Section 5 A systems approach
5.1 The cardiovascular system
Hypertension
The control of hypertension can lead to the prevention of its cardiovascular complications. A raised systolic blood pressure is now regarded as being more significant than a raised diastolic pressure as a risk factor for CVD and isolated systolic hypertension is associated with a two to three times greater death rate from heart disease (Table 5.1).
Table 5.1 British Hypertension Society (BHS) classification of blood pressure levels
| Category | Systolic BP (mmHg) | Diastolic BP (mmHg) |
|---|---|---|
| Optimal BP | < 120 | < 80 |
| Normal BP | < 130 | < 85 |
| High normal BP | 130–139 | 85–89 |
| Grade 1 hypertension (mild) | 140–159 | 90–99 |
| Grade 2 hypertension (moderate) | 160–179 | 100–109 |
| Grade 3 hypertension (severe) | > 180 | > 110 |
| Isolated systolic hypertension (grade 1) | 140–159 | < 90 |
| Isolated systolic hypertension (grade 2) | > 160 | < 90 |
These levels will be at least 5 mmHg lower if ambulatory monitoring of blood pressure is used or home monitoring of blood pressure. The reader is referred to the full NICE guidelines on Hypertension.
There are risk factors associated with essential hypertension and these include:
 Phaeochromocytoma (tumour of the adrenal medulla).
Phaeochromocytoma (tumour of the adrenal medulla).
 Conn’s syndrome (hyperaldosteronism).
Conn’s syndrome (hyperaldosteronism).
 Cushing’s disease (overactivity of the adrenal cortex or due to administration of long-term steroids).
Cushing’s disease (overactivity of the adrenal cortex or due to administration of long-term steroids).
 Acromegaly (excessive growth hormone in adulthood).
Acromegaly (excessive growth hormone in adulthood).
Diagnosis
 A blood pressure in the doctor’s surgery of 140/90 mmHg or more is followed by ambulatory blood pressure monitoring (ABPM) at home. If this is higher than 135/85 mmHg this is classed as Stage 1 hypertension.
A blood pressure in the doctor’s surgery of 140/90 mmHg or more is followed by ambulatory blood pressure monitoring (ABPM) at home. If this is higher than 135/85 mmHg this is classed as Stage 1 hypertension.
 Stage 2 hypertension is a clinic reading of 160/100 mmHg or higher followed by ABPM average of 150/95 mmHg.
Stage 2 hypertension is a clinic reading of 160/100 mmHg or higher followed by ABPM average of 150/95 mmHg.
 In severe hypertension the clinic systolic BP is 180 mmHg or higher or the clinic diastolic BP is 110 mmHg or higher.
In severe hypertension the clinic systolic BP is 180 mmHg or higher or the clinic diastolic BP is 110 mmHg or higher.
Medication
The British Hypertension Society (BHS) and the National Institute for Health and Clinical Excellence (NICE) have together issued guidelines on the pharmacological management of hypertension (www.nice.org.uk).
Step 1
 For those younger than 55 years of age, angiotensin-converting enzyme (ACE) inhibitors, e.g. ramipril or an angiotensin receptor blocker (ARB) such as losartan (used if intolerance such as a cough with ACE-inhibitors) are the first-line treatment.
For those younger than 55 years of age, angiotensin-converting enzyme (ACE) inhibitors, e.g. ramipril or an angiotensin receptor blocker (ARB) such as losartan (used if intolerance such as a cough with ACE-inhibitors) are the first-line treatment.
 For those over 55 years of age or black patients of any age, calcium channel blockers, e.g. diltiazem, are the first-line therapy. If these are not suitable because of the presence of oedema, or intolerance or heart failure then a thiazide diuretic, e.g. chlortalidone or indapamide should be given rather than the conventional bendroflumethiazide.
For those over 55 years of age or black patients of any age, calcium channel blockers, e.g. diltiazem, are the first-line therapy. If these are not suitable because of the presence of oedema, or intolerance or heart failure then a thiazide diuretic, e.g. chlortalidone or indapamide should be given rather than the conventional bendroflumethiazide.
Low blood pressure
 Lead to reduced tissue perfusion throughout the body and a state of shock.
Lead to reduced tissue perfusion throughout the body and a state of shock.
