Drugs Used to Treat Glaucoma and Other Eye Disorders
Objectives
1 Describe the anatomy and physiology of the eye.
2 Describe the normal flow of aqueous humor in the eye.
3 Identify the changes in normal flow of aqueous humor caused by open-angle and closed-angle glaucoma.
4 Explain patient assessments needed for eye disorders.
6 Compare the mechanisms of action of drugs used to lower intraocular pressure.
Key Terms
cornea ( ) (p. 678)
) (p. 678)
sclera ( ) (p. 678)
) (p. 678)
iris ( ) (p. 678)
) (p. 678)
sphincter muscle ( ) (p. 678)
) (p. 678)
miosis ( ) (p. 678)
) (p. 678)
dilator muscle ( ) (p. 678)
) (p. 678)
mydriasis ( ) (p. 678)
) (p. 678)
lens ( ) (p. 678)
) (p. 678)
near point ( ) (p. 678)
) (p. 678)
zonular fibers ( ) (p. 678)
) (p. 678)
cycloplegia ( ) (p. 678)
) (p. 678)
lacrimal canaliculi ( ) (p. 679)
) (p. 679)
intraocular pressure (IOP) ( ) (p. 680)
) (p. 680)
closed-angle glaucoma ( ) (p. 680)
) (p. 680)
open-angle glaucoma (p. 680)
Anatomy and Physiology of the Eye
![]() http://evolve.elsevier.com/Clayton
http://evolve.elsevier.com/Clayton
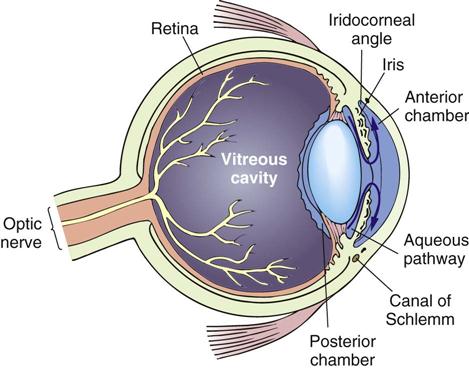
The eyeball has three coats, or layers: the protective external, or corneoscleral coat; the nutritive middle vascular layer, called the choroid; and the light-sensitive inner layer, or retina (Figure 43-1).
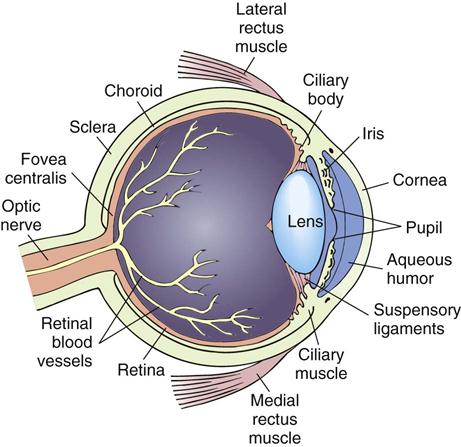
The cornea, or outermost sheath of the anterior eyeball, is transparent so that light can enter the eye. The cornea has no blood vessels; it receives its nutrition from the aqueous humor and its oxygen supply by diffusion from the air and surrounding vascular structures. There is a thin layer of epithelial cells on the external surface of the cornea that is resistant to infection. An abraded cornea, however, is highly susceptible to infection. The cornea has sensory fibers, and any damage to the corneal epithelium will cause pain. Seriously injured corneal tissue is replaced by scar tissue that is usually not transparent. The sclera is the eye’s white portion that is continuous with the cornea and is not transparent. The pupil is the center black portion of the eye, which is actually a hole in the iris that allows light to reach the retina.
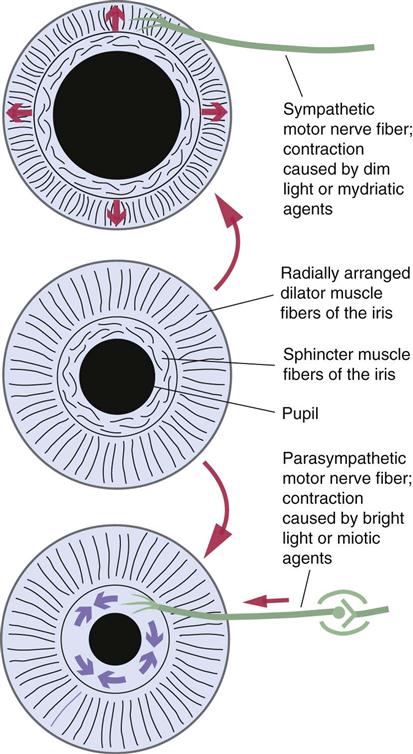
The iris is a diaphragm that surrounds the pupil and gives the eye its color—blue, green, hazel, brown, or gray. The sphincter muscle within the iris encircles the pupil and is innervated by the parasympathetic nervous system. Miosis is contraction of the iris sphincter muscle, which causes the pupil to narrow. The dilator muscle, which runs radially from the pupillary margin to the iris periphery, is sympathetically innervated. Mydriasis is contraction of the dilator muscle and relaxation of the sphincter muscle, which causes the pupil to dilate (Figure 43-2).
