CHAPTER 45. Ocular Emergencies
Darcy Egging
According to the National Hospital Ambulatory Medical Care Survey: 2004 Emergency Department Summary, approximately 3.6 million individuals present to the ED annually with complaints related to the eyes or ears. This number is approximately 11% of all ED visits. Of the 3.6 million visits, 1.6 million are for traumatic eye injuries according to the 2004 report. 28 The typical ocular emergencies treated in the ED include corneal or conjunctival foreign body, conjunctivitis, and corneal abrasion. These conditions do not cause significant morbidity; however, the patient does experience discomfort and disruption of routine. True ocular emergencies, those conditions with potential for vision loss, include chemical burns, angle-closure glaucoma, globe rupture, and retinal artery occlusion.
ANATOMY AND PHYSIOLOGY
The eyes are the windows to the world. Vision is often considered the most important of the five senses. Basic understanding of ocular structures facilitates assessment and treatment of ocular problems. Figure 45-1 illustrates these ocular structures. The eyes are protected by the surrounding bony structures, eyelids, and sclera. Lacrimal glands secrete tears, which continuously bathe the eye to decrease friction and remove minor irritants. Meibomian and Zeis glands are sebaceous glands that line the eyelid margins and prevent tears from evaporating and running out of the conjunctival sacs.
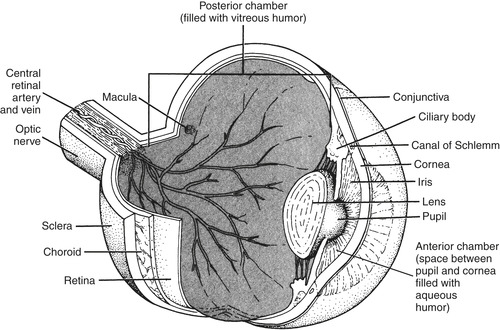 |
| FIGURE 45-1 Anatomy of the eye. |
Light enters the eye through the cornea, passes through the lens, and is reflected off the retina. The amount of light entering the posterior chamber is controlled by the iris as it expands and contracts to open and close the pupil. Six oculomotor muscles control movement of the eye itself.
PATIENT ASSESSMENT
Assessment of the patient with an ocular problem begins with triage and continues into the treatment area. A potential threat to vision should be triaged as emergent, whereas a patient with a reddened eye and no potential for loss of vision could be triaged as nonurgent if no other problems exist.
After a brief assessment to ensure that the airway, breathing, and circulation (ABCs) are stable, the patient is evaluated to identify potential threats to vision. Focused assessment includes determination of precipitating events, duration of symptoms, and identification of anything that worsens or improves symptoms. When the patient verbalizes discomfort, description of the discomfort helps clarify the patient’s problem. Does the patient describe itching, burning, or the sensation of something in the eye? Determine the degree of pain and where the pain occurs. Clarify reported visual changes to determine if the loss is partial or complete, and in one or both eyes. Biocular changes suggest a neurologic condition rather than an ocular condition, whereas the presence of floaters suggests retinal tear.
When the patient has a history of trauma, determine the mechanism of injury and when it occurred. If the injury occurred as a result of a motor vehicle crash, did the air bag deploy? Injuries associated with air-bag deployment include orbital fractures, retinal detachment, hyphema, and globe rupture; an increased incidence of globe rupture and hyphema has been noted in older adults. 40 The alkaline powder in air bags can also cause significant eye irritation. 46 Question the patient regarding use of protective eyewear, glasses, or contact lenses. Evaluate medical history, including ocular history, use of corrective lenses, ocular medications, past ocular surgery, and disease such as diabetes. Tetanus status should be determined if signs of ocular trauma are noted.
The primary elements of the ocular examination for all patients are visual acuity and evaluation of external features, pupils, anterior segment, and extraocular movement (EOM). 1. and 20. The physician may perform a slit-lamp examination, intraocular pressure (IOP) measurement, and direct ophthalmoscope examination.