 Reduce the blood supply to the heart.
Reduce the blood supply to the heart.
 Reduce renal blood flow and thus reduce urine output – leading to renal tubular necrosis.
Reduce renal blood flow and thus reduce urine output – leading to renal tubular necrosis.
 Reduce blood flow to the brain and eventually lead to unconsciousness. It may result in permanent brain damage.
Reduce blood flow to the brain and eventually lead to unconsciousness. It may result in permanent brain damage.
Causes of hypotension
Management
 This will depend on the cause of the hypotension.
This will depend on the cause of the hypotension.
 Record observations of blood pressure, pulse and respirations as prescribed.
Record observations of blood pressure, pulse and respirations as prescribed.
 When the blood pressure is low, the pulse rate will usually be increased (tachycardia).
When the blood pressure is low, the pulse rate will usually be increased (tachycardia).
 The respiratory rate may also be increased, as in acidosis or haemorrhage, but in severe instances the rate may be reduced and respirations may be shallow.
The respiratory rate may also be increased, as in acidosis or haemorrhage, but in severe instances the rate may be reduced and respirations may be shallow.
 Fluid replacement may be commenced by intravenous infusion and a plasma expander such as Gelofusine may be given.
Fluid replacement may be commenced by intravenous infusion and a plasma expander such as Gelofusine may be given.
 If blood has been lost the doctor will group and crossmatch the patient and order a transfusion.
If blood has been lost the doctor will group and crossmatch the patient and order a transfusion.
 The urine output has to be closely monitored as hypotension can lead to impaired renal function. It may be necessary to catheterize the patient if the urine output falls and it should remain above 30 ml per hour.
The urine output has to be closely monitored as hypotension can lead to impaired renal function. It may be necessary to catheterize the patient if the urine output falls and it should remain above 30 ml per hour.
 The patient may be anxious and will need reassurance.
The patient may be anxious and will need reassurance.
 Investigations such as an electrocardiogram, chest X-ray and blood cultures to identify infection may be ordered.
Investigations such as an electrocardiogram, chest X-ray and blood cultures to identify infection may be ordered.
Coronary artery disease
Others we may be able to change with treatment. These include:
The National Service Framework (NSF) has set standards of care with the aim of reducing CAD-related deaths in the under-75-year age group by 40% by the year 2010. These guidelines are available on the Department of Health website at www.dh.gov.uk.
Angina pectoris
Types of angina
 Stable angina – ‘angina of effort’ – the commonest form.
Stable angina – ‘angina of effort’ – the commonest form.
 Variant (Prinzmetal’s) angina – may occur at rest – usually due to spasm of a coronary artery.
Variant (Prinzmetal’s) angina – may occur at rest – usually due to spasm of a coronary artery.
 Nocturnal angina – wakes the patient up – may occur with vivid dreams.
Nocturnal angina – wakes the patient up – may occur with vivid dreams.
 Unstable angina (see acute coronary syndrome) – rapidly worsening angina of recent onset or occurring at rest.
Unstable angina (see acute coronary syndrome) – rapidly worsening angina of recent onset or occurring at rest.
Clinical features of stable angina
 The pain is usually in the chest but may extend down the left arm or both arms or into the neck and jaw.
The pain is usually in the chest but may extend down the left arm or both arms or into the neck and jaw.
 Some patients may experience pain just in the arm, the neck, the jaw or the back.
Some patients may experience pain just in the arm, the neck, the jaw or the back.
 It is usually described as a tightness or squeezing pain, gripping or a heavy discomfort.
It is usually described as a tightness or squeezing pain, gripping or a heavy discomfort.
 The pain is brought on by exertion (angina of effort), excitement or extreme cold, all of which increase the oxygen demand of the myocardium.
The pain is brought on by exertion (angina of effort), excitement or extreme cold, all of which increase the oxygen demand of the myocardium.
 The pain fades fairly rapidly on rest.
The pain fades fairly rapidly on rest.
 A glyceryl trinitrate (GTN) tablet sublingually or GTN spray buccally usually gets rid of the pain.
A glyceryl trinitrate (GTN) tablet sublingually or GTN spray buccally usually gets rid of the pain.
 The pain will always occur after a similar amount of physical exertion.
