CHAPTER 40. Environmental Emergencies
Kathleen Flarity
HEAT-RELATED EMERGENCIES
Many cases of heat illness are reported annually in the United States. Only head injury, spinal cord injury, and heart failure are responsible for more deaths in athletes than heat illness. 23 Regardless of physical condition, anyone can suffer ill effects from heat stress if the exposure is intense or prolonged. The effects of environmental heat stress can be mild or severe, depending on the degree of heat and length of exposure. Emergencies related to heat stress range in severity from heat edema, heat cramps, and heat exhaustion to potentially life-threatening heat stroke.
Heat Edema
Heat edema occurs in nonacclimated individuals during prolonged periods of standing or sitting. Characteristic swelling of feet and ankles resolves in a few days. Treatment includes rest, elevation of the legs, and support hose. Heat edema is self-limiting and generally does not require further treatment.
Heat Cramps
Heat cramps are severe cramps (brief and intermittent) of specific muscles, usually in the shoulders, thighs, and abdominal wall. Associated symptoms include weakness, nausea, tachycardia, pallor, profuse diaphoresis, and cool moist skin. The person’s core temperature may be normal or slightly elevated. Heat cramps usually develop suddenly when the victim is resting after exertion in a hot environment or one with high humidity. Salt depletion secondary to excessive perspiration in combination with excessive water consumption leads to muscle cramping. Increased water intake does not replace sodium losses caused by perspiration. Instead, water dilutes serum sodium, causing hyponatremia, the key factor in the development of heat cramps. 1
Treatment includes removal of the person from the heat source, rest, and electrolyte replacement with oral or parenteral fluids. Discharge instructions should stress the importance of drinking commercially prepared electrolyte supplements (e.g., Gatorade, Powerade, All Sport) when working outdoors or participating in strenuous recreational activities during hot weather. Strenuous activity should be avoided for at least 12 hours after discharge. 1. and 22.
Heat Exhaustion
Heat exhaustion is a clinical syndrome caused by prolonged heat exposure, usually over hours or days. Excessive perspiration and inadequate fluid and electrolyte replacement lead to fluid loss, electrolyte depletion, and dehydration. Heat exhaustion occurs most often in individuals working in hot environments. Older adults and the very young are at greatest risk because they cannot or do not increase fluid intake sufficiently to compensate for increased fluid losses from sweating. 1.12. and 23.
Heat exhaustion is characterized by rapid onset (within minutes) of extreme thirst, general malaise, muscle cramping, headache, nausea, vomiting, anxiety, and tachycardia—ultimately leading to syncope and collapse. Associated dehydration may cause orthostatic hypotension and mild to severe temperature elevation (98.6° F to 105° F [37° C to 40.5° C]). Diaphoresis may or may not be present. Untreated, heat exhaustion can progress to heat stroke.
Initial treatment begins with moving the patient to a cool, quiet environment and removing constricting clothing. When significant hyperthermia is present, moist cloths placed on the patient reduce temperature by evaporation. Fluid and electrolyte replacement should be initiated. Oral replacement with a balanced commercial salt preparation can be used if the patient is not nauseated. Intravenous 0.9% saline solution should be used if the patient is nauseated or vomiting. Salt tablets are not recommended because of potential gastric irritation and hypernatremia. Monitor the patient’s temperature during treatment. Hypotension may be corrected initially with a 300- to 500-mL bolus of 0.9% saline, with subsequent infusions correlated to clinical and laboratory findings. Patients with hypotension or a history of cardiac disease should be placed on a cardiac monitor because heat exhaustion can rapidly evolve into heat stroke. Admission should be considered for any patient who does not improve significantly after 3 to 4 hours of emergency treatment. 1.12. and 23.
Heat Stroke
Heat stroke is the least common but most emergent and life-threatening form of heat illness. Mortality as high as 70%1 is directly related to the speed and effectiveness of diagnosis and treatment. Heat stroke is defined as an abnormal form of hyperthermia resulting from a failure of the body’s physiologic systems to dissipate heat and cool down. Heat stroke is characterized by an elevated core temperature of 104°F (40° C) or greater. Environmental factors and the patient’s ability to dissipate heat also affect the outcome of heat stroke.
