There are three parts to this section:
1. Principles of tracheostomy care
2. Removal of respiratory tract secretions via a tracheostomy tube
3. Changing a tracheostomy tube/tube management
Learning outcomes
By the end of this section, you will be able to:
▪ Understand the rationale for tracheostomy
▪ Identify the equipment used in this nursing practice
▪ Discuss the care of a patient with a tracheostomy in situ
▪ Identify the potential problems a patient with a tracheostomy may experience.
Background knowledge required
Revision of the anatomy and physiology of the upper respiratory tract, and theanatomy of the upper gastrointestinal tract
Revision of local policy or guidelines on the care of a patient with a tracheostomy
Revision of your knowledge in relation to wound care.
Indications and rationale for the creation of a tracheostomy
A tracheostomy is an artificial opening, which is surgically created by an incision made into the anterior wall of the trachea (Docherty & Bench 2002). The incision is usually made at a level between the 2nd and 4th cartilaginous rings of the trachea.
A tracheostomy can be temporary, e.g. left in situ for a number of days, weeks or months before removal, or permanent, i.e. for the remainder of the patient’s life. Most tracheostomies are temporary (Docherty & Bench 2002).
Temporary tracheostomy
This involves the opening of the surgical incision and the insertion of a tracheostomy tube. The tube is then held in place by tapes secured around the patient’s neck (Fig. 42.1).
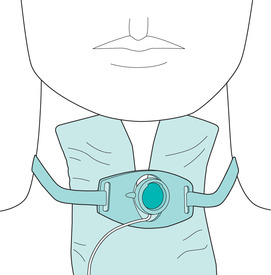 |
| FIGURE 42.1Tracheostomy dressing and securing device in situ |
Permanent tracheostomy (or tracheostoma)
This involves the incision of the circumference of the trachea so that it forms a permanent stoma or opening on the surface of the skin, i.e. the trachea is incised and sutured to the skin surface. In these cases a tracheostomy tube may remain in situ until the stoma has healed or if there are any complications with healing or stoma formation.
Tracheostomy is becoming more common in both acute and community settings (Serra 2000). As a nurse, you therefore need to understand the rationale for this surgical procedure and utilise evidence-based knowledge in caring for your patient who has a tracheostomy in place. In doing this you will promote clinical effectiveness and prevent potential complications, as well as reassure your patient and their family.
Indications for tracheostomy
These can be listed (Serra 2000) as:
▪ the need to bypass potential or actual airway obstructions, e.g. tumour, inflammation, trauma, foreign body
▪ to support prolonged and assisted ventilation in certain neuromuscular disorders, e.g. motorneurone disease, certain chronic respiratory disorders, e.g. chronic obstructive pulmonary disease, and in patients who are sedated or comatose
▪ to aid in the expectoration and/or removal of bronchial secretions, thus reducing the risk of respiratory infection or to prevent other respiratory complications such as atelectasis
▪ in laryngectomy, where a permanent tracheostoma is formed.
 Equipment
Equipment1. Plastic disposable or single-patient tracheostomy tubes are usually used in the management of both temporary and long-term tracheostomies. Tubes can either have a single cannula or consist of two parts – an outer and inner cannula. Each healthcare provider will have guidelines on the type of tube they prefer to use. A tube without an inner cannula can be left in situ for a few days or removed and replaced as and when necessary. A two-part tube can be left for a longer period. In both cases the manufacturer’s instructions should be read carefully as this will give guidance as to the length of time the tube can remain in situ – this refers to the licensed use of the product.
2. Most of your patients will have a tracheostomy tube that incorporates an inner cannula that can be changed and cleaned regularly, reducing the need to perform a complete change of the outer tracheostomy tube. The inner cannula also provides essential protection against potentially life-threatening problems, such as tube obstruction, as it can be removed quickly and safely thus providing prompt relief to your patient (Oxford Radcliffe NHS Hospital Trust 2005). A patient may occasionally have a silver tube in situ that also incorporates an inner cannula, although this is now rare due to the extensive range of plastic tubes available.