The pain will always occur after a similar amount of physical exertion.
 The distribution of the pain will be the same each time but in more severe attacks it may extend further.
The distribution of the pain will be the same each time but in more severe attacks it may extend further.
 Sometimes the pain of angina is mild and the patient confuses it with heartburn or ignores it.
Sometimes the pain of angina is mild and the patient confuses it with heartburn or ignores it.
Management of stable angina
General advice will aim to restore normal exercise capacity and will include:
Pharmacological management
Nitrates
 These may be given in several forms and relieve the pain of angina by causing vasodilatation. They are coronary vasodilators but also reduce the work of the left ventricle by reducing venous return due to venodilatation. All nitrates may produce a troublesome headache.
These may be given in several forms and relieve the pain of angina by causing vasodilatation. They are coronary vasodilators but also reduce the work of the left ventricle by reducing venous return due to venodilatation. All nitrates may produce a troublesome headache.
 GTN may be given as a tablet sublingually or as an aerosol spray. Its onset of action is very rapid, 1–2 minutes, and its duration of action is under 30 minutes. The spray has a longer storage life.
GTN may be given as a tablet sublingually or as an aerosol spray. Its onset of action is very rapid, 1–2 minutes, and its duration of action is under 30 minutes. The spray has a longer storage life.
 GTN may also be given in the form of a sustained-release transdermal patch where the GTN is absorbed through the skin.
GTN may also be given in the form of a sustained-release transdermal patch where the GTN is absorbed through the skin.
 Isosorbide mononitrate and isosorbide dinitrate are both longer-acting nitrates that are given once or twice daily.
Isosorbide mononitrate and isosorbide dinitrate are both longer-acting nitrates that are given once or twice daily.
 Tolerance and reduced therapeutic effects may occur with prolonged use of long-acting nitrates, including transdermal patches. The patches should be removed for several consecutive hours in each 24-hour period to prevent this from happening.
Tolerance and reduced therapeutic effects may occur with prolonged use of long-acting nitrates, including transdermal patches. The patches should be removed for several consecutive hours in each 24-hour period to prevent this from happening.
Beta-blockers
 Contraindicated in asthma, beta-blockers reduce the heart’s demand for oxygen and also reduce pulse rate and blood pressure.
Contraindicated in asthma, beta-blockers reduce the heart’s demand for oxygen and also reduce pulse rate and blood pressure.
 An example of a general beta-blocker is propranolol, but cardioselective beta-blockers such as atenolol are usually used. These block the beta-1 receptors in the heart in preference to the beta-2 receptors found in other parts of the body, e.g. the bronchi, but are still not regarded as safe in those with asthma.
An example of a general beta-blocker is propranolol, but cardioselective beta-blockers such as atenolol are usually used. These block the beta-1 receptors in the heart in preference to the beta-2 receptors found in other parts of the body, e.g. the bronchi, but are still not regarded as safe in those with asthma.
Calcium antagonists
These vasodilate and may be used in angina or hypertension. An example is amlodipine.
Lipid-lowering drugs
 As a raised low-density lipoprotein (LDL) cholesterol is a risk factor for CHD, statins such as atorvastatin are prescribed if the total cholesterol is above 4.8 mmol/l.
As a raised low-density lipoprotein (LDL) cholesterol is a risk factor for CHD, statins such as atorvastatin are prescribed if the total cholesterol is above 4.8 mmol/l.
 These drugs reduce the total cholesterol by inhibiting an enzyme in the liver that allows the manufacture of cholesterol from saturated fats.
These drugs reduce the total cholesterol by inhibiting an enzyme in the liver that allows the manufacture of cholesterol from saturated fats.
Unstable angina
 More ominous symptoms than stable angina.
More ominous symptoms than stable angina.
 The episodes of pain are more frequent.
The episodes of pain are more frequent.
 They may occur without obvious cause and at rest.
They may occur without obvious cause and at rest.
 Some patients present atypically with pleuritic pain, indigestion or dyspnoea.
Some patients present atypically with pleuritic pain, indigestion or dyspnoea.
 12-lead ECG may be normal in ACS but there may be ST depression and T-wave inversion.
12-lead ECG may be normal in ACS but there may be ST depression and T-wave inversion.