Constriction of the pupil normally occurs with light or when the eye is focusing on nearby objects. Dilation of the pupil normally occurs in dim light or when the eye is focusing on distant objects.
The lens is a transparent gelatinous mass of fibers encased in an elastic capsule situated behind the iris. Its function is to ensure that the image on the retina is in sharp focus. It does this by changing shape (accommodation). This occurs readily in youth, but with age the lens becomes more rigid and the ability to focus close objects is lost. The near point, the closest point that can be seen clearly, recedes. With age, the lens may lose its transparency and become opaque, forming a cataract. Blindness can occur unless the cataract can be treated or surgically removed.
The lens has ligaments around its edge, called zonular fibers, which connect with the ciliary body. Tension on the zonular fibers helps change the shape of the lens. In the unaccommodated eye, the ciliary muscle is relaxed and the zonular fibers are taut. For near vision, the ciliary muscle fibers contract, relaxing the pull on the ligaments and allowing the lens to become thick. Accommodation depends on two factors: (1) the ability of the lens to assume a more biconvex shape when tension on the ligaments is relaxed and (2) ciliary muscle contraction. Paralysis of the ciliary muscle is termed cycloplegia. The ciliary muscle is innervated by parasympathetic nerve fibers.
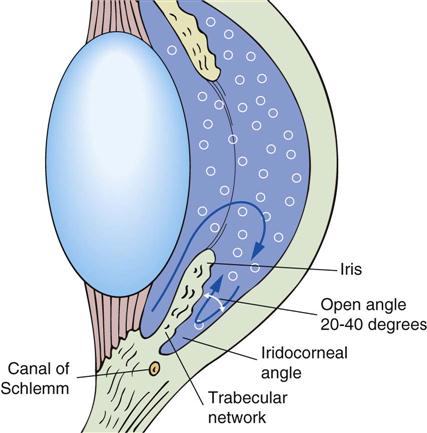
The ciliary body secretes aqueous humor, which bathes and feeds the lens, posterior surface of the cornea, and iris. After it is formed, the fluid flows forward between the lens and the iris into the anterior chamber. It drains out of the eye through drainage channels located near the junction of the cornea and sclera into a meshwork that leads into Schlemm’s canal and into the venous system of the eye.
Eyelids, eyelashes, tears, and blinking all protect the eye. There are about 200 eyelashes for each eye. The eyelashes cause a blink reflex whenever a foreign body touches them, closing the lids for a fraction of a second to prevent the foreign body from entering the eye. Blinking, which is bilateral, occurs every few seconds during waking hours. It keeps the corneal surface free from mucus and spreads the lacrimal fluid evenly over the cornea. Tears are secreted by lacrimal glands and contain lysozyme, a mucolytic lubrication for lid movements. They wash away foreign agents and form a thin film over the cornea, providing it with a good optical surface. Tear fluid is lost by drainage into two small ducts, the lacrimal canaliculi, at the inner corners of the eyelids and by evaporation.
General Considerations for Topical Ophthalmic Drug Therapy
The most common route of administration for ophthalmic drugs is topical application. Advantages include convenience, simplicity, noninvasive nature, and the ability of the patient to self-administer. Topically administered medications do not penetrate adequately for use with posterior eye diseases, so topical administration is not used for such diseases as with the optic nerve or retina.
Proper administration is essential to optimal therapeutic response. The administration technique used often determines drug safety and efficacy (see pp. 113-114).
• Eyecup use is discouraged because of the risk of contamination.