Heat stroke occurs in one of two forms: classic heat stroke and exertional heat stroke. Classic heat stroke occurs during prolonged exposure to sustained high ambient temperatures and humidity. It commonly affects older adults, the chronically ill, and those who live in poorly ventilated homes without air conditioning. Children locked in cars on hot days are at great risk for developing heat stroke. Poor dissipation of environmental heat is the underlying cause of classic heat stroke. In contrast, those patients with exertional heat stroke are usually young and healthy, often athletes and military recruits. In these individuals heat production overcomes the internal heat dissipation mechanisms. Onset of heat stroke is usually sudden; however, older adults and patients in predisposing environments can develop heat exhaustion several hours before heat stroke develops (Box 40-1). Heat stroke may present with changes in neurologic function such as anxiety, confusion, hallucinations, loss of muscle coordination, combativeness, and coma. Direct thermal damage to the brain combined with decreased cerebral blood flow can lead to cerebral edema and hemorrhage. The brain, particularly the cerebellum, is extremely sensitive to thermal injury; therefore the range of neurologic symptoms is broad. 1.12. and 23.
Box 40-1
Get Clinical Tree app for offline access

R isk F actors A ssociated W ith H eat S troke
AGE
Older adults
Infants
ENVIRONMENTAL CONDITIONS
High environmental temperatures
High relative humidity
Low wind
PREEXISTING ILLNESS
Cardiovascular disease
Dehydration
Autonomic neuropathies
Previous stroke/central nervous system lesions
Obesity
Diabetes
Cystic fibrosis
Low fitness
Skin disorders (e.g., large burn scars)
PRESCRIPTION DRUGS
Anticholinergics
Phenothiazines
Butyrophenones
Tricyclic antidepressants
Antihistamines
Antispasmodics
Diuretics
Antiparkinsonian drugs
β-Blockers
STREET DRUGS
Lysergic acid diethylamide (LSD)
Jimson weed
Amphetamines
Phencyclidine (PCP)
Alcohol
Management of heat stroke is directed at reducing core temperature as rapidly as possible and treating subsequent complications. Heat stroke is often fatal despite rapid treatment. Maintenance of airway, breathing, and circulation (ABCs) is crucial for patient recovery. Establish an airway, and administer supplemental oxygen by the method most appropriate for the patient’s level of consciousness. Fluid volume is not depleted in most victims of hyperthermia; therefore 1 to 2 L of 0.9% saline solution during the first 4 hours is usually adequate. Lactated Ringer’s solution is not recommended because the liver may not be able to metabolize lactate. Hemodynamic monitoring is indicated until normal vital signs are restored. After the ABCs are secured, rapid, aggressive cooling becomes the next intervention.
Prehospital treatment starts with removing the patient from the external source of heat and removing all clothing. Aggressive ice- or cold-water cooling should be avoided in the field to prevent shivering and seizure activity, which will only increase the core body temperature. Spray the patient with tepid water while fanning the entire body to promote cooling by evaporation. Well-padded ice packs in vascular areas such as the groin, axilla, and neck are also useful. Ice water or cold water immersion is an effective method of rapidly lowering core body temperature; however, its use is one the of the more hotly debated topics in the heatstroke literature. In addition to being unpleasant for the patient and caregiver, access to the patient is limited. Ice water immersion can also cause shivering, which dramatically increases oxygen consumption and can increase body temperature. Intravenous chlorpromazine (Thorazine), 10 to 25 mg, may be used to prevent shivering during the cooling process. Massive peripheral vasoconstriction from ice water immersion can act as an insulator and prevent adequate cooling. After the patient is in the emergency department (ED), aggressive cooling measures such as ice water gastric and peritoneal lavage can also be used. Cooling blankets may be used; however, cooling from wet skin is 25 times more effective than cooling from dry skin
Cooling should be continued until the rectal temperature is 102° F (38.8° C) or less. Core temperature should be monitored frequently during the cooling phase to prevent inadvertent hypothermia. Aspirin and acetaminophen have not proved effective in reducing hyperthermia secondary to heat stroke. Corticosteroid therapy, usually with methylprednisolone, may be used to treat cerebral edema. Intracranial pressure monitoring may be helpful for some patients. To increase renal blood flow, intravenous mannitol, 0.2 g/kg over 3 to 5 minutes, is recommended in patients over 12 years of age whose urinary output is less than 50 mL/hr.
