilation is provided. Warm blankets are placed over the patient, vital signs are assessed and compared with baseline readings, and a full neurologic assessment is performed. Neurologic assessment includes level of consciousness, orientation, sensory and motor status, and size, equality, and reactivity of the pupils. The patient may be asleep, drowsy but arousable, or awake.
Determine intake and output to assess function of the urinary system. Closely monitor urinary output. Check all intravenous (IV) lines for patency, verify the correct solutions along with the correct drip rate, and inspect wound drains and evacuation devices for proper function. Assess dressings for unexpected drainage.
Surgical recovery can take from 2 to 6 hours. Because patients are coming out of anesthesia through various stages and are unstable, keep the environment as quiet as possible. Briefly communicate with the staff in hushed tones. The patient may wake up confused and may need reorientation and reassurance that the surgery is over, that he is in the recovery room, and that his family member or relative has been notified. Once the patient is awake, family members are sometimes allowed to visit for a few minutes so that they are assured that their loved one is all right and recovering.
Assessments are performed at least every 15 minutes or according to the status of the patient. Assessment for complications of the particular surgery and anesthesia are ongoing. The patient remains in the PACU until the vital signs are stable and the patient is awake and able to respond to stimuli. A form of the Aldrete scoring system may be used to determine readiness for transfer. Activity, respiration, circulation, consciousness, skin color, and oxygen saturation are each given a score. The patient with a score of 9 or
transfer. Activity, respiration, circulation, consciousness, skin color, and oxygen saturation are each given a score. The patient with a score of 9 or
10 is ready for transfer to the nursing unit. Report is given to the staff nurse (Box 5-1).
For many procedures the patient may be transferred from the operating room (OR) directly back to the same-day surgery unit. Monitor the patient’s respirations, circulation, vital signs, neurologic status, fluid balance, wound drainage and dressings, and comfort level. When the vital signs are stable, the patient is allowed to sit up and then is ambulated. If discharge criteria are met, the patient may be discharged when able to ambulate unassisted and empty the bladder. Recovery time in the same-day surgery unit usually takes 1 to 3 hours. Discharge teaching is begun before the surgery and continues once the patient is again alert. Written instructions are always sent home with the patient. If the patient has undergone sedation, another adult driver must provide transportation home after same-day surgery. Advise surgery patients who have received anesthesia or procedural sedation not to resume normal activities or make important decisions for at least 24 hours after surgery. The phone number of the surgeon and signs and symptoms to report are written on the postoperative instruction sheet.
Immediate Postoperative Care
Nursing Management
Assessment (Data Collection)
After the patient is transferred from recovery, check identity, settle the patient in bed, and perform an initial postoperative assessment. Airway, breathing, and circulation are always the top priorities. This provides a baseline against which frequent postoperative assessment data can be compared to prevent or quickly detect signs of complications. Vital signs are taken more frequently if they are unstable; this is a nursing judgment.
Monitoring for signs of the various surgical complications that may occur is a major nursing responsibility. The first 72 hours after surgery require frequent observations to detect signs of postoperative complications.
Nursing Diagnosis
Nursing diagnoses commonly used for postoperative patients who have undergone general anesthesia are:
• Impaired gas exchange related to the effect of anesthesia on the lungs
• Ineffective breathing pattern related to analgesia and pain
• Impaired skin integrity related to surgical incision
• Risk for infection related to surgical wound
• Risk for injury related to sedation, decreased level of consciousness, or excessive blood loss
• Acute pain related to disruption of tissue
• Ineffective airway clearance related to inability to breathe deeply and cough without discomfort
• Deficient fluid volume related to fluid loss and nothing by mouth (NPO) status
• Risk for constipation related to opioid analgesics, decreased mobility, and decreased peristalsis
• Ineffective tissue perfusion related to surgery, anesthesia, and positioning in the OR
• Ineffective coping related to loss of body part or change in body image
• Impaired urinary elimination related to effects of anesthesia or presence of catheter
For patients who have undergone spinal anesthesia, include all of the above diagnoses plus:
• Impaired physical mobility related to effects of spinal anesthesia
• Risk for injury related to decreased sensation and movement in lower extremities
Planning
The expected outcomes depend on the individual specific nursing diagnoses. General nursing goals are:
• Maintain patent airway and adequate respiratory exchange.
• Maintain adequate tissue perfusion.
• Promote normal physiologic body function.
• Promote psychological adjustment to lifestyle or body image changes.
When planning your work for the shift, allow time for frequent postoperative assessments. Careful planning is essential so that proper care for the early postoperative patient does not override the needs of other patients.
Implementation
Maintain Ventilation
 The postoperative patient is at risk for respiratory problems from the effects of anesthesia on the lungs, being in one position for the duration of surgery, and limited mobility in the immediate postoperative period. Maintaining a patent airway is a priority measure. Unless contraindicated, the patient must be positioned on the side or with the head turned to the side to prevent aspiration until fully recovered, alert, and with the gag reflex intact. Monitor oxygen saturation closely, and administer oxygen as ordered.