• Observe expiration dates closely. Do not use outdated medication.
| Therapeutic Class | Cap and Label Color |
| Anti-infectives | Brown or tan |
| Beta-adrenergic blocking agents | Yellow, blue, or both |
| Miotics | Green |
| Mydriatics and cycloplegics | Red |
| Nonsteroidal anti-inflammatory agents | Gray |
Glaucoma
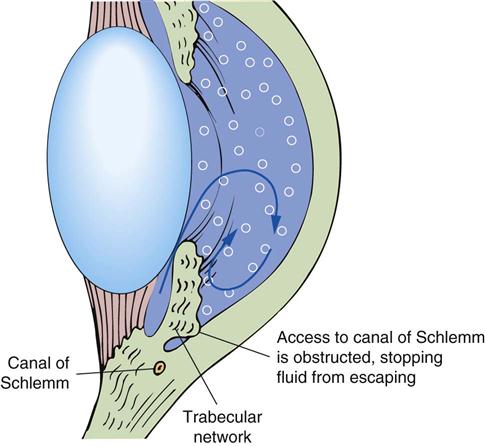
Glaucoma is an eye disease characterized by abnormally elevated intraocular pressure (IOP), which may result from excessive production of the aqueous humor or from diminished ocular fluid outflow. Increased pressure, if persistent and sufficiently elevated, may lead to permanent blindness. There are three major types of glaucoma, primary, secondary, and congenital. Primary includes closed-angle glaucoma and open-angle glaucoma. These are diagnosed by determination of the iridocorneal angle of the anterior chamber, where aqueous humor reabsorption takes place. Secondary glaucoma may result from previous eye disease or may occur after a cataract extraction and may require drug therapy for an indefinite period. Congenital glaucoma requires surgical treatment.
Open-angle glaucoma develops insidiously over the years as pathologic changes at the iridocorneal angle prevent the outflow of aqueous humor through the trabecular network to Schlemm’s canal and into the veins of the eye (Figure 43-3). In cases of open-angle glaucoma, there is reduced outflow of aqueous humor through the trabecular network and Schlemm’s canal because of resistance of the aqueous humor outflow; the iridocorneal angle is open (Figure 43-4).
Intraocular pressure builds up and, if not treated, will damage the optic disc. Initially, the patient has no symptoms, but over the years there is a gradual loss of peripheral vision. If untreated, total blindness may result.
Acute closed-angle glaucoma occurs when there is a sudden increase in IOP caused by a mechanical obstruction of the trabecular network in the iridocorneal angle (Figure 43-5). This occurs in patients who have narrow anterior chamber angles. Symptoms develop gradually and appear intermittently for short periods, especially when the pupil is dilated. (Dilation of the pupil pushes the iris against the trabecular meshwork, causing the obstruction.) Symptoms often reported are blurred vision, halos around white lights, frontal headache, and eye pain. Patients often associate the symptoms with stress or fatigue. An attack can also be precipitated by administration of a mydriatic agent, such as atropine or scopolamine, for eye examination.
Drug Therapy for Glaucoma
The treatment of open-angle glaucoma is maintenance of IOP at normal levels to prevent further blindness. Treatment options include surgery, laser surgery, and drug therapy. A beta-adrenergic blocking agent (e.g., timolol maleate) has become the initial drug of choice. Other agents that may also be used are prostaglandins (e.g., latanoprost, sympathomimetic agents (e.g., brimonidine), carbonic anhydrase inhibitors (e.g., acetazolamide), and cholinesterase inhibitors (e.g., echothiophate iodide). The selection of the drug is determined to a great extent by the requirements of the individual patient and response to therapy.
Acute angle-closure glaucoma requires immediate treatment to reduce IOP. Intravenous mannitol, an osmotic diuretic, may be administered to draw aqueous humor from the eye. Topical corticosteroids may be used to reduce ocular inflammation. Other medications used to reduce formation of aqueous humor include beta blockers, prostaglandins, a sympathomimetic agent, or a carbonic anhydrase inhibitor. After IOP has been reduced, pilocarpine may be used to induce miosis, relieving the pressure of the iris against the trabecular network and allowing drainage of the aqueous humor. Analgesics and antiemetics may be administered if pain and vomiting persist. Surgery is then required to correct the abnormality.
 Nursing Implications for Glaucoma and Other Eye Disorders
Nursing Implications for Glaucoma and Other Eye Disorders
The nurse has an important role in educating the public and promoting safety measures to protect the eye from potential sources of injury. Health professionals can participate in this role during their daily contacts with people in the community. The use of safety glasses in potentially hazardous situations, prevention of chemical burns from common household cleansing items or other agents at home or work, proper cleaning and wearing of contact lenses or glasses, and selection of safe toys and play activities for children are some areas about which the nurse can teach the public. These safety measures can significantly reduce the number of injuries that occur annually.