High-output cardiac failure may develop with heat stroke; therefore patients should be placed on a cardiac monitor. Central venous pressure and pulmonary capillary wedge pressure monitoring may be considered in the critical phase to evaluate fluid status. Protecting the kidneys and liver from thermal and low-flow damage is critical. Myoglobinuria and poor renal perfusion put the kidneys at risk for renal failure; therefore urine should be carefully monitored for color, amount, pH, and myoglobin. 1.12. and 23.
COLD-RELATED EMERGENCIES
Approximately 700 fatalities occur annually in the United States from cold exposure. 6 In 2003 the majority of reported deaths from exposure to cold were male (67%), and 51% were older than 65 years of age. 6 Most deaths do not occur in the extreme northern areas but are reported in temperate regions, urban areas in poorly heated apartments, and among the homeless. Nicotine, alcohol intoxication, and major psychiatric disorders are also predisposing factors. 4
Injuries related to cold exposure are localized or generalized. Localized cold emergencies include chilblains, immersion foot, and frostbite, whereas hypothermia is a generalized cold emergency. Cold-related emergencies occur with prolonged exposure to cold ambient temperatures, immersion in cold water, or as a result of factors such as alcohol. Ambient temperature is a product of air temperature and wind speed: the greater the wind speed, the lower the ambient temperature. Heat loss occurs 24 times more quickly with immersion in cold water. 12. and 19.
Chilblains
Chilblains are localized areas of itching and redness accompanied by recurrent edema to exposed or poorly insulated body parts such as the ears, fingers, and toes. Chilblains are usually seen in cool, damp climates with temperatures above freezing. Chilblains are probably a mild form of frostbite with gradual onset of symptoms. There is generally no pain; however, the patient may experience transient numbness and tingling. Initial pallor or redness of the nose, digits, or ears may evolve into plaques and small, superficial ulcerations over chronically exposed areas.
Prehospital treatment begins with removal to a warm area in conjunction with covering the affected area with a warm hand or placing fingers under the axilla. 19 Elevation of the affected area decreases edema, which increases circulation and allows gradual warming at room temperature. Never rub or massage injured tissue. Avoid direct heat application. Tissue damage is rarely seen with chilblains; however, the patient should be instructed to protect the area from injury and further environmental exposure and to watch for signs of secondary infection. 11. and 18.
Nonfreezing Cold Injury (Immersion Foot)
Nonfreezing cold injury, a syndrome also known as immersion foot or trench foot, results from damage to peripheral tissues from prolonged (hours to days) contact between a wet foot and cold temperature. This usually occurs when the patient is wearing a watertight boot that does not allow normal evaporative “breathing.” This condition is commonly seen in hunters and soldiers on outdoor maneuvers. Feet initially are cold, damp, numb, and edematous but within 24 to 48 hours will appear warm. Vasodilation and hyperemia, which result from warming, cause intense burning and tingling. Prolonged and repeated exposure can lead to lymphangitis, cellulitis, thrombophlebitis, and liquefaction gangrene.
Therapeutic interventions include drying the feet and changing frequently into dry socks. After the patient is in a controlled environment, rewarm injured areas gradually by exposing them to air or soaking them in warm water (100° F to 105° F [37.7° C to 40.5° C]) before drying. Some clinicians recommend daily air-drying of the feet for 8 hours. 3 Immersion foot is reversible with timely treatment. Patients are usually hospitalized for observation and prevention of complications.