The postoperative patient is at risk for respiratory problems from the effects of anesthesia on the lungs, being in one position for the duration of surgery, and limited mobility in the immediate postoperative period. Maintaining a patent airway is a priority measure. Unless contraindicated, the patient must be positioned on the side or with the head turned to the side to prevent aspiration until fully recovered, alert, and with the gag reflex intact. Monitor oxygen saturation closely, and administer oxygen as ordered.
Some degree of atelectasis (collapse of alveoli in the lungs) exists after anesthesia. A mild hypoxia is usually present for about 48 hours after surgery. A large percentage of all patients who have had either abdominal or thoracic surgery suffer from increasing atelectasis and pneumonitis. If any area of the lung remains atelectatic for more than 72 hours, hypostatic pneumonia from retained secretions is likely to occur.
Hypostatic pneumonia results when lack of movement or of position change causes stasis of secretions, which become a breeding ground for bacteria. Auscultate the lungs carefully for abnormal sounds indicating retained secretions, assess the rate and depth of breathing, and encourage the patient to deep breathe and cough every 2 hours. Coughing to remove secretions may be contraindicated for patients who have had a hernia repair or eye, ear, brain, jaw, or plastic surgery. Check the physician’s orders. If the patient cannot cough effectively, instruct to “huff” cough (see Patient Teaching, Lung Exercises on p. 71-72).
Be certain the patient turns every 2 hours, which changes the distribution of gas and blood flow in the lungs and helps move secretions. Early ambulation is ordered to promote ventilation. Signs of complications for procedures other than thoracic surgery are complaints of shortness of breath, pain on inspiration, and extreme fatigue (which is related to hypoxemia).
The use of an incentive spirometer is especially helpful to prevent atelectasis and hypoventilation (see Chapter 4). It should be used every hour while the patient is awake for the first 24 hours following surgery, and every 2 hours thereafter. The elderly patient may need extra coaching to master the spirometer technique.
A pulse oximeter may be used to determine blood oxygenation. Monitor oxygen readings periodically and report oxygen saturation (SaO2) readings below 95%.
Maintain Circulation and Tissue Perfusion
When considerable blood is lost during surgery, a blood transfusion may be ordered. Autologous blood may be transfused if the patient donated blood several weeks before surgery or if the patient’s blood was collected as it was lost during surgery. This blood is filtered and returned to the patient.
If surgery involves an extremity (arm, leg, foot, or hand) or if a procedure has been done to the pelvic area, the distal or peripheral pulse is checked during each full assessment. Swelling at the surgical site can compress vessels and decrease blood flow distal to the surgical site. The skin distal to the surgical site should be warm to the touch, and there should be brisk capillary refill in the fingers or toes. Color, movement, and sensation of the fingers and toes should be checked to detect nerve compression from swelling and edema.
Blood pressure and pulse should be compared with preoperative values to determine if there are significant changes. An increase in pulse may indicate that internal bleeding is occurring, but it can also signify incomplete pain control. Blood pressure falling below the patient’s normal baseline level may indicate major bleeding.
Core Measures (The Joint Commission [TJC], 2008) require antithrombosis therapy after many surgeries. The use of antiembolic (elastic) stockings increases venous return from the legs and helps prevent stasis of blood in the lower extremities. The stockings should be checked frequently to ensure that they fit smoothly. They may be removed for 20 minutes per shift for bathing, to allow air circulation to the skin, and/or full skin inspection (Winslow & Brosz, 2008).
(Winslow & Brosz, 2008).
If the patient is at considerable risk of venous thrombosis (blood clot), the surgeon may order pneumatic sequential compression devices (SCDs) to be applied to the legs. SCDs alternately compress and release, squeezing the legs and propelling blood along the vessels (Figure 5-3). Orders for ambulation are written as soon as the patient is able to be up and walking.
Low-molecular-weight subcutaneous heparin injections may be ordered as a general precaution and for any patient who has a history of thrombophlebitis (clot and inflammation in a blood vessel). Patients undergoing hip surgery also receive heparin. Thrombophlebitis may not occur until after the fifth day of bed rest, when stasis has allowed a clot to form and irritate the vein. Question the patient about pain or tenderness in the legs. If the patient complains of leg pain, gently assess the skin for increased warmth, and notify the physician.
Prevent Injury
Safety is a primary concern until the patient is fully recovered from anesthesia. Always leave the bed in the low position after administering care. Remind the patient to call for assistance as needed and be certain the call bell is within reach. Core Measures (The Joint Commission, 2011) require the use of interventions to prevent falls. Remember that you are the patient’s advocate while the patient is still recovering from surgery and anesthesia or is under the influence of narcotic analgesia. Be certain that all appropriate safety measures are listed on the patient’s care plan.