Visual Acuity
Visual acuity is a “vital sign” for patients with an ocular concern. This simple test is done on all patients presenting with any type of eye or vision complaint. 1.20. and 24. Physical examination begins with visual acuity unless the patient has sustained ocular exposure to a chemical. In these situations irrigation takes priority over determination of visual acuity. 1.2.4.24. and 30. Measure visual acuity both with and without the patient wearing corrective lenses. When corrective lenses are not available, the pinhole test can be used for measurement of visual acuity. This is accomplished by punching a hole in a note card with an 18-gauge needle. Looking through a pinhole usually corrects any refractory error to at least 20/30. 29. and 31. Test the affected eye first, then the unaffected eye, and finally both eyes. The Snellen chart is the standard method for determination of visual acuity. For the examination, have the patient stand 20 feet from the chart and cover the eye without applying pressure to the orbit. Alternative techniques for visual acuity when a Snellen chart is not available are using a pocket vision screener held 14 inches from the nose or having the patient read a newspaper and record the distance at which the paper must be held for the patient to read. If the patient is unable to read, hold fingers up, record the distance at which the patient can see your fingers, then ask the patient how many fingers you are holding up. If the patient cannot see fingers moving; record the distance at which the patient perceives hand motion. If unable to see hand motion, is the patient able to perceive light?Table 45-1 describes documentation of visual acuity for the Snellen chart and alternative techniques for reporting visual acuity. For people who are illiterate or do not speak English, there is an E chart where the patient indicates the direction of the letter E. The Allen card of objects is used for children. Be sure to name the objects before the test so that they are identified correctly. The patient with a corneal abrasion or foreign body may have difficulty with photophobia, pain, and tearing. Placing a drop of topical anesthetic in the affected eye may assist in accomplishing an accurate visual acuity in these patients. 25
| 20/20 | Standing at 20 feet, patient can read what the normal eye can read at 20 feet. |
| 20/20 2 | Standing at 20 feet, patient can read what the normal eye can read at 20 feet; however, missed two letters. |
| 20/200 | At 20 feet, patient can read what the normal eye can read at 200 feet. Patient is considered legally blind if reading is obtained while wearing glasses or contact lenses. |
| 10/200 | When the patient cannot read letters on the Snellen chart, have patient stand half the distance to the chart. Record findings at the distance the patient is standing from the chart over the smallest line he or she can read. |
| CF/3 ft | Patient can count fingers at a maximum distance of 3 feet. |
| HM/4 | Patient can see hand motion at a maximum distance of 4 feet. |
| LP/position | Patient can perceive light and determine the direction from which it is coming. |
| LP/no position | Patient can perceive light but is unable to tell the direction from which it is coming. |
| NLP | Patient is unable to perceive light. |
External Features
External examination of ocular complaints begins by inspecting the patient. Observe for bruising, lacerations, lesions, and other differences between the eyes. Assess eyelids, lashes, and how the eyes rest in the socket. Examine the conjunctiva and sclera for abnormal color.
Pupil Examination
Pupil examination includes assessment of shape, size, and reactivity. Testing should be performed in a dimly lit examination room. Pupils are normally round, black, and equal in size. Variations may indicate a potentially serious problem or may reflect a normal physiologic variation. Up to 20% to 25%13 of the population have unequal pupils (physiologic anisocoria) as a normal finding. 7 Physiologic anisocoria is a normal finding when the difference in pupils is 1 mm or less and both pupils react briskly to light. 41 An oval pupil may be caused by a tumor or retinal detachment. A pupil that is the shape of a teardrop suggests a ruptured globe, with the teardrop pointing to the rupture site. 24 Pupil size is measured in millimeters. Assess and document the change in size that occurs in each pupil in response to direct and consensual light stimulation. Normally both pupils constrict equally when a strong light is directed at one eye (direct response in eye to which light is directed and consensual response of the other eye). 24
Anterior Segment
The anterior segment is composed of the sclera, conjunctiva, cornea, anterior chamber, iris, lens, and ciliary body. 20 The conjunctiva or the white of the eye should be inspected for changes in color, swelling (chemosis), discharge, foreign bodies, and laceration. The cornea should be clear. The cornea is stained with fluorescein to inspect for the presence of any abrasions. The anterior chamber is inspected for hyphema (blood in the anterior chamber) or hypopyon (pus in the anterior chamber). To inspect the anterior chamber, hold a light tangential or at a 90-degree angle to the eye. A slit lamp is used to perform an adequate assessment of the anterior chamber. 20. and 25.