Frostbite
Frostbite, the most prevalent injury caused by extreme cold, occurs when ice crystals form in intracellular spaces as tissue freezes. These crystals enlarge and compress cells, causing membrane rupture, interruption of enzymatic activity, and altered metabolic processes. Histamine release increases capillary permeability, red cell aggregation, and microvascular occlusion. 1 Once frostbite occurs, damage is irreversible. Further exposure to extreme cold or trauma increases tissue damage and worsens the injury. The patient with frostbite may also have hypothermia. Treatment of hypothermia takes priority over management of frostbite. Frostbite can be superficial or deep, depending on the degree of the cold and the length of exposure. Estimation of the extent of injury may not be possible until several days after exposure. 6. and 12.
Superficial Frostbite
Superficial frostbite involves skin and subcutaneous tissue and is similar to a superficial burn. Fingertips, ears, nose, toes, and cheeks are the areas most commonly affected. Symptoms include tingling, numbness, burning sensation, and white, waxy color. Frozen skin feels cold and stiff. After the tissue thaws, the patient may feel a hot, stinging sensation. Affected areas become mottled and blisters develop within a few hours. Frostbite tissue is extremely sensitive to subsequent cold and heat exposure and therefore is susceptible to repeat frostbite or burn injury.
Injured tissue is friable, so recovery depends on very gentle handling. Do not rewarm if there is a chance of refreezing. Do not rub the affected area. Apply warm soaks (104° F to 110° F [40° C to 43.3° C]), and elevate the extremity. Place the patient on bed rest for several days until the full extent of the injury has been evaluated and normal circulation has returned. The patient’s room should be warm; however, heavy blankets should be avoided because friction and weight on the affected area can lead to sloughing. 6. and 12.
Deep Frostbite
Deep frostbite occurs when the temperature of a limb is lowered. Deep frostbite usually involves muscles, bones, and tendons. The degree of frostbite depends on ambient temperature, wind chill factor, duration of exposure, whether the patient was wet while exposed or in direct contact with metal objects, and the type of clothing worn. Deep frostbite appears white or yellow-white and is hard, cool, and insensitive to touch. 1 The patient has a burning sensation followed by a feeling of warmth, then numbness. Blisters appear 1 to 7 days after injury. Edema of the entire extremity occurs and may persist for months (Figure 40-1). A gray-black mottling eventually progresses to gangrene (Figure 40-2).
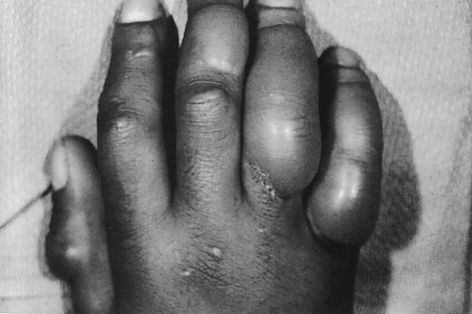 |
| FIGURE 40-1 Large, clear frostbite blisters on the right hand. (From Rosen P, Barkin RM, Hockberger RS et al, editors: Emergency medicine: concepts and clinical practice, ed 4, St. Louis, 1998, Mosby.) |
 |
| FIGURE 40-2 Gangrenous necrosis resulting from frostbite injury. (From Auerbach P, editor: Wilderness medicine, ed 5, St. Louis, 2007, Mosby.) |
Prehospital treatment includes transport with gentle handling and moderate elevation of the affected part. 3 Rewarming of the affected area is deferred until the patient reaches the ED. Do not rub the affected part with snow or ice. If the extremity has thawed, keep it immobile. Prevent heat loss by removing wet clothing, covering the patient with dry blankets, and removing the patient from the cold environment. If the patient is transported in a ground or air ambulance, warmed oxygen is recommended. Mylar or wool head coverings help prevent further heat loss.
