CHAPTER 48. Child Abuse and Neglect
Angela Black
Child abuse and neglect affect children of all ages, ethnicities, genders, and socioeconomic groups. Approximately 1460 children died as a result of abuse in 2005 alone. 19 This figure may be conservative due to potential inaccurate determination of the manner and the cause of death. Several researchers suggest that deaths related to maltreatment are underreported by as much as 60%. 8.13. and 17. These tragic figures represent the death of approximately four children in the United States each day. Younger children experience the highest rate of fatalities: children under the age of 4 years account for three quarters (76.6%) of children killed as a result of child maltreatment. 19
In Chicago a 35-year-old mother kicks and throws her 16-month-old baby out a window because he will not stop crying; an Alabama couple shackles their twin daughters above the knees and locks them in a room to live in their own excrement; a Detroit drug addict sells her son to settle a $1000 crack cocaine debt; a trusted priest is sentenced to more than 30 years for sexually abusing children during his reign as youth leader; in California a teenage girl is abducted from her home and later found raped, beaten, and dead; a 4-year-old is beaten to death by her father while a neighbor reports she had to walk to another part of the house and turn up the television volume to drown out the child’s screams; a 3-year-old raped by a trusted family friend is left infected with Neisseria gonorrhoeae and human immunodeficiency virus (HIV); and in South Carolina, the drowning of two young boys at the hand of their mother horrifies the nation. Children are the future of our communities, and they must be protected; yet they are not able to protect themselves. Child abuse and neglect are a burden to society in many ways. Abused children are more likely to develop alcoholism, abuse drugs, and suffer from depression. Tragically, abused children often grow up to be abusive adults. There is also a significant financial burden. Annual direct costs related to child abuse exceed $24 billion, whereas annual indirect costs approach $70 billion. 20 Direct costs include hospitalization, the child welfare system, and the judicial system; indirect costs encompass special education, juvenile delinquency, and adult criminality.
In 2005 approximately 3.3 million incidents of suspected child abuse and neglect, involving approximately 6 million children, were reported to child protection services. 19 Reports of violence against children have almost tripled since 1976. The most common pattern of abuse is neglect, usually perpetrated by the female parent, whereas physical and sexual abuse is most often inflicted by a male acting alone. 20
More often than not, abused children present to the emergency department (ED) without a declaration of abuse or neglect. This, along with a false presentation of the history surrounding the child’s injury or illness, or a caregiver’s intentional withholding of information, leads to difficulty in identifying child maltreatment. A detailed history and thorough physical assessment are essential when identifying these small victims of maltreatment. The historical data and physical findings must be compared and evaluated to determine congruency. The interactions among the child, caregivers, and staff are also important to evaluate. Some behaviors that could indicate that the child is suffering from abuse or neglect are reviewed in Box 48-1.
Box 48-1

I ndicators of C hild A buse or N eglect
| Child | Caregiver |
|---|---|
Extreme change in behavior (regressive, passive, or overly aggressive) Flat affect Does not cry during painful procedures Appears malnourished, unkempt Sudden drop in school performance Sexual behavior toward adults or other children | No explanation or changing explanation for the child’s injury Explanation of injury does not match clinical findings Delay in seeking health care Uncooperative or hostile toward health care team Inappropriate response to the seriousness of the child’s condition |
NEGLECT
The lack of visible bruises or broken bones belies the fact that ongoing child neglect is a silent, serious attack on children that can leave lasting mental and physical problems. Currently 62.8% of all abuse cases involve neglect, and 42% of the deaths in 2005 were attributed to neglect. 19 Neglect, defined as intentional or unintentional omission of needed care and support, may appear to the emergency nurse as a child who is unkempt, left unattended, not dressed appropriately for the weather, malnourished, or diagnosed with “failure to thrive.” Identification of neglect must recognize parental attempts to provide essentials despite limited resources. Failure to provide adequate physical protection, nutrition, or health care is generally considered neglect, but neglect can also include lack of human contact and love. Recognizing neglect is often difficult in the ED because of limited, one-time contact with most patients. However, the emergency nurse should be alert for behaviors that suggest neglect (Box 48-2). Figure 48-1 depicts a case of neglect.
Box 48-2
P otential I ndicators of C hild N eglect
| Behavioral Findings | Physical Findings |
|---|---|
Begs or steals food Falls asleep in school, lethargic Poor school attendance, frequent tardiness Chronic hunger Dull, apathetic appearance Runs away from home Reports no caregiver in the home Assumes adult responsibilities | Height and weight significantly below normal for age level Inappropriate clothing for weather Poor hygiene, including lice, body odor, scaly skin Child abandoned and left with inadequate supervision Untreated illness or injury Lack of safe, warm, and sanitary shelter Lack of necessary medical and dental care |
From For kids sake: a child abuse prevention and reporting kit, rev ed, Oklahoma City, 1992, Oklahoma State Department of Health.
 |
| FIGURE 48-1 Neglect. An infant with severe failure to thrive has a badly neglected case of irritant diaper dermatitis. (From Zitelli BJ, Davis HW: Atlas of pediatric physical diagnosis, ed 4, St. Louis, 2002, Mosby.) |
Neglect can be physical, medical, educational, or emotional. Physical neglect accounts for the majority of child maltreatment in the United States. Physical neglect includes cases such as child abandonment, inadequate supervision, and failing to adequately provide for the child’s safety and physical and emotional needs. This type of neglect can lead to failure to thrive, malnutrition, serious illness, physical harm from injuries due to lack of supervision, and a lifetime of low self-esteem. 16 Medical neglect is the failure to provide appropriate health care for a child such as immunizations, recommended surgery, or other interventions necessary for a serious health problem. In some cases a parent may withhold traditional medical care because of religious beliefs. These cases generally do not fall under the definition of medical neglect; however, some states will intervene through the court system and force medical treatment for the child to save the child’s life or prevent life-threatening injury. Medical neglect can lead to poor overall health and compounded medical issues. 16 Educational neglect occurs when a child is allowed to engage in chronic absenteeism or is of mandatory school age but not enrolled in school or receiving needed special educational training. This can ultimately lead to inability to acquire necessary basic skills, dropping out of school, and continual disruptive behaviors. 16 Finally, emotional neglect is difficult to recognize and diagnose because of the lack of physical evidence. Emotional neglect is often typified by child behaviors such as depression, habit disorders (sucking, biting, rocking, enuresis), or conduct and learning disorders such as antisocial behaviors (e.g., cruelty). Emotional neglect includes actions such as chronic or extreme spousal abuse in the child’s presence, failure to provide needed psychologic care, belittling and withholding of affection. This can lead to poor self-image, alcohol or drug abuse, destructive behavior, and even suicide. 16
Failure to Thrive
Failure to thrive is defined as a condition in children younger than age 5 years whose growth persistently and significantly deviates from norms for age and sex based on national growth charts. Measurements for height, weight, and head circumference are plotted against normal childhood growth patterns. Failure-to-thrive children generally fall below average in all three areas. Actual weight less than 70% of predicted weight for length requires urgent attention. 5 The cause of failure to thrive may be organic, which is caused by a medical condition (e.g., Giardia organism infection, celiac disease, lead poisoning, malabsorption) or inorganic, caused by psychosocial issues.
Psychosocial causes are often linked to and reported as child neglect. Maladaptive parenting practices, chronic family illnesses, parental depression, and substance abuse among caregivers are recognized causes. Failure to thrive does not necessarily imply abuse or neglect but does require aggressive treatment and follow-up by appropriate health care professionals. Untreated, failure to thrive can lead to developmental and behavioral difficulties secondary to nutritional deprivation of the nervous system and other systems. A multidisciplinary approach in treating failure to thrive has the best opportunity for success. Family assessment, nutritional counseling, medical intervention, and family support are needed to correct failure to thrive.
The medical evaluation for suspected neglect and failure to thrive should include a thorough history, physical examination, feeding observation, and a home visit by a health care provider. The history should review the child’s family history, including genetic conditions, growth histories, endocrine disorders, caregivers’ knowledge of normal growth and development, family functioning, eating patterns, types of food available in the home, and family stressors. 5 The physical examination should include past and present growth parameters, including head circumference using appropriate growth charts. Along with a general examination, a careful neurologic examination and observation of the child’s developmental skills and interactive behaviors with parents is necessary. Laboratory and radiologic studies are frequently unnecessary, and the yield of positive laboratory data is less than 1%. 5Figure 48-2 illustrates a case of failure to thrive.
 |
| FIGURE 48-2 Psychologic failure to thrive as a result of neglect. A, This 4½-month-old infant was brought to the emergency department because of congestion, where she was found to be below her birth weight and to be suffering from severe developmental delay. Note the marked loss of subcutaneous tissue manifested by the wrinkled skin folds over her buttocks, shoulders, and upper arms. (From Zitelli BJ, Davis HW: Atlas of pediatric physical diagnosis, ed 4, St. Louis, 2002, Mosby.) |
PHYSICAL ABUSE
Physical abuse is intentional injury to a child younger than age 18 years by a parent or caregiver. Of the four types of child maltreatment, physical abuse is second to neglect, accounting for approximately 17% of all abuse cases. 19 In 2004, 152,250 children were confirmed victims of physical abuse in the United States. 6 It is estimated that the rate of physical abuse in children with disabilities is 2.1 times greater than for children without disabilities. Despite these statistics, physical abuse remains underreported for several reasons, including individual and community variations in what is considered abuse, inadequate knowledge among professionals in recognition of abusive injuries, and unwillingness to report suspected abuse. 6 Child abuse is typically a pattern of behavior repeated over time, but it can also be a single attack. The condition is characterized by injury, torture, maiming, or use of unreasonable force. Abuse may result from harsh discipline or severe punishment. Box 48-3 identifies behavioral and physical indicators found in physical abuse. Children rarely tell anyone about physical abuse because of feelings of shame or confusion. They may also fear breaking up their family, isolation, or threats from the abuser. 1
Box 48-3




Get Clinical Tree app for offline access
P hysical A buse F indings
| Behavioral Findings | Physical Findings |
|---|---|
Requests or feels deserving of punishment Afraid to go home, or requests to stay in school or daycare Overly shy, tends to avoid physical contact with adults, especially parents Displays behavioral extremes (withdrawal or aggressiveness) Cries excessively or sits and stares Reports injury by parent or caretaker Gives unbelievable explanations for injuries Clings to health care worker rather than parent | Unexplained bruises or welts found most frequently, usually on face, torso, buttocks, back, or thighs; can reflect shape of object used (e.g., electric cord, hand, belt buckle); may be in various stages of healing Unexplained burns often on palms, soles of feet, buttocks, or back; can reflect pattern of cigarette burn, electrical appliance, or rope burn Unexplained fractures or dislocations involving skull, ribs, and bones around joints; may include multiple fractures or spiral fractures Other unexplained injuries such as lacerations, abrasions, human bite, or pinch marks; loss of hair or bald patches; retinal hemorrhages; abdominal injuries |
Modified from For kids sake: a child abuse prevention and reporting kit, rev ed, Oklahoma City, 1992, Oklahoma State Department of Health.
Skin Injuries
In contrast to unintentional injuries, inflicted injuries tend to occur on surfaces other than bony prominences such as the head, trunk, upper arms, buttocks, and backs of the thighs. Location, size, and shape of bruises, lacerations, burns, or bites should be documented in the medical record accompanied by high-quality photographs. 6 Measurement of skin injuries will help in determining the mechanism of injury, as well as the object used to inflict the injury. Bite marks should be carefully measured and photographed if possible. Referral to professionals that can gather specific forensic information is ideal. Causes of burn injuries may be chemical, thermal, or electrical. The history and continuity of the burn pattern may indicate a greater probability of inflicted trauma. Unintentional scalds commonly involve hot liquids that are pulled or splashed onto the child’s head, torso, and upper extremities. Inflicted injuries will be sharply demarcated with few or no splash marks.
Cranial Injuries
Head trauma is the leading cause of death for victims of child abuse. 6 Inflicted injuries tend to occur in younger children. Abuse should be suspected in infants with a history of a minor head trauma, such as a short fall off a sofa, presenting with multiple, complex, or occipital skull fractures. A funduscopic examination for retinal hemorrhages should be performed in any infant who is a suspected victim of physical abuse. Retinal hemorrhages occur in approximately 85% of infants who are subjected to abusive shaking with or without impact. 6
Skeletal Injuries
Skeletal fractures are common in childhood, leading to difficulty determining whether a fracture is unintentional or inflicted. Fractures that are particularly suspicious for abuse include multiple fractures in different stages of healing, long-bone fractures including metaphyseal fractures, spiral/oblique fractures, and bilateral or symmetric fractures. If a fracture is suspected, the skin should be carefully assessed for grab marks; however, the absence of bruising does not exclude an abusive mechanism of injury. Rib fractures in infants are usually caused by forceful squeezing of the chest. Posterior or lateral rib fractures or multiple rib fractures are especially predictive of abusive trauma. 6
Specific Abuse Patterns
Children can experience a multitude of insults and injuries at the hands of primary caregivers or other adults. Two patterns seen with increasing frequency are shaken baby syndrome (SBS) and Munchausen syndrome by proxy (MSP) (also referred to as factitious disorder by proxy).
SBS occurs when infants are shaken vigorously. Approximately 1500 cases of SBS occur each year in the United States; however, the true number of cases is unknown due to misdiagnosis and underreporting. 14 According to the American Academy of Pediatrics, SBS is a violent form of abuse that occurs in infants younger than 2 years but can involve children as old as 5 years. 2. and 15. Acceleration-deceleration of the head creates a triad of injuries: subdural hemorrhage (Figure 48-3), retinal hemorrhage (Figure 48-4), and altered level of consciousness. There are often no external signs of trauma. Babies shaken into unconsciousness are often put to bed in hopes the injuries will resolve; therefore the window for therapeutic intervention is lost. The spectrum of symptoms may vary from vomiting and irritability in mild shakings to unconsciousness, convulsions, and even death in severe shakings. A funduscopic examination of the pupils should be performed to look for retinal hemorrhages. Pupil dilation may be required in some patients. A computed tomography scan should be obtained to identify brain hemorrhages. Magnetic resonance imaging, when available, is extremely helpful for detection of subdural hematoma. A skeletal survey should be obtained to rule out fractures, especially in the area of the ribs. The diagnosis of SBS is made following a thorough history of the circumstances of the injury(s), pattern of injury, and social context in which they occur. Recent legal and medical controversies over SBS have led to questions regarding its diagnosis and even its existence. The controversies concern the precise cause of brain injury and the retinal and subdural hemorrhages, the degree of force required, and whether impact in addition to acceleration-deceleration forces is needed.
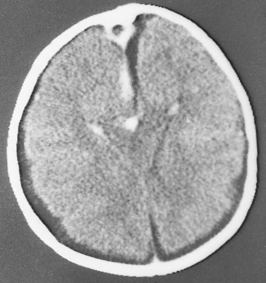 |
| FIGURE 48-3 Subdural hematoma secondary to shaken baby syndrome. (From Zitelli BJ, Davis HW: Atlas of pediatric physical diagnosis, ed 4, St. Louis, 2002, Mosby. Courtesy the Division of Neuroradiology, University Health Center of Pittsburgh.) |
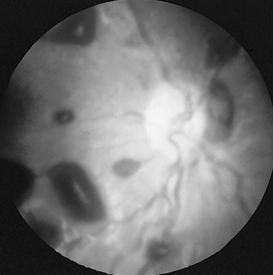 |
| FIGURE 48-4 Retinal hemorrhages secondary to shaken baby syndrome. (From Zitelli BJ, Davis HW: Atlas of pediatric physical diagnosis, ed 4, St. Louis, 2002, Mosby. Courtesy Dr. Stephen Ludwig, Children’s Hospital of Philadelphia.) |
MSP is a complex condition in which a parent, usually the mother, knowingly keeps a child ill or fabricates an illness for secondary gain or attention through the child’s illness. The child is subjected to illnesses perpetuated by caregivers who may administer emetics, laxatives, or other drugs, introduce pathogens, or otherwise contribute to a child’s illness. Commonly seen signs and symptoms of MSP include apnea, seizures, vomiting, diarrhea, simulated or actual hemorrhage, bacteremia, rash, and fever. 9 The history provided is often sophisticated and elaborate. The parent often demands extensive medical evaluations and appears very concerned for the child. The child’s history may also include the parent’s seeking health care at multiple locations and from multiple physicians. Often undetected by health care professionals, MSP can lead to emotional problems, chronic disabilities, and death.
One difficulty in identifying abuse is the number of conditions that mimic physical abuse. Physiologic or pathologic causes for physical findings should always be considered. 7
• Sudden infant death syndrome can appear as child abuse because of pooling of blood, mottling, and other discoloration associated with death. The definitive cause of death should be determined by a complete autopsy with appropriate ancillary studies, a review of clinical findings, and a scene investigation.
• Disorders such as erythema multiforme, Henoch-Schönlein purpura, leukemia, Wiskott-Aldrich syndrome, hemophilia, and idiopathic thrombocytopenic purpura can cause bruising or lesions resembling burns.
• Mongolian spots are benign bluish gray birthmarks found predominantly in African Americans, Hispanic Americans, Asians, Latinos, Native Americans, or anyone with dark pigmentation. Mongolian spots are usually located over the sacral area and buttocks but may also be located on the legs, shoulders, upper arms, and face.
• Multiple petechiae and purpuric lesions of the face can occur when vigorous crying, retching, or coughing increases vena caval pressure. Unlike intentional choking, there are no marks around the neck.
• Bullous impetigo may appear as an infected wound or burn. This condition may reflect neglect if caregivers are apathetic about care of lesions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