Ocular Motility
Evaluate the patient’s ability to move the eyes through six cardinal positions of gaze by asking the patient to follow your finger as you move it through these positions. Ocular movement is controlled by the cranial nerves that regulate the oculomotor muscles. Figure 45-2 shows these positions of gaze and identifies the specific oculomotor muscles and cranial nerves involved. Impaired ocular movement may occur with an entrapped muscle secondary to a blowout fracture, muscular injury, orbital cellulitis, or underlying central nervous system problem. Evaluation of ocular motility in children requires patience and creativity. Hold toys, keys, or lights in different areas so that the child glances in that direction. Children become easily bored with the same object, so a general rule of thumb is to use a different toy for each position. 24. and 29.
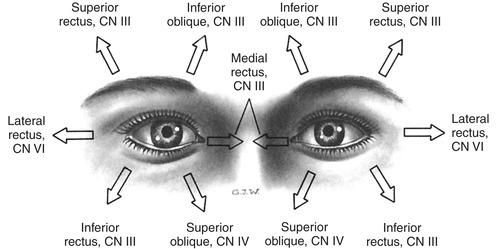 |
| FIGURE 45-2 Innervation and movement of extraocular muscles. CN, Cranial nerve. (From Thompson JM, McFarland GK, Hirsch JE et al: Mosby’s clinical nursing, ed 5, St. Louis, 2002, Mosby.) |
Other Examinations
Other techniques used to evaluate ocular function include fluorescein staining, measurement of IOP, and funduscopic examination. Fluorescein is used to determine if the corneal epithelium is intact. Before staining, the patient should remove his or her contact lenses. Explain the procedure to the patient. Moisten end of a sterile fluorescein strip with normal saline solution. Pull down on the lower lid and touch the moistened fluorescein strip to the inner canthus of the lower lid. Ask the patient to blink several times before examining the patient with a cobalt blue light; disruptions of the corneal epithelium appear as a bright yellow spot. Following fluorescein application, flush the eye with normal saline and instruct the patient not to insert contact lenses for at least 3 to 5 hours. 34
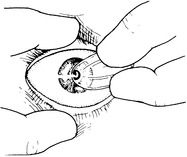
IOP is measured with a Schiøtz tonometer (Figure 45-3) or a Tono-Pen. This procedure is contraindicated in patients with possible globe rupture. The Tono-Pen is a handheld instrument that has gained popularity because of its ease of use and decreased incidence of contamination; the tip is covered with a sterile cover that is discarded after each patient. Regardless of technique, the cornea must be anesthetized before measurement. Normal IOP is 10 to 21 mm Hg. A low reading indicates decreased IOP, whereas a high reading indicates increased IOP. Any obstruction to aqueous outflow, such as glaucoma, can result in an elevated IOP. 25.29. and 34.
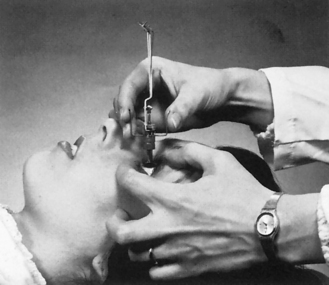 |
| FIGURE 45-3 Measurement of ocular tension with Schiøtz tonometer. (From Newell FW: Ophthalmology: principles and concepts, ed 8, St. Louis, 1996, Mosby.) |
Direct ophthalmoscopy, or funduscopic evaluation, is used to evaluate the posterior chamber of the eye using a light beam directed through the pupil. 20 Mydriatic drops may be administered to dilate the pupil and make visualization of the disc, retinal artery, and macula easier; however, they are contraindicated in patients who have sustained a head injury. 25 Ophthalmoscopes provide different shapes and colored light beams to assist in detecting various abnormalities.
PATIENT MANAGEMENT
General management of ocular emergencies includes removal of contact lens, instillation of ocular medication, irrigation, and eye patching.
Figure 45-4 illustrates removal of hard contacts; Figure 45-5 illustrates soft contact removal.
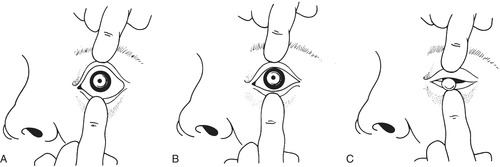 |
| FIGURE 45-4 Technique for removing hard corneal contact lens from eye. A, Spread eyelids apart. B, Push lids toward center of eye under contact lens. C, Remove lens. |
 |
| FIGURE 45-5 Soft contact lens removal. Lift lens off cornea. |
Eye drops and ophthalmic ointments are used to decrease pain, provide antibiotic therapy, change pupil size, reduce allergic reactions in the eye, and cleanse the eye. Topical ophthalmic medications are prepared under sterile conditions and distributed in single-dose containers. Container caps are color coded by the medication’s effect on the pupil. For example, a red cap indicates a mydriatic (pupil dilating) medication, green for a pupil constrictor (miotic); white is for a topical anesthetic, blue an irrigating or lubricating agent, and a yellow cap denotes medications that decrease aqueous humor production.