Rapid rewarming under controlled conditions is the ideal treatment for maintaining tissue viability. Rewarming the patient with hypothermia and severe frostbite should occur with strict medical control. After the patient reaches the ED, obtain a baseline core temperature (rectal or esophageal), then immerse the affected area in warm (104° F to 110° F [40° C to 43.3° C]) water. Thawing frozen tissue is extremely painful, so liberal administration of parenteral narcotics is needed in severe cases. Warm all intravenous fluids before infusing them. Assess tetanus immunization status, and consider antibiotic therapy for deep infections. If hypothermia is not present, administer warm oral liquids. Cover the patient with warm blankets, but avoid friction and pressure on the affected area. Protect the thawed part with a large, soft, bulky dressing. Elevate the affected area to minimize edema. If severe vasoconstriction is present, escharotomy may be required. Final determination of the depth of injury may not be possible for several weeks; therefore amputation is not considered in the ED.
Hypothermia
Hypothermia can occur in many different situations, including cold ambient air, cold water immersion, or cold water submersion. Hypothermia can also occur as the result of a disease process (e.g., hypoglycemia), infusion of room temperature fluids, alcohol consumption, and ingestion of some medications. Hypothermia is defined as a core temperature below 95° F (35° C). Severe hypothermia is a core temperature less than 90° F (32.2° C). The American Heart Association has established 86° F (30° C) as the temperature for initiation of aggressive internal rewarming procedures. 17 The body’s metabolic responses depend on a normal core temperature. As the core temperature drops, there is a progressive decrease in cellular activity and organ function. When the temperature drops by 18° F (10° C), the basal metabolic rate drops by two to three times the normal rate. The most obvious response is seen in the central nervous system (CNS). The patient becomes apathetic, weak, and easily fatigued, with impaired reasoning, coordination, and gait. The patient’s speech is slow or slurred. Renal blood flow decreases, causing a decline in the glomerular filtration rate. Impaired water reabsorption leads to dehydration. Decreased respiratory rate and effort lead to carbon dioxide retention, hypoxia, and acidosis. Shivering consumes glucose stores, so the patient becomes hypoglycemic. Insulin levels fall, so available glucose decreases, forcing the body to metabolize fat for energy. Drug metabolism in the liver is sluggish, so medication effects may last longer. 8. and 17.
The cardiovascular system is also dramatically affected. Cold heart muscle is irritable and prone to dysrhythmias. The Osborne or J wave is a striking feature seen on electrocardiogram in approximately one third of hypothermic patients32 (Figure 40-3). The J wave is described as a “humplike” deflection between the QRS complex and the early part of the ST segment. The most common dysrhythmias are atrial and ventricular fibrillation. The cold patient is in great danger of ventricular fibrillation when core temperature falls below 82° F (27.8° C). Ventricular fibrillation at these extremely cold temperatures does not respond to conventional treatment without prior rewarming. Defibrillation is limited to three shocks until core temperature is greater than 86° F (30° C). 10 Intravenous medications are also limited until the core temperature is greater than 86° F (30° C). Careful handling of hypothermic patients, especially when their temperatures reach the vulnerable mid-80s range, is imperative because even turning may cause ventricular fibrillation. Rewarming procedures are active or passive, based on external warming or internal warming. 17Table 40-1 lists various procedures by category.