Nurses play an important role in detecting eye disorders and implementing treatment plans. An example of this is in patients with diabetes mellitus. Encourage annual, or more frequent, eye examinations to detect and prevent complications associated with the disease.
The primary delivery of eye care is through self-administration of drugs. One of the greatest challenges in the care of chronic eye disorders such as glaucoma is convincing the patient of the need for long-term treatment and adherence to the therapeutic regimen.
Assessment
Eye Examination
History of Symptoms
Psychological.
What type of response is the patient exhibiting to the disturbance in visual acuity? Is the patient withdrawing socially? Identify a support system available for at-home care and assistance. Plan a specific time to meet with the patient and significant others to discuss at-home care and community resources available if assistance is indicated.
Diagnostics.
Ask the patient to describe what eye diagnostic procedures have been completed before admission (e.g., visual acuity measurement, tonometry, slit-lamp examination, visual fields). Normal IOP using an applanation tonometer is 10 to 21 mm Hg.
Medications.
Ask for a list of all prescribed, over-the-counter medications and herbal products being taken. Ask for details on medications, dosage, schedule, and degree of compliance. List all ordered medications on the medication administration record (MAR). If beta blockers are being taken, list the pulse and blood pressure on the MAR as a preassessment to administration of the ophthalmic drops. Mark the Kardex or enter data into the computer with parameters relating to the prevention of injury, the activity and exercise level permitted, and diet orders.
Implementation
• Perform assessments every shift consistent with the patient’s status and diagnosis.
• Prepare the patient for eye examinations, diagnostics, or eye surgery.
• Assist with diagnostic procedures (e.g., visual fields, tonometry, visual acuity).
• Institute appropriate comfort measures.
• Ensure that an eye patch and shield are applied properly to protect the eye from further injury.
• Always speak before touching a person with impaired vision.
 Patient Teaching and Health Promotion
Patient Teaching and Health Promotion
After Eye Surgery
• Instruct the patient to instill the eye medications using aseptic techniques and to comply with prescribed eye medication routine to prevent infection (see Figures 8-6 and 8-7). In general, using more than one drop per dose of medication does not improve response but increases the frequency of adverse effects and the cost of therapy. Instruct the patient on how to block the nasolacrimal duct during instillation to minimize systemic effects.
Disease or Disorder
Visual Acuity
Medications
Fostering Health Maintenance
Written Record.
Enlist the patient’s aid in developing and maintaining a written record (see Patient Self-Assessment Form for Eye Medications on the![]() Evolve Web site at http://evolve.elsevier.com/Clayton) of monitoring parameters (e.g., blood pressure and pulse with adrenergic and beta-adrenergic blocking agents, degree of visual disturbance, progression of impairment) and response to prescribed therapies for discussion with the physician. Encourage the patient to take this record to all follow-up visits.
Evolve Web site at http://evolve.elsevier.com/Clayton) of monitoring parameters (e.g., blood pressure and pulse with adrenergic and beta-adrenergic blocking agents, degree of visual disturbance, progression of impairment) and response to prescribed therapies for discussion with the physician. Encourage the patient to take this record to all follow-up visits.
Drug Class: Osmotic Agents
Actions
Osmotic agents are administered intravenously, orally, or topically to reduce IOP. These agents elevate the osmotic pressure of the plasma, causing fluid from the extravascular spaces to be drawn into the blood. The effect on the eye is reduction of volume of intraocular fluid, which produces a decrease in IOP.
Uses
The osmotic agents are used to reduce IOP in patients with acute narrow-angle glaucoma; before iridectomy; preoperatively and postoperatively in conditions such as congenital glaucoma, retinal detachment, cataract extraction, and keratoplasty; and in some secondary glaucomas.
Therapeutic Outcome
The primary therapeutic outcome expected from osmotic agents is reduced IOP.
 Nursing Implications for Osmotic Agents
Nursing Implications for Osmotic Agents
Premedication Assessment
Availability
See Table 43-1.