Instilling eye drops or ointments requires attention to detail to prevent contamination and minimize systemic effects of the medication. Before instilling eye drops or ointments, explain the procedure to the patient, and place the patient in the supine position. Instruct the patient not to roll his or her eyes because this can worsen injury, particularly when anesthetic drops have been used; topical anesthetics may be used to facilitate the examination but should not be prescribed for continuous use because these agents retard epithelial healing. Instillation of eye drops and ointments are relatively easy procedures to master; in both instances have the patient gaze upward because this will help to ensure that the patient does not blink at an inopportune time. Pull the lower eyelid downward and instill the medication in the conjunctival sac. Monitor patients carefully following instillation of eye drops; systemic effects secondary to eye drops may occur. These systemic effects can be minimized by instructing patients to apply pressure to the medial canthus for several minutes after medication instillation to close the nasolacrimal duct. If more than one type of drop is ordered, wait several minutes between applications to allow maximal exposure for each drop.
Irrigation is used to remove chemicals, small foreign bodies, and other substances. Isotonic saline or lactated Ringer’s are the fluids of choice for ocular irrigation. 25.32. and 38. Dextrose solutions should not be used because they are sticky and irritate the eye. Irrigation is contraindicated in the patient with a possible ruptured globe. There is no documented literature on the correct length of tubing to be used; however, the shorter the tubing, the faster the flow. Before irrigating the eye, make sure the outer aspects of the eye are cleansed so that additional debris does not inadvertently contaminate the eye and cause further problems. When using intravenous tubing to irrigate, gently separate the eyelids and have the patient look around while the irrigant is flowing. Sweep from the inner to the outer canthus. Occasionally allow the patient to blink for comfort. A Morgan Lens can also be used for irrigation. In the case of a chemical exposure, a baseline pH measurement of the eye should be obtained by placing pH paper in the conjunctival sac before irrigation is initiated. Irrigation is continued until the pH of the tear film is neutral (normal conjunctival pH is 7.1). As a rule of thumb, for acidic chemical exposure 1 L of fluid will be necessary, whereas exposure to an alkali will require a minimum of 2 L of fluid. 25. and 32.
Eye patching is performed to minimize ocular stimulation by reducing movement and limiting light exposure. A common intervention in the past, this procedure is currently not being used for routine management of uncomplicated corneal injuries because evidence does not support its use. 25 A Cochrane review of the literature shows that patching of a simple corneal abrasion does not increase healing time nor does it decrease pain. 36 Patching of both eyes simulates total blindness; patching one eye alters depth perception. Eye patches should not be used when there is an increased risk for a Pseudomonas organism infection, for example, in the contact lens wearer. Although not widely available in the ED, a collagen shield that is similar to a contact lens is being used by ophthalmologists for corneal erosions. 25. and 33. The correct method of patching the eye includes asking the patient to gently close both eyes and placing a folded eye pad over the affected eye followed by an unfolded eye pad. The eye pad is taped obliquely, ensuring that the entire eye patch is covered. Ask the patient if he or she can blink under the pad: if the patient is able to blink, the patch has not been applied correctly. When the patient is discharged with an eye patch, discharge instructions must include discussion of altered vision and the hazards of driving or using machinery. Eye patches should not be applied for more than a 24-hour period; therefore follow-up is essential. 33
SPECIFIC OCULAR EMERGENCIES
Injury or disease may cause ocular emergencies. Comprehensive discussion of every disease process is beyond the scope of this text; however, situations encountered most often by the emergency nurse are discussed.
Trauma
General principles pertaining to ocular examination are essentially the same for the patient with an eye injury; however, the patient’s ABCs should be evaluated and stabilized before interventions for the ocular problem. Ocular injury often occurs in conjunction with head and facial trauma; therefore these patients should be carefully evaluated for an associated eye injury. Check for contact lenses in the unconscious patient, and remove them as soon as possible. Do not instill eye drops before evaluation of ocular injury. Severe pain associated with ocular trauma can be minimized without medication by patching both eyes. When the patient cannot blink, protect the cornea from drying with ophthalmic ointment or artificial tears. The eyes may be taped shut when ointment is used.