Reassure the patient who has had spinal anesthesia that it is normal for the legs to feel numb and heavy, and that feeling will soon return to normal. Maintain a flat position with only a pillow until feeling returns. Sense of position in space will return to the legs first, followed by sensation to deep pressure, voluntary movement, and finally feeling of superficial pain and temperature. A feeling of “pins and needles” in the legs is common. The patient is susceptible to hypotension until all effects of the spinal anesthesia are gone. Lying flat for 6 to 8 hours may decrease the chance of post–spinal anesthesia headache. If a headache develops, staying flat in bed reduces the pain. Keep IV fluid running as ordered. Encourage the patient to drink a lot of fluids, including those containing caffeine. The patient can turn the head to the side and sip from a straw while someone else holds the container. Fluids and caffeine raise the vascular pressure at the spinal puncture site and help to seal the hole.
Many surgical procedures last several hours, which means that the patient has been lying motionless, in a fixed position, on a hard table for a considerable time. Check pressure points related to the position that the patient was in during surgery and provide padding and appropriate positioning for areas that are painful (see Chapter 43).
Prevent Infection
Use aseptic technique when caring for the postoperative patient. Good hand hygiene is the primary means of preventing infection. Dressing changes are performed with strict sterile technique while the patient is in the hospital; the patient may use clean technique at home. Encouraging fluid intake in order to flush the bladder will help prevent a bladder infection for the patient who was catheterized or has an indwelling catheter. Turning, coughing, deep breathing, and ambulation will assist in preventing pneumonia (inflammation and accumulation of exudate in the lung) from retained secretions and lack of movement. Aseptically handling drains and aseptically emptying wound drainage devices prevents the entry of microorganisms.
Core Measures (TJC, 2008) state that if the patient is receiving a prophylactic antibiotic, it must be discontinued within 24 hours after surgery. Assess the surgical wound area each shift and assess for signs of infection (e.g., local pain, increased tenderness, warmth, redness, or drainage of purulent material). Monitor the blood count for increasing leukocytes (white blood cells [WBCs]) and the body temperature for unexpected increase.
Maintain Fluid Balance and Elimination
Urine output is closely monitored after surgery. If the patient has an indwelling catheter, observe the urine in the bag every hour in the early postoperative period. Report urine flow less than 30 mL/hr to the charge nurse. Check the catheter to ensure that it is not kinked and that the connecting tubing is not lying beneath the patient. The patient without a catheter in place must void within 4 to 8 hours depending on the type of surgery undergone. If the patient is unable to empty the bladder spontaneously, obtain an order for catheterization. If flow is less than 60 mL over a 2-hour period, the surgeon must be notified.
Patients usually return from surgery with an IV infusion running. Depending on the type of surgery, IV fluids may be continued for a few days or may be discontinued after the fluid has infused. Check orders to see that the correct solution is running. No potassium additive should be given until the urine flow is at least 30 mL/hr. Potassium may cause hyperkalemia if kidney function is not adequate. Assess the IV site for patency, flow rate, and complications each hour. Document all IV fluids administered as intake on the intake and output record.
As soon as the patient is conscious and the gag reflex has returned, offer a few ice chips or sips of water, unless there is an order to maintain NPO status. Document all oral intake, as well as IV fluids administered. At the end of each shift, calculate and document the difference between the intake and output. Because fluids were lost during surgery, the body will initially retain fluid. Postoperatively, the output will slowly increase until it is more than the intake; after 2 to 3 days, fluids should again be balanced.
Anesthesia may cause nausea, and vomiting. Keep the emesis basin close by, and position the patient on the side to prevent aspiration. Check the orders to determine on which side the patient can be positioned. The surgeon usually writes an order for medication in the event of excessive nausea or vomiting. To prevent stress on the incision and sutures, it is best to medicate the patient before actual vomiting occurs.
Apply a cool cloth to the forehead and back of the neck, rinse the mouth, rid the room of odors, and provide a quiet environment to help reduce nausea. After emesis, mouth care should be provided. If vomiting is uncontrolled with medication, a nasogastric (NG) tube, which suctions stomach contents and prevents fluid and electrolyte loss, may need to be inserted.
Surgeons often place an NG tube after abdominal procedures because handling of the gastrointestinal tract and general anesthesia cause peristalsis to halt, which means that secretions will not flow through the system properly. The NG tube removes gathering secretions. When an NG tube is in place, check that the tube is positioned and functioning properly and that the suction is set according to orders. Assess the amount of drainage produced every 1 to 2 hours. If the drainage turns dark brown and grainy, it should be checked for blood using a special reagent. Report the presence of blood to the surgeon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






 Assignment Considerations
Assignment Considerations