3. A cuffed tube (Fig. 42.2) may be used in your patient’s immediate postoperative phase of care as they assist in airway maintenance and prevent the potential aspiration of secretions from the recently formed wound around the tube. Your patient may feel the cuff pressing against their throat so you should provide meaningful explanation at this point. Once any secretions from the wound have ceased an uncuffed tube may be considered. Finally, tubes can either be fenestrated or unfenestrated. Fenestrated tubes are used when weaning off the tube or to enable phonation. Therefore tubes can be (Fig. 42.3):
— single/double cannula
— cuffed/uncuffed
— fenestrated/unfenestrated.
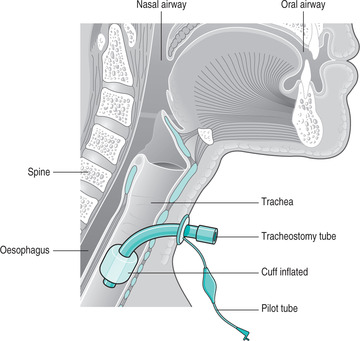 |
| FIGURE 42.2Anatomy of the trachea with a tracheostomy tube in placeFrom Woodrow 2002. Copyright RCN Publishing Company 2002. Reproduced by permission of Nursing StandardRCN Publishing Company |
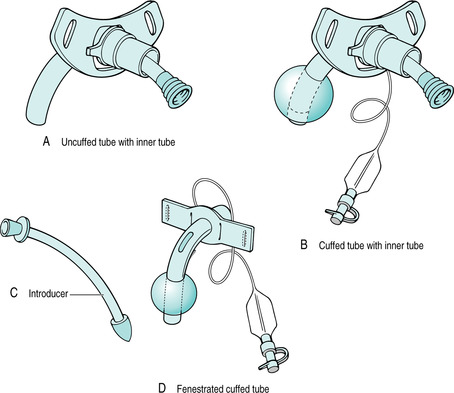 |
| FIGURE 42.3Tracheostomy tubes in common use A Uncuffed tube with inner tube B Cuffed tube with inner tube C Introducer D Fenestrated cuffed tube |
4. Tracheostomy tubes come in a variety of sizes for adult use: 7.0 mm, 7.5 mm, 8.0 mm, 8.5 mm and 9 mm. The diameter and length of the tube selected will be dependent upon your patient’s needs and will always be slightly smaller than the diameter of the trachea (Dickson & Martindale 2002).
Essential equipment
The essential equipment to be at the bedside of all patients with a tracheostomy should include the following (Serra 2000; Oxford Radcliffe NHS Hospital Trust 2005):
1. Spare tracheostomy tubes – same size and type as well as a tube the next size down
2. Tracheal dilators
3. Stitch cutter (if the tracheostomy tube is stitched to the skin)
4. Suction equipment: suction catheters (no larger in diameter than half the diameter of the tracheostomy tube), connection tubing, suction container, gloves, aprons
5. Sterile water and normal saline
6. Humidification equipment and tracheal masks
7. Tracheostomy dressings
8. Scissors
9. Cuff manometer if cuffed tube in situ
10. Tracheostomy tapes
12. Cuffed tube (if your patient has an uncuffed tube in situ)
13. Equipment for oral hygiene.
The Code of Professional Conduct (Nursing and Midwifery Council 2004) states that all nurses are individually accountable for their own actions. It is therefore imperative that you ensure that you are familiar not only with your local policies regarding tracheostomy care but are able to identify and use safely, all equipment related to this practice.
 Guidelines and rationale
Guidelines and rationaleSuccessful tracheostomy care is dependent upon a multi-disciplinary approach to care as well as collaborative care involving healthcare professionals, patients and their families. Where possible, patients should be educated regarding their treatment and care in the preoperative phase and introduced to all members of the multi-disciplinary team who will include:
▪ nurses
▪ consultant surgeon and medical team
▪ specialist nurse
▪ speech and language therapist
▪ physiotherapist
▪ dietician
Get Clinical Tree app for offline access