Obtain pertinent details of history, including mechanism of injury, time of injury, energy source, material involved when there is ocular penetration, and use of protective eyewear. If the foreign material is organic, there is increased risk for infection, whereas metallic materials cause vitreous and ocular reactions.
Blunt Trauma
Blunt trauma to the eye may be caused by a motor vehicle collision, assault with various weapons, or a fall. The most commonly seen ocular injury is periorbital contusion or a black eye. This injury is usually benign, but the patient should be assessed for more serious injury, such as a hyphema or basilar skull fracture. Symptoms usually include ecchymosis of the lids, which can make it very difficult to visualize the globe. If the globe appears intact, rule out orbital fracture and hyphema. If no obvious associated problems are identified, therapeutic interventions such as ice, head elevation, and reassurance are initiated. Resolution of noncomplicated periorbital ecchymosis usually occurs within 2 to 3 weeks. 29
ORBITAL FRACTURES
Orbital fractures involve the orbital floor and the orbital rim. A fracture of the orbital floor, sometimes called a blowout fracture, is serious and usually results from direct blunt trauma to the eye. A blowout fracture occurs when direct trauma increases IOP to the point where the orbital floor fractures. Orbital contents may herniate into the maxillary or ethmoid sinuses and trap the inferior rectus muscle in the defect. A blowout fracture is diagnosed by history and observation of periorbital ecchymosis, subconjunctival hemorrhage, periorbital edema, enophthalmos (sunken eye), an upward gaze, and a complaint of diplopia. 24 The latter three conditions occur when the inferior rectus and oblique muscles are trapped in the fracture. Computed tomography (CT) scan is most often used for the diagnosis of orbital fractures; facial radiographs are rarely used. Magnetic resonance imaging (MRI) is not generally used in acute orbital trauma and is contraindicated if there is a possibility of a metallic foreign body. CT or MRI is more helpful in identification of entrapment than plain radiographs. 24. and 29.
Orbital fractures are not considered an ocular emergency unless visual impairment or globe injury is present. Surgical intervention is usually delayed until swelling resolves in 7 to 10 days. Patients without eye injury or entrapment may be referred to an ophthalmologist and treated conservatively. Patients who have fractures involving the sinuses should receive a prescription of antibiotics. Discharge instructions should include ice and cautions against Valsalva maneuvers, sneezing, and nose blowing (activities that increase IOP). 24.29. and 42.
HYPHEMA
Hyphema refers to bleeding into the anterior chamber of the eye, usually secondary to blunt trauma (Figure 45-6). It occurs when blood vessels of the iris rupture and leak into the clear aqueous fluid of the anterior chamber. 43 Hyphema size varies from microscopic to total involvement of the anterior chamber. The term “eight-ball hyphema” describes a total hyphema that has begun to clot. 18 A large clot can obstruct aqueous outflow and lead to secondary glaucoma. Any patient with a hyphema requires evaluation by an ophthalmologist.
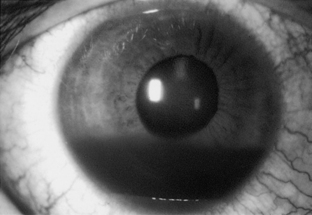 |
| FIGURE 45-6 Traumatic hyphema. (From Abrams D: Ophthalmology in medicine: an illustrated clinical guide, St. Louis, 1990, Mosby.) |
Symptoms of hyphema include pain, photophobia, and blurred vision. Blood in the anterior chamber may be easily seen in patients with lighter-colored eyes but may be extremely difficult to see in dark-eyed patients. Suspect concurrent head injury if the patient has an altered level of consciousness. Patients with bleeding disorders, anticoagulant therapy, kidney disease, liver disease, or sickle cell disease have an increased risk for complications; therefore these patients should be monitored carefully for increased bleeding. The most common complication of hyphema is rebleeding, which occurs in 30% of patients, usually within 2 to 5 days, but can occur up to 14 days after the initial injury. 18.29. and 39. Other complications include corneal blood staining, secondary glaucoma, loss of vision, and loss of the eye.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