 The patient is admitted to hospital.
The patient is admitted to hospital.
 Urgent angiography is required for diagnosis and treatment in those in danger of progressing to myocardial infarction or death.
Urgent angiography is required for diagnosis and treatment in those in danger of progressing to myocardial infarction or death.
 Anti-platelet drugs are vitally important. Aspirin is given but other anti-platelet drugs such as clopidogrel are additionally used.
Anti-platelet drugs are vitally important. Aspirin is given but other anti-platelet drugs such as clopidogrel are additionally used.
 Low-molecular-weight heparins such as enoxaparin are used as anticoagulants.
Low-molecular-weight heparins such as enoxaparin are used as anticoagulants.
 Beta-blockers may be given to reduce the demand of the heart for oxygen and nutrients.
Beta-blockers may be given to reduce the demand of the heart for oxygen and nutrients.
 Statins and ACE inhibitors are also routinely given in ACS and appear to stabilize the plaque.
Statins and ACE inhibitors are also routinely given in ACS and appear to stabilize the plaque.
ST elevation myocardial infarction
Clinical features
 Chest pain which is tight or crushing in nature; 80% of patients have this.
Chest pain which is tight or crushing in nature; 80% of patients have this.
 The pain may be similar to that of angina, but more severe.
The pain may be similar to that of angina, but more severe.
 The pain lasts longer than angina – usually more than 20 minutes.
The pain lasts longer than angina – usually more than 20 minutes.
 Pain may radiate to the arms, throat and jaw.
Pain may radiate to the arms, throat and jaw.
 The pain may not respond to sublingual GTN and morphine is usually needed.
The pain may not respond to sublingual GTN and morphine is usually needed.
 Nausea and vomiting may occur.
Nausea and vomiting may occur.
Early medical management
The main aim is revascularization:
 A 12-lead ECG should be done as soon as the patient is admitted. If this baseline ECG is normal (rare) it should be repeated every 15 minutes for as long as the patient is still in pain.
A 12-lead ECG should be done as soon as the patient is admitted. If this baseline ECG is normal (rare) it should be repeated every 15 minutes for as long as the patient is still in pain.
 The patient will be connected to a cardiac monitor for immediate detection of cardiac arrhythmias. These are common following a STEMI.
The patient will be connected to a cardiac monitor for immediate detection of cardiac arrhythmias. These are common following a STEMI.
 An intravenous cannula will be inserted to allow drugs to be given easily and immediately.
An intravenous cannula will be inserted to allow drugs to be given easily and immediately.
 Blood samples will be taken for cardiac markers (see below), full blood count (FBC), biochemistry, lipids and glucose.
Blood samples will be taken for cardiac markers (see below), full blood count (FBC), biochemistry, lipids and glucose.
 Analgesia will be given as needed to try to keep the patient pain free. This is likely to be IV diamorphine 2.5–5 mg and an anti-emetic if needed, e.g. metoclopramide 10 mg.
Analgesia will be given as needed to try to keep the patient pain free. This is likely to be IV diamorphine 2.5–5 mg and an anti-emetic if needed, e.g. metoclopramide 10 mg.
 The patient will be made comfortable using the headrest and pillows.
The patient will be made comfortable using the headrest and pillows.
 Oxygen may be prescribed if the oxygen saturation measured by pulse oximetry is below 94% (British Thoracic Society Guidelines).
Oxygen may be prescribed if the oxygen saturation measured by pulse oximetry is below 94% (British Thoracic Society Guidelines).
 Observations of blood pressure and pulse will be monitored half hourly at first.
Observations of blood pressure and pulse will be monitored half hourly at first.
Cardiac markers of myocardial necrosis
 These are substances that are released into the bloodstream by the damaged myocardium and may be measured by biochemical assays.
These are substances that are released into the bloodstream by the damaged myocardium and may be measured by biochemical assays.
 Examples are cardiac troponins I and T and creatinine kinase (CK).
Examples are cardiac troponins I and T and creatinine kinase (CK).
 They rise following cardiac damage and this may confirm the diagnosis of myocardial infarction.
They rise following cardiac damage and this may confirm the diagnosis of myocardial infarction.
 CK is a relatively non-specific marker as it is also released by damaged skeletal muscle. It peaks within 24 hours of MI and falls back to baseline in 48 hours.
CK is a relatively non-specific marker as it is also released by damaged skeletal muscle. It peaks within 24 hours of MI and falls back to baseline in 48 hours.
 Troponins are highly specific to damaged cardiac muscle although they may be undetectable within the first 12 hours of the MI (see Table 2.4).
Troponins are highly specific to damaged cardiac muscle although they may be undetectable within the first 12 hours of the MI (see Table 2.4).
Cardiac arrhythmias
Cardiac arrhythmia is the commonest and most lethal complication of an MI. The most dangerous irregularity is ventricular fibrillation (VF) which constitutes a cardiac arrest. This is shown in Figure 5.1. Immediate treatment of VF using defibrillation (DC shock) may be lifesaving.
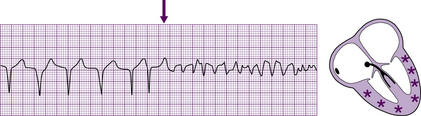
Fig. 5.1 Ventricular fibrillation.
From Hampton/The ECG Made Easy, Elsevier 2003, reproduced with permission.
Drugs used to treat cardiac arrhythmias include the following:
 Amiodarone – used in atrial fibrillation and other supraventricular arrhythmias but also ventricular arrhythmias including non-responsive ventricular tachycardia. Amiodarone should be given by a central line if possible when given intravenously.
Amiodarone – used in atrial fibrillation and other supraventricular arrhythmias but also ventricular arrhythmias including non-responsive ventricular tachycardia. Amiodarone should be given by a central line if possible when given intravenously.
 Lidocaine – used in ventricular arrhythmias, including ventricular tachycardia.
Lidocaine – used in ventricular arrhythmias, including ventricular tachycardia.
 Digoxin – used in atrial fibrillation.
Digoxin – used in atrial fibrillation.
 Adenosine – extremely short-acting drug useful in paroxysmal supraventricular tachycardia but often used as an aid to the diagnosis of broad or narrow complex supraventricular tachycardias.
Adenosine – extremely short-acting drug useful in paroxysmal supraventricular tachycardia but often used as an aid to the diagnosis of broad or narrow complex supraventricular tachycardias.
 Verapamil – a calcium antagonist that is occasionally used in supraventricular tachycardias. It must not be given to a patient who is being treated with a beta-blocker as both drugs reduce the force of cardiac contractions.
Verapamil – a calcium antagonist that is occasionally used in supraventricular tachycardias. It must not be given to a patient who is being treated with a beta-blocker as both drugs reduce the force of cardiac contractions.
 Beta-blockers – act mainly by decreasing the effects of the sympathetic nervous system on the heart. They may be used with digoxin to control the ventricular response in atrial fibrillation and are also useful in some forms of supraventricular tachycardia. Esmolol and sotalol are examples.
Beta-blockers – act mainly by decreasing the effects of the sympathetic nervous system on the heart. They may be used with digoxin to control the ventricular response in atrial fibrillation and are also useful in some forms of supraventricular tachycardia. Esmolol and sotalol are examples.
 Atropine – used to treat bradyarrhythmias (slow rate), although a pacemaker may sometimes be needed.
Atropine – used to treat bradyarrhythmias (slow rate), although a pacemaker may sometimes be needed.
Different cardiac arrhythmias and their causes are shown in Table 5.2.
Table 5.2 Causes of different cardiac arrhythmias
| Abnormal impulse formation and ectopic beats | Conduction disturbances |
|---|---|
| At the sinus node Sinus arrhythmia Sinus bradycardia Sinus tachycardia Sinus arrest | In the sinus node SA block |
| In the atria Atrial ectopic beats Atrial tachycardia Atrial fibrillation Atrial flutter Wandering atrial pacemaker | In the AV node First- second- and third-degree AV block |
| In the AV node Nodal ectopic beats Junctional rhythm Junctional tachycardia | In the bundle of His Left bundle branch block Right bundle branch block Left anterior and posterior hemiblocks |
| In the ventricles Ventricular ectopic beats Idioventricular rhythm Ventricular tachycardia Ventricular fibrillation | Others Intra-atrial block Ventricular pre-excitation Atrioventricular dissociation |
Consequences of cardiac dysrhythmias
 Impairment of circulation or myocardial oxygenation has consequences that are extremely variable but are more pronounced in the presence of cardiac disease.
Impairment of circulation or myocardial oxygenation has consequences that are extremely variable but are more pronounced in the presence of cardiac disease.
 The healthy heart can withstand many abnormal rhythms. The diseased heart cannot and sustained tachycardias may lead to circulatory collapse or ischaemic pain.
The healthy heart can withstand many abnormal rhythms. The diseased heart cannot and sustained tachycardias may lead to circulatory collapse or ischaemic pain.
Management of acute dysrhythmias aims:
Sinus bradycardia
 Sinus rhythm slower than 60 beats per minute during the day or 50 beats per minute in the night.
Sinus rhythm slower than 60 beats per minute during the day or 50 beats per minute in the night.
 Bradycardia occurs in about 30% of patients following MI.
Bradycardia occurs in about 30% of patients following MI.
 Normally indicates parasympathetic overactivity, with release of acetylcholine from autonomic fibres in the atria and AV node.
Normally indicates parasympathetic overactivity, with release of acetylcholine from autonomic fibres in the atria and AV node.
 Afferent vagal fibres are more common on the inferior surface of the heart and inferior MI is complicated more by this. Slowing of the heart is useful and protective in that it limits myocardial work but may result in hypotension secondary to a reduced output. Coronary perfusion may also be reduced.
Afferent vagal fibres are more common on the inferior surface of the heart and inferior MI is complicated more by this. Slowing of the heart is useful and protective in that it limits myocardial work but may result in hypotension secondary to a reduced output. Coronary perfusion may also be reduced.
 Usually symptomless but sudden onset of bradycardia may result in hypotension with dizziness or syncope.
Usually symptomless but sudden onset of bradycardia may result in hypotension with dizziness or syncope.
Junctional bradycardia
 If the sinus node fails to initiate an impulse and there are no other focuses in the atria, the AV junction takes over the pacemaker function.
If the sinus node fails to initiate an impulse and there are no other focuses in the atria, the AV junction takes over the pacemaker function.
 Most commonly occurs after acute MI, particularly if the patient is hypoxic or acidotic.
Most commonly occurs after acute MI, particularly if the patient is hypoxic or acidotic.
 Relatively slow (40–60 beats per minute) but sometimes may speed up and junctional tachycardia (>100) may occur.
Relatively slow (40–60 beats per minute) but sometimes may speed up and junctional tachycardia (>100) may occur.
Heart block
There are three forms of AV block:
 First-degree AV block where there is prolongation of the PR interval to no more than 0.22 s and every atrial depolarization is followed by delayed conduction to the ventricles.
First-degree AV block where there is prolongation of the PR interval to no more than 0.22 s and every atrial depolarization is followed by delayed conduction to the ventricles.
 Second-degree heart block where some P waves conduct and some do not. There are several forms – Mobitz I block (Wenckebach block), Mobitz II block and 2:1 or 3:1 (advanced) block where every second or third P wave conducts to the ventricles. The reader is referred to one of the more advanced medical texts in the Further Reading for more detail.
Second-degree heart block where some P waves conduct and some do not. There are several forms – Mobitz I block (Wenckebach block), Mobitz II block and 2:1 or 3:1 (advanced) block where every second or third P wave conducts to the ventricles. The reader is referred to one of the more advanced medical texts in the Further Reading for more detail.
 Third-degree (complete) AV block where all atrial activity fails to conduct to the ventricles. The electrical activity from the atria and ventricles is completely unrelated.
Third-degree (complete) AV block where all atrial activity fails to conduct to the ventricles. The electrical activity from the atria and ventricles is completely unrelated.
Ventricular standstill and asystole
 Occurs when impulses fail to reach the ventricles or impulse formation ceases.
Occurs when impulses fail to reach the ventricles or impulse formation ceases.
 If the problem is in the conduction system, atrial P waves may continue to occur.
If the problem is in the conduction system, atrial P waves may continue to occur.
 There will be no ventricular activity unless a ventricular pacemaker takes over.
There will be no ventricular activity unless a ventricular pacemaker takes over.
 The ventricles are left without electrical stimulation and ventricular standstill occurs.
The ventricles are left without electrical stimulation and ventricular standstill occurs.
 No cardiac output and cardiac arrest results.
No cardiac output and cardiac arrest results.
 More often, no electrical activity (either atrial or ventricular) is seen and the term asystole is used.
More often, no electrical activity (either atrial or ventricular) is seen and the term asystole is used.
This form of arrest has a poor prognosis and has several causes:
About 25% of arrests in hospital and 10% out of hospital are of this type. Mortality exceeds 90%.
Tachycardias
 An increase in rate is the normal response of the heart to increased work. This occurs so that cardiac output will increase.
An increase in rate is the normal response of the heart to increased work. This occurs so that cardiac output will increase.
 However, abnormal tachycardias are frequently associated with a diminished cardiac output.
However, abnormal tachycardias are frequently associated with a diminished cardiac output.
 Increase in heart rate is at the expense of diastole and the heart has less time to fill.
Increase in heart rate is at the expense of diastole and the heart has less time to fill.
 If ventricular filling is reduced, cardiac output will be reduced.
If ventricular filling is reduced, cardiac output will be reduced.
 Coronary blood flow takes place in diastole and therefore ischaemia may result.
Coronary blood flow takes place in diastole and therefore ischaemia may result.
 Symptoms provoked by tachycardia may include angina, dyspnoea, palpitations or syncope.
Symptoms provoked by tachycardia may include angina, dyspnoea, palpitations or syncope.
 Most tachycardias are produced by re-entry or enhanced automaticity.
Most tachycardias are produced by re-entry or enhanced automaticity.
 Narrow complex tachycardias include junctional tachycardias (SVTs), atrial flutter and atrial fibrillation.
Narrow complex tachycardias include junctional tachycardias (SVTs), atrial flutter and atrial fibrillation.
Atrial fibrillation
 One of the commonest cardiac arrhythmias.
One of the commonest cardiac arrhythmias.
 Affects approximately 1 in 20 of those over the age of 65 years in the UK.
Affects approximately 1 in 20 of those over the age of 65 years in the UK.
 Complicates 10–15% of MIs and is associated with a poor prognosis.
Complicates 10–15% of MIs and is associated with a poor prognosis.
 Normal atrial contraction is replaced by a series of irregular fibrillation waves (350–600/min) caused by multiple and changing micro re-entry circuits.
Normal atrial contraction is replaced by a series of irregular fibrillation waves (350–600/min) caused by multiple and changing micro re-entry circuits.
 Myocardial contraction is ineffective for atrial emptying and the atria remain functionally in diastole.
Myocardial contraction is ineffective for atrial emptying and the atria remain functionally in diastole.
 Reduces cardiac output by 10–20%.
Reduces cardiac output by 10–20%.
 Although AF makes the heart less efficient, the most important consequence is thromboembolism, especially stroke.
Although AF makes the heart less efficient, the most important consequence is thromboembolism, especially stroke.
 Patients with chronic atrial fibrillation are usually prescribed the anticoagulant warfarin in an attempt to prevent embolism and stroke.
Patients with chronic atrial fibrillation are usually prescribed the anticoagulant warfarin in an attempt to prevent embolism and stroke.
Sinus tachycardia
 Sinus rhythm greater than 100 and commonly between 100 and 150.
Sinus rhythm greater than 100 and commonly between 100 and 150.
 P waves are normal and have a 1:1 relationship with the QRS.
P waves are normal and have a 1:1 relationship with the QRS.
 Found in one-third of patients with MI – an attempt to maintain cardiac output when there is reduced stroke volume.
Found in one-third of patients with MI – an attempt to maintain cardiac output when there is reduced stroke volume.
 May be worsened by fear, pain or anxiety.
May be worsened by fear, pain or anxiety.
 Adequate analgesia will often settle this post-MI.
Adequate analgesia will often settle this post-MI.
 Mortality for those with MI is higher in sinus tachycardia than for those with sinus bradycardia.
Mortality for those with MI is higher in sinus tachycardia than for those with sinus bradycardia.
Ventricular dysrhythmias
 These include ventricular ectopics, ventricular tachycardia, ventricular flutter and ventricular fibrillation.
These include ventricular ectopics, ventricular tachycardia, ventricular flutter and ventricular fibrillation.
 Myocardial ischaemia predisposes to ventricular dysrhythmias as normal electrical conduction pathways may be disturbed.
Myocardial ischaemia predisposes to ventricular dysrhythmias as normal electrical conduction pathways may be disturbed.
 Myocardial irritability following an MI is the commonest cause of ventricular arrhythmias.
Myocardial irritability following an MI is the commonest cause of ventricular arrhythmias.
 Necrotic myocardial tissue is a focus for this ectopic activity.
Necrotic myocardial tissue is a focus for this ectopic activity.
 Predisposing factors following an MI include potassium imbalances or drugs.
Predisposing factors following an MI include potassium imbalances or drugs.
Ventricular tachycardia
There are four types of ventricular tachycardia (VT):
 The commonest is monomorphic VT and the complexes are of uniform appearance (monomorphic). Each episode of VT continues for a variable time and usually terminates in a long pause before sinus rhythm returns.
The commonest is monomorphic VT and the complexes are of uniform appearance (monomorphic). Each episode of VT continues for a variable time and usually terminates in a long pause before sinus rhythm returns.
 Polymorphic VT (torsades de pointes) is a dangerous dysrhythmia. The QRS undulates around the isoelectric line, with a marked change in amplitude every 5–30 beats. Episodes may be precipitated by drugs that prolong the QT interval or by electrolyte imbalances. Usually terminates spontaneously but may lead to VF.
Polymorphic VT (torsades de pointes) is a dangerous dysrhythmia. The QRS undulates around the isoelectric line, with a marked change in amplitude every 5–30 beats. Episodes may be precipitated by drugs that prolong the QT interval or by electrolyte imbalances. Usually terminates spontaneously but may lead to VF.
 Ventricular flutter is characterized by a rapid ventricular rate of about 180–250 beats. The ECG has been likened to a row of hairpins. It often precedes VF.
Ventricular flutter is characterized by a rapid ventricular rate of about 180–250 beats. The ECG has been likened to a row of hairpins. It often precedes VF.
 Accelerated idioventricular tachycardia is an escape rhythm which is slow, usually about 60 and not exceeding 120. After about 30 beats, sinus rhythm usually returns but may occasionally be replaced by sustained VT or VF.
Accelerated idioventricular tachycardia is an escape rhythm which is slow, usually about 60 and not exceeding 120. After about 30 beats, sinus rhythm usually returns but may occasionally be replaced by sustained VT or VF.
Ventricular fibrillation
 Electrically and mechanically, the heart is completely disorganized and cardiac arrest ensues.
Electrically and mechanically, the heart is completely disorganized and cardiac arrest ensues.
 The ECG shows fine and coarse waves of irregular size, shape and rhythm.
The ECG shows fine and coarse waves of irregular size, shape and rhythm.
 Fine VF may mimic asystole and produce an apparently flat line on the ECG.
Fine VF may mimic asystole and produce an apparently flat line on the ECG.
 About 90% of deaths following acute MI are due to VF. Nearly half occur in the first half hour.
About 90% of deaths following acute MI are due to VF. Nearly half occur in the first half hour.
 Primary VF is that which occurs in the first 12 hours after MI. Usually associated with a good prognosis as the heart is usually still functioning well.
Primary VF is that which occurs in the first 12 hours after MI. Usually associated with a good prognosis as the heart is usually still functioning well.
 Reperfusional VF may occur following thrombolysis, but this probably reflects a good prognosis as the infarct-related artery has been re-opened.
Reperfusional VF may occur following thrombolysis, but this probably reflects a good prognosis as the infarct-related artery has been re-opened.
 Secondary or late VF occurs when function has been severely compromised by the infarct and prognosis is poor.
Secondary or late VF occurs when function has been severely compromised by the infarct and prognosis is poor.
The Resuscitation Council (UK) has produced guidelines for the management of peri-arrest arrhythmias and these can be obtained from their website (www.resus.org.uk). They have been designed to allow the advanced life support provider to treat the patient effectively and safely in an emergency.





































