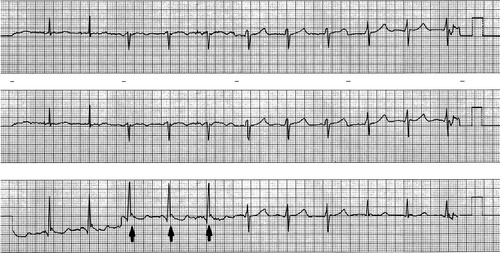 |
| FIGURE 40-3 Hypothermic J waves with QT prolongation. (From Rosen P, Barkin RM, Hockberger RS et al: Emergency medicine: concepts and clinical practice, ed 3, vol 1, St. Louis, 1992, Mosby.) |
| KCL, Potassium chloride. | |
| External Rewarming Procedures | Internal Rewarming Procedures |
|---|---|
| PASSIVE | PASSIVE |
| Move the patient to a warm area | Warmed humidified oxygen |
| Remove patient’s wet clothing | Warmed intravenous fluids |
| Cover the patient with blankets | |
| ACTIVE | ACTIVE |
Radiant heat lamps Heating blankets Bair Hugger warming blanket Hot water bottles Heating pads | Peritoneal lavage with KCL-free fluid Gastrointestinal irrigation Extracorporeal rewarming Cardiopulmonary bypass Hemodialysis Esophageal rewarming tubes Continuous arteriovenous rewarming (CAVR) |
The goal in mild hypothermia (93.2° F to 96.8° F [34° C to 36° C]), in which the patient is still shivering, alert, and oriented, is to prevent further heat loss and rewarm the patient as rapidly as possible. 8.16. and 17. Passive external rewarming techniques such as moving the patient to a warm environment, replacing wet clothing with dry material, and wrapping with warm blankets may be effective. However, many patients require internal rewarming using warmed humidified oxygen. Giving the patient warmed, oral fluids that contain glucose or other sugars provides more heat through calories. Passive rewarming raises the temperature 1° F to 4° F (0.5° C to 2.0° C) per hour. Gradual rewarming minimizes the risk for active rewarming shock.
In moderate hypothermia (86° F to 93.2° F [30° C to 34° C]), rewarm truncal areas at 1° F (0.5° C) per hour using heating blankets such as Bair Hugger Therapy, radiant heating lamps, and hot water bottles. Monitor closely for marked vasodilatation and subsequent hypotension. American Heart Association guidelines recommend active internal rewarming when core temperature is less than 86° F (30° C) (see Table 40-1). Warmed humidified oxygen via endotracheal tube (108° F to 111° F [42.2° C to 43.8° C]), mechanically warmed intravenous fluid, peritoneal lavage, esophageal rewarming tubes, gastrointestinal irrigation, bladder irrigation, extracorporeal rewarming cardiopulmonary bypass, and hemodialysis may all be used.
In severe hypothermia (lower than 78.8° F [26° C]), active internal (core) rewarming in conjunction with active external rewarming procedures is essential to prevent rewarming shock. Rewarming shock can occur after rewarming is initiated. Cold peripheral blood returns to the central circulation, causing a continual drop in core temperature. Circulation of cold blood through the heart also increases ventricular irritability and leads to fibrillation. Rewarming may also cause peripheral vasodilatation, which can precipitate hypotension and cardiovascular collapse.
The continuous arteriovenous rewarming (CAVR) method, developed at the University of Washington, employs a modified bypass technique for rapid blood rewarming using a Level One fluid warmer normally used for trauma resuscitation. The treatment is preferred for patients with profound hypothermia. A spontaneous pulse is necessary because the patient’s intrinsic blood pressure drives flow through the countercurrent module. (In true cardiothoracic bypass, an external pump is built into the machine.) The catheters are placed into a femoral artery and venous cordis, the blood is warmed as it flows through the countercurrent module. The CAVR method has rewarmed profoundly hypothermic patients five times more rapidly (39 minus versus 199 minutes) than standard methods and was demonstrated to decrease mortality rate. 13
Successful rewarming depends on the patient’s age, general condition before the hypothermic event, length of the patient’s exposure, and careful handling by the ED team. To prevent hyperthermia secondary to aggressive rewarming, discontinue active rewarming when core temperature reaches 89.6° F to 93.2° F (32° C to 34° C).
SUBMERSION INCIDENTS
Each year in the United States more than 4,000 people die of drowning, with an additional 50,000 surviving submersion events annually. 7 The age distribution of victims is bimodal. One peak is for children less than 4 years of age (40% of all drowning victims); the other peak is for 15- to 25-year-olds. 31 Nearly 80% of teenagers who drown or suffer submersion injuries are male. Toddlers and young children are at risk because of their naturally inquisitive nature and inadequate supervision. Teenage boys are at risk because of risk-taking behavior during water-related activities, with alcohol as a contributing factor in more than 60% of teenage drownings. 7. and 20.
Submersion injury or near-drowning occurs when a patient initially survives suffocation while submerged in a liquid medium (Box 40-2). Drowning refers to death within 24 hours after a submersion event. Submersion can be intentional or unintentional. An estimated 59% of drownings in children younger than 1 year occur in bathtubs, and 56% are a result of child abuse. Because submersion victims rarely aspirate more than 3 to 4 mL/kg as a result of reflex laryngospasm, differentiating between saltwater and freshwater submersion is clinically insignificant.
Box 40-2




N ear-D rowning S urvival
FACTORS THAT INCREASE SURVIVAL
Immediate, quality cardiopulmonary resuscitation
Colder water (<70° F [21.1° C])
Cleaner water
Shorter immersion time
Less struggle
No associated injuries
FACTORS THAT HAVE NO EFFECT ON SURVIVAL
Sex
Race
Swimming ability
Eating a meal before the event
Type of water (saltwater or freshwater)
Use of abdominal thrusts (Heimlich maneuver) during resuscitation attempts
Concurrent illnesses (i.e., cardiac or pulmonary disease)
Hypoxemia, laryngospasm, and fluid aspiration cause airway inflammation, obstruction, and collapse of the small airways. Pulmonary capillaries become leaky, resulting in pulmonary edema and acute respiratory distress syndrome (ARDS). Surfactant washout and inactivation contribute to the development of atelectasis and intrapulmonary shunting. Severity of neurologic outcome depends on the duration of submersion, temperature of the water, and the time elapsed before effective basic life support (BLS). Submersion greater than 5 minutes is generally associated with severe neurologic damage.
Complications associated with near-drowning are the direct result of the hypoxic event. Primary complications are pulmonary, cerebral, and cardiovascular, including pulmonary edema, pneumonitis, ARDS, anoxic encephalopathy, and cardiopulmonary arrest. Later complications include cerebral edema, disseminated intravascular coagulation (DIC), acute tubular necrosis, and renal failure. The most important part of treatment for a near-drowning victim is immediate resuscitation in the prehospital phase. If a submersion victim has appropriate airway and ventilation management, anoxic brain injury may be avoided. 7.11.16.26. and 27.
Secondary drowning can occur up to 72 hours after the initial insult; therefore every near-drowning victim should be taken to the hospital for observation, regardless of how he or she appears immediately after the event. Inflammatory reactions in the lung injure the alveolar-capillary membrane and alter surfactant function. Approximately 10% to 15% of deaths associated with drowning are due to secondary drowning. Near-drowning victims should be observed for at least 24 hours. 7.11. and 16.
Immersion in cold water can cause sudden death from cardiac dysrhythmias rather than drowning. Immersion syndrome occurs when cold water stimulates the vagus nerve, causing bradycardia or cardiac arrest. Many victims of cold water immersion have a good chance of survival without neurologic sequelae when resuscitation is initiated early.
Presenting symptoms with near-drowning vary with length of submersion, water temperature, quality of water, associated injuries, onset of BLS, and the patient’s resuscitative response. Occasionally, near-drowning victims may be asymptomatic; however, most present with mild dyspnea, a deathlike appearance with blue or gray coloring, apnea or tachypnea, hypotension, heart rate as slow as 4 to 5 beats/min or pulselessness, cold skin, dilated pupils known as fish eyes, hypothermia, and vomiting. 33
Field resuscitation of the near-drowning victim is crucial for survival. Performing immediate BLS procedures on the victim after removal from the water has been cited as a significant factor in survival, regardless of advanced life support availability. Initial resuscitation focuses on correcting hypoxia, associated acidosis, and hypotension as soon as possible. Box 40-3 highlights essential prehospital resuscitation. Establish a patent airway while initiating cervical spine protection (there is a high incidence of cervical spine injury in drowning victims). Additional interventions include applying a nonrebreather oxygen mask to patients with spontaneous respirations, initiating bag-mask ventilation or endotracheal intubation if indicated, ventilating with 100% oxygen to correct hypoxia and acidosis, and obtaining intravenous access.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