![]() Table 43-1
Table 43-1
| GENERIC NAME | BRAND NAME | AVAILABILITY | DOSAGE | COMMENTS |
| mannitol | Osmitrol | 5%, 10%, 15%, 20%, 25% solutions for infusions | IV: 1.5-2 g/kg as a 20% solution over 30 min | Used intravenously when oral methods are unacceptable |
| When used preoperatively, administer 60-90 min before surgery | ||||
| Use an in-line filter because mannitol has a tendency to crystallize | ||||
| urea | Ureaphil | 40 g in 150 mL | IV: 1-5 g/kg | Administer as a 30% solution at an infusion rate not to exceed 4 mL/min |
| Used when mannitol and oral methods are not available | ||||
| Do not exceed 120 g daily | ||||
| Use extreme caution against extravasation, or tissue necrosis may result | ||||
| Do not infuse in veins of lower extremities because of the possibility of thrombus formation |
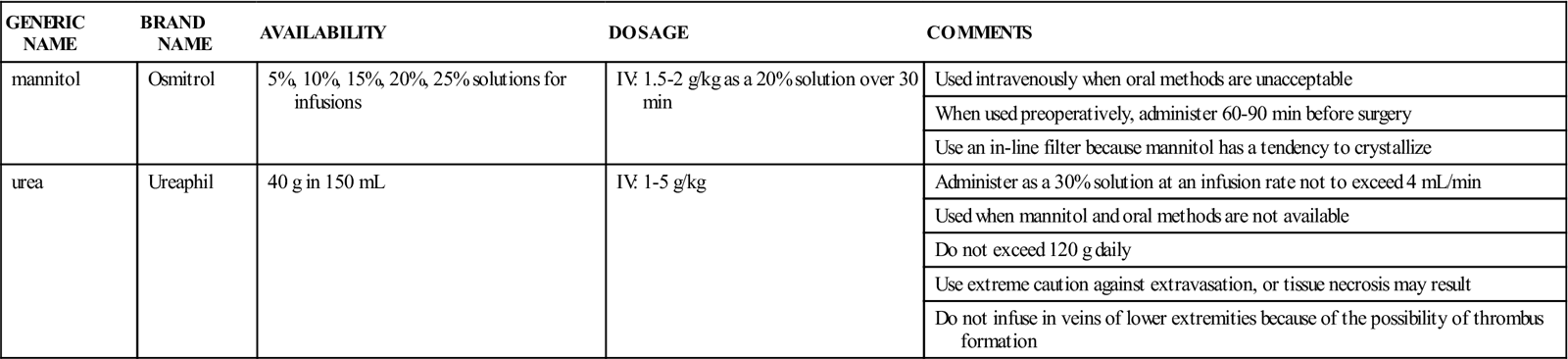
Dosage and Administration
See Table 43-1.
Monitoring
Serious Adverse Effects
Hematologic
Thirst, Nausea, Dehydration, Electrolyte Imbalance.
The electrolytes most commonly altered are potassium (K+), sodium (Na+), and chloride (Cl−). Many symptoms associated with altered fluid and electrolyte balance are subtle and resemble general symptoms of drug toxicity or the disease process itself. Gather data about changes in the patient’s mental status (alertness, orientation, and confusion), muscle strength, muscle cramps, tremors, nausea, and general appearance (drowsy, anxious, lethargic). Always check the electrolyte reports for early indicators of electrolyte imbalance. Keep accurate records of intake and output, daily weights, and vital signs.
Neurologic
Headache.
This is an indication of cerebral dehydration. Keeping the patient in a supine position can minimize it.
Vascular
Circulatory Overload.
These medications act on the blood volume by pulling fluid from the tissue spaces into the general circulation (blood). Assess the patient at regularly scheduled intervals for signs and symptoms of fluid overload, pulmonary edema, or heart failure. Perform lung assessments; report the development of crackles and increasing dyspnea, frothy sputum, or cough.
Drug Interactions
Lithium.
Mannitol increases the excretion of lithium. Patients being treated with lithium should be monitored for low lithium levels if treated with mannitol.
Drug Class: Carbonic Anhydrase Inhibitors
Actions
These agents are inhibitors of the enzyme carbonic anhydrase. Inhibition of this enzyme results in a decrease in the production of aqueous humor, thus lowering IOP.
Uses
These agents are used in conjunction with other treatments to control IOP in cases of intraocular hypertension and closed-angle and open-angle glaucoma. Dorzolamide has the advantage of intraocular administration, with less potential for systemic adverse effects.
Therapeutic Outcomes
The primary therapeutic outcome expected from carbonic anhydrase inhibitors is reduced IOP.
 Nursing Implications for Carbonic Anhydrase Inhibitors
Nursing Implications for Carbonic Anhydrase Inhibitors
Premedication Assessment
3 Ensure that contact lenses have been removed before the instillation of dorzolamide drops.
4 Ensure that baseline electrolyte laboratory studies have been drawn as ordered.
5 Assess and record baseline weight, hydration data, vital signs, and mental status.
6 Record premedication IOP readings and visual acuity data.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree