Care of Men with Reproductive Disorders
Objectives
1. Understand the effects of aging on the male reproductive system.
2. Summarize the medical and nursing management of erectile dysfunction.
3. Describe factors involved in fertility, infertility, and contraception in the male patient.
4. Discuss the most common diagnostic tests and examinations of the male reproductive system.
5. Describe the assessment of the male reproductive system.
6. Outline the pathophysiology and manifestations of common disorders of the male reproductive tract.
7. Evaluate the plan of care for a patient with a disorder of the male reproductive tract.
8. Identify the psychological and emotional impact of disorders of the male reproductive tract.
9. Understand the role of drug therapy in disorders of the male reproductive tract.
10. Compare and contrast four types of surgical treatments for benign prostatic hyperplasia (BPH).
11. Diagram the preoperative and postoperative nursing care of a patient with BPH.
12. Discuss inflammations of the male reproductive system and their treatments.
13. Illustrate the patient teaching involved for early detection of testicular and prostate tumors.
14. Describe the nursing care of a patient with prostate cancer.
1. Teach a patient about the procedure for a prostate biopsy.
2. Outline a nursing care plan for a patient with prostate cancer.
3. Devise a teaching plan for testicular examination for young adult men.
4. Prepare materials describing treatment to a patient experiencing erectile dysfunction.
Key Terms
androgens (ĂN-drō-jĕnz, p. 919)
azotemia (ă-zō-TĒ-mē-ă, p. 927)
cremasteric reflex (p. 926)
ejaculation (ē-jăk-ū-LĀ-shŭn, p. 919)
erectile dysfunction (ED) (p. 923)
erection (ĕ-RĔK-shŭn, p. 919)
gonads (GŌ-năds, p. 918)
gynecomastia (jīn-ĕ-kō-MĂS-tĭ-ă, p. 928)
impotence (ĬM-pō-tĕnz, p. 923)
infertility (ĭn-fĕr-TĬL-ĭ-tē, p. 924)
libido (lĭ-BĒ-dō, p. 920)
orchiectomy (ŏr-kē-ĔK-tō-mē, p. 933)
premature ejaculation (p. 924)
priapism (PRĪ-ă-pĭz-ĕm, p. 924)
PSA velocity (p. 934)
prostate-specific antigen (PSA) (prŏs-tāt, p. 922)
retrograde ejaculation (p. 924)
rugae (RŪ-jē, p. 919)
semen (SĒ-mĕn, p. 919)
spermatogenesis (p. 919)
tamponade (tăm-pŏn-ĀD, p. 929)
urodynamics (ū-rō-dī-NĂM-ĭks, p. 927)
vasectomy (vă-SĔK-tō-mē, p. 920)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Many diseases and disorders, and many medications, can affect the male reproductive system. The urinary system and reproductive system are so closely linked in the male that a disorder in one system often affects the other. Assessment of the reproductive system is an essential part of any comprehensive health history. The nurse needs to be comfortable with his or her own sexuality and knowledgeable about the male reproductive system to be helpful to the patient.
Overview of Anatomy and Physiology of the Male Reproductive System
What are the structures of the male reproductive system?
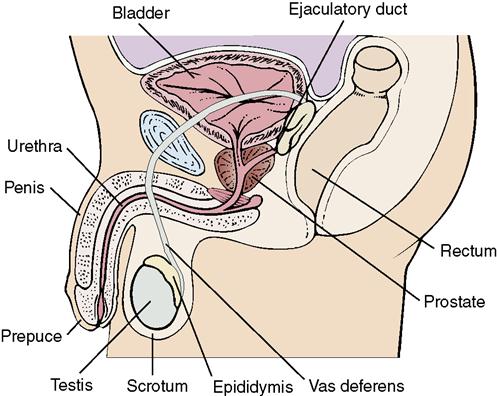
• The male gonads (sex glands) are the testes; they are oval shaped and are encased in the scrotum along with the epididymis, seminal vesicles, and vas deferens (Figure 40-1).
What are the functions of the organs of the male reproductive system?
How is sperm production controlled?
What changes occur with aging?
• The scrotum becomes more pendulous and there are fewer rugae.
• Prostate enlargement may occur with risk of urethral obstruction.
• Plasma testosterone and progesterone levels decrease.
• There is decreased sperm production, but fertility remains intact. Ejaculate volume decreases.
• Sexual activity in the older man is closely related to his sexual activity in earlier years.
• Vascular problems are the major causes of impotence.
The male reproductive system
The male reproductive organs are shared with the urinary tract, and disorders in functioning of one system often affect the other. For this reason, a male patient who has a disorder or dysfunction of the reproductive tract is often treated by a urologist.
Fertility
If the anatomy and physiology of the male reproductive tract are intact, sexual function is influenced by the functioning of the hypothalamus, pituitary, and testes; the metabolism and transport of sex hormones (such as GnRH and others); and the cognitive and sensory centers in the brain. A sexual desire (libido, the ability to respond to sexual stimulation with a penile erection) and the ejaculation of semen containing live sperm are necessary for fertility. Both the parasympathetic and sympathetic nervous systems influence the normal sexual response cycle.
As a man ages, there is not an abrupt cessation of gonadal hormone activity as there is in a woman. In the man, there is a gradual decrease in testosterone and other anabolic hormones, such as growth hormone and dehydroepiandrosterone (DHEA).
Contraception
Contraception is a method of preventing unwanted pregnancy. The only 100% effective method of contraception is abstinence. Abstinence is encouraged for adolescents and young adults and is taught in many school programs. However, the nurse must be able to provide contraceptive options for the many couples that prefer not to have additional children added to the family. Contraception is the responsibility of both the male and the female. Female contraception is discussed in Table 39-1.
Reversible Contraception
Reversible contraception involves the use of spermicidal creams, gels, or foams applied before intercourse to kill sperm in the vagina. These are more effective if used in conjunction with a condom. A male condom is an effective reversible contraceptive technique if it is applied and used properly. The condom sheath is typically made of latex. Proper application includes timing of application and removal, and providing a space at the tip for semen to collect. Oil-based lubricants such as petroleum jelly can cause latex to deteriorate, so these lubricants reduce reliability of latex condoms. Condoms made of polyurethane are compatible with oil-based lubricants. Latex condoms provide some protection against sexually transmitted infections (STIs).
Permanent Contraception: Vasectomy
Sterilization of the male by vasectomy is a popular method of permanent contraception. The term vasectomy refers to a surgical procedure performed on the vas deferens for the purpose of interrupting the continuity of this duct, which conveys the sperm at the time of ejaculation. This is considered a permanent procedure, but occasionally a vasectomy can be successfully reversed by vasovasotomy (microsurgery) at a later time if a man’s life circumstances change.
A vasectomy is done on an outpatient basis in a clinic or physician’s office, with a local anesthetic. An incision is made into the scrotal sac on each side, and the vas is lifted out. A segment of the vas is cut out, the ends are bound, and the incision is closed.
Instruct the patient to use ice applications and acetaminophen or ibuprofen for scrotal pain and swelling the first 12 to 24 hours postoperatively. The patient should wear jockey shorts or a scrotal support for comfort. Sexual intercourse may be resumed in about 1 week or whenever the patient finds it comfortable. Two negative sperm counts are needed after vasectomy before the patient is infertile and some form of contraception should be used until then.
Since seminal fluid is manufactured in seminal vesicles and the prostate gland, there is no decrease in semen ejaculation following a vasectomy. However, the semen does not contain sperm. After vasectomy, the sperm cells produced by the vas deferens are reabsorbed by the body. Vasectomy has no effect on libido or sexual performance, and provides no protection from STIs. Some patients consider storing fertile sperm in a sperm bank before a vasectomy. Since reversal of a vasectomy may or may not be successful, using frozen sperm at a later date to father a child remains an option.
Nursing management
Assessment (Data Collection)
Because certain kinds of male reproductive disorders predominate in certain age groups, the age of the patient is relevant to nursing assessment. In men over age 50, the assessment is directed more toward detecting prostate problems, whereas younger men are carefully assessed for STIs and testicular cancer.
It may be awkward for the new nurse to obtain a sexual and reproductive history, but with experience in interviewing male patients of all ages, she will soon become more comfortable and adept at obtaining necessary data. Because questions about urinary problems are usually less sensitive than those dealing with sexual dysfunction, it is best to begin with questions of this kind and then lead into more sensitive ones.
Open-ended questions that start out with “Tell me about …” or “When did you first notice … ” give the patient room to discuss only those things he is comfortable talking about. It also is helpful to relate his problem to the inconvenience it has caused in his daily life. For example, tenderness and discomfort in the scrotal area could make sitting at a desk or walking very difficult and interfere with getting assigned work done. Frequent urination can cause distracting and sometimes embarrassing interruptions in his work schedule or recreational activities.
Good communication depends on the sender and receiver of messages using mutually understood language. Many people do not know the medical names of their sex organs. If the nurse suspects that the patient does not understand what particular part of the body she is talking about, or if the nurse herself is not familiar with the term the patient is using, it is important to phrase questions differently or ask for clarification from the patient.
Diagnostic Tests
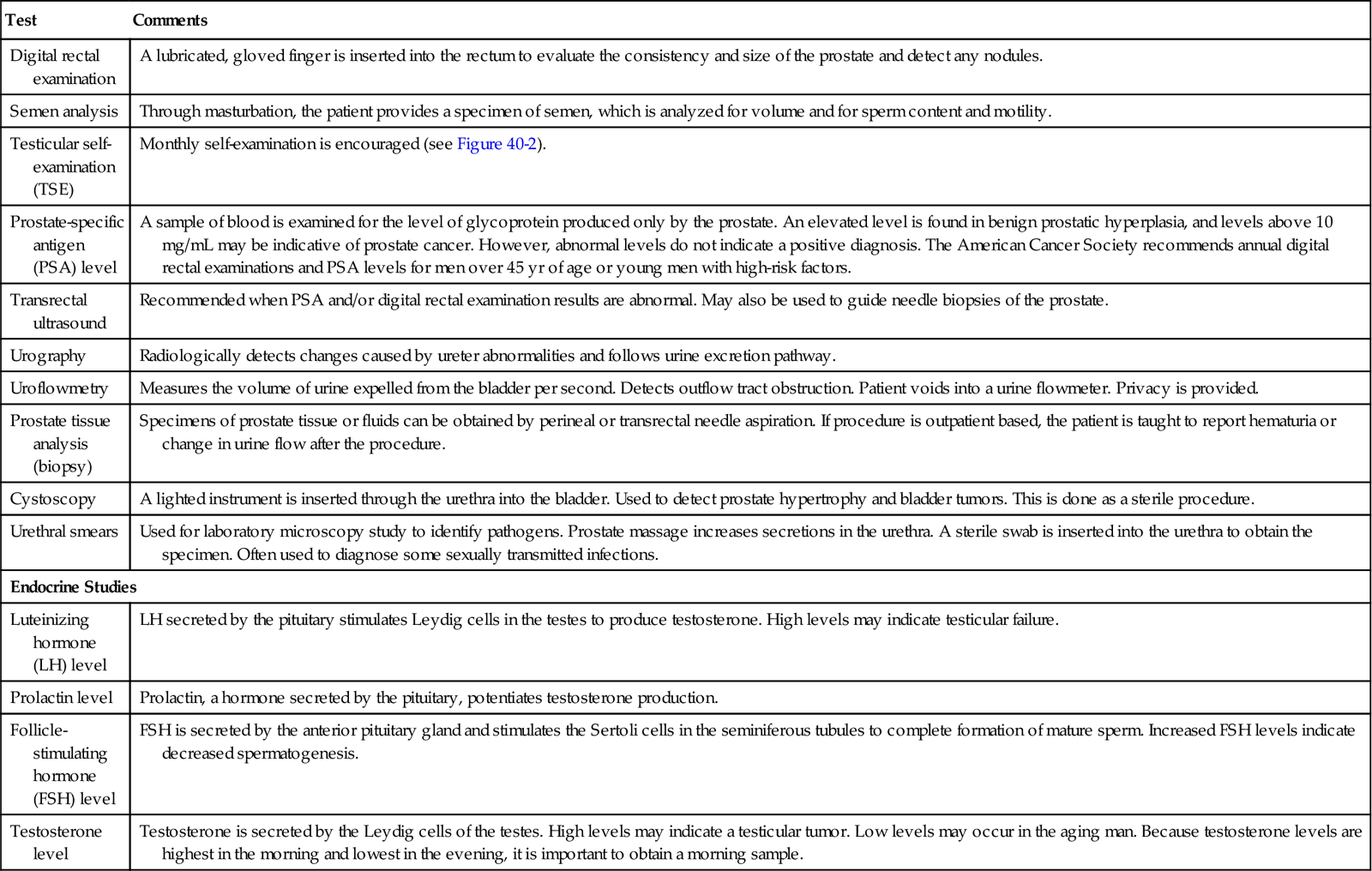
Tests for general state of health, such as complete blood cell count, urinalysis, chemistry profile, and thyroid tests, are done initially for problems concerning the male reproductive tract. Serum acid phosphatase is usually elevated in the patient with prostate cancer. Serum alkaline phosphatase is elevated if malignancy of the prostate has metastasized to the bone. A kidney-ureters-bladder (KUB) x-ray, an intravenous pyelogram, and cystoscopy with uroflowmetry studies also may be done (see Chapter 34 for more information on these tests). Blood tests are done to detect specific UTIs.
Tumor protein marker studies are performed for patients with testicular cancer for follow-up to determine the success of treatment or recurrence of the disease. The primary tumor markers are alpha-fetoprotein (AFP) and the beta subunit of human chorionic gonadotropin (beta-hCG). A prostate-specific antigen (PSA) test detects levels of a glycoprotein produced by the prostate that is elevated in prostate cancer. Diagnostic tests that relate to the male reproductive organs are summarized in Table 40-1.
Table 40-1
Diagnostic Tests for the Male Reproductive System
| Test | Comments |
| Digital rectal examination | A lubricated, gloved finger is inserted into the rectum to evaluate the consistency and size of the prostate and detect any nodules. |
| Semen analysis | Through masturbation, the patient provides a specimen of semen, which is analyzed for volume and for sperm content and motility. |
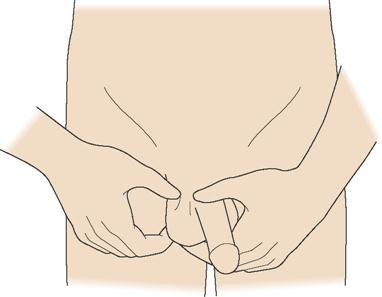
| Testicular self-examination (TSE) | Monthly self-examination is encouraged (see Figure 40-2). |
| Prostate-specific antigen (PSA) level | A sample of blood is examined for the level of glycoprotein produced only by the prostate. An elevated level is found in benign prostatic hyperplasia, and levels above 10 mg/mL may be indicative of prostate cancer. However, abnormal levels do not indicate a positive diagnosis. The American Cancer Society recommends annual digital rectal examinations and PSA levels for men over 45 yr of age or young men with high-risk factors. |
| Transrectal ultrasound | Recommended when PSA and/or digital rectal examination results are abnormal. May also be used to guide needle biopsies of the prostate. |
| Urography | Radiologically detects changes caused by ureter abnormalities and follows urine excretion pathway. |
| Uroflowmetry | Measures the volume of urine expelled from the bladder per second. Detects outflow tract obstruction. Patient voids into a urine flowmeter. Privacy is provided. |
| Prostate tissue analysis (biopsy) | Specimens of prostate tissue or fluids can be obtained by perineal or transrectal needle aspiration. If procedure is outpatient based, the patient is taught to report hematuria or change in urine flow after the procedure. |
| Cystoscopy | A lighted instrument is inserted through the urethra into the bladder. Used to detect prostate hypertrophy and bladder tumors. This is done as a sterile procedure. |
| Urethral smears | Used for laboratory microscopy study to identify pathogens. Prostate massage increases secretions in the urethra. A sterile swab is inserted into the urethra to obtain the specimen. Often used to diagnose some sexually transmitted infections. |
| Endocrine Studies | |
| Luteinizing hormone (LH) level | LH secreted by the pituitary stimulates Leydig cells in the testes to produce testosterone. High levels may indicate testicular failure. |
| Prolactin level | Prolactin, a hormone secreted by the pituitary, potentiates testosterone production. |
| Follicle-stimulating hormone (FSH) level | FSH is secreted by the anterior pituitary gland and stimulates the Sertoli cells in the seminiferous tubules to complete formation of mature sperm. Increased FSH levels indicate decreased spermatogenesis. |
| Testosterone level | Testosterone is secreted by the Leydig cells of the testes. High levels may indicate a testicular tumor. Low levels may occur in the aging man. Because testosterone levels are highest in the morning and lowest in the evening, it is important to obtain a morning sample. |
Nursing Diagnosis
Nursing diagnoses commonly used for problems of the male reproductive system may include:
• Urinary retention related to urinary obstruction
• Anxiety related to inability to empty bladder completely or dribbling
• Pain related to pressure of pelvic mass or distended bladder; surgical incisions; or bladder spasms
• Sexual dysfunction related to inability to achieve erection
• Ineffective sexuality pattern related to decreased libido
• Disturbed body image related to changes in sexual function
• Potential fluid volume excess related to bladder irrigation.
Additional nursing diagnoses may be appropriate for the patient undergoing surgery or for one who has cancer (see Chapters 4, 5, and 8).
Planning
Expected outcomes are written for individual patients based on the nursing diagnoses chosen. Interventions are planned to help the patient meet the expected outcomes. The nurse plans her interaction with the patient based on his age, educational level, degree of comfort in discussing reproductive problems, and culture.
Expected outcomes for the patient with problems of the male reproductive system are:
• Patient will have normal urinary flow without obstruction.
• Patient will have normal urinary elimination after surgery.
• Patient will have bladder spasms controlled with medication.
• Pain will be resolved after surgical recovery.
• Patient will have intact self-esteem 3 months after surgery.
• Patient will explore avenues for achieving sexual satisfaction.
• Patient will focus on positive traits and capabilities to increase a positive body image.
Implementation
Nursing actions for selected problems of the male reproductive system are found within the sections on specific disease that follow. Privacy should always be provided when assessing the genitals, performing catheter care, or doing dressing changes. There are wide variances in the degree of modesty in men. The female nurse must be especially cautious and display a matter-of-fact, respectful manner when providing care. Sensitivity to embarrassment is necessary. Rather than stating “Don’t worry; I’m used to this,” it might be better to state, “I understand that this may be embarrassing for you; I will try to be as quick about it as I can.”
Some patients express inappropriate comments when they feel that their sexuality is threatened. A male patient with sexual dysfunction, or one about to undergo surgery that may affect his sexuality, might make sexual comments or advances to a female nurse; she should be tactful and matter-of-fact in setting limits on such behavior, without taking the patient’s inappropriateness personally.
Evaluation
Evaluation assesses how effective the nursing actions are in helping the patient achieve the expected outcomes. If the actions and treatments are not achieving the desired effect, a revision in the plan of care is necessary.
Disorders of the male reproductive system
Erectile Dysfunction
Erectile dysfunction (ED), also known as impotence, is the inability to achieve or maintain an erection that is firm enough for sexual intercourse more than 25% of the time. Impotence can also involve ejaculation problems. Erectile dysfunction has both psychological and organic causes.
Factors that interfere with the mechanisms of penile erection will cause erectile dysfunction. Any condition that impairs the blood supply to the penis, impairs pathology of the nervous system or hormonal supply, or impairs psychosocial responses can interrupt the process of penile erection. Anxiety and depression can affect achieving or maintaining an erection. Organic causes can include diabetes mellitus and other endocrine disorders, disorders of the urinary tract, neurologic disorders, and chronic illness (such as sickle cell anemia, hypertension, cardiovascular disease, liver disease, and cancer). Medications and drug and alcohol abuse can interfere with sexual performance. Some antihypertensive drugs, diuretics, tranquilizers, and medications used to prevent gastroesophageal reflux disease (GERD) can cause sexual problems. Antiparkinson medications can enhance sexual desire but not the ability to perform (Wold, 2008).
A complete history and physical examination is needed to rule out any physical illness that may affect sexual performance. Sleep laboratories can monitor nighttime penile erections to detect organic causes of impotence. A Doppler probe can measure arterial flow in the penis essential for erections, and nerve conduction tests can rule out neurologic pathology related to impotence. Review the patient’s medications for side effects affecting erectile function and conduct a complete psychological evaluation for psychological causes of impotence before devising an individualized treatment plan. Studies have shown that among patients who seek help for ED, nearly 30% have undiagnosed hypertension, 15% have diabetes mellitus, and 5% have significant coronary artery disease (Jackson et al., 2006).
Treatment
Medical treatment depends on the cause of ED. Medical conditions are treated, the medications prescribed are reviewed and adjusted, hormone therapy may be prescribed for hypothalamic-pituitary disorders, and vascular surgery may be indicated for penile blood flow obstruction.
The primary intervention for ED is modifying reversible causes of the problem. Drug therapy includes phosphodiesterase (PDE-5) inhibitors, taken an hour before sexual activity. These drugs should not be taken with nitrate-based drugs used for heart problems, as a serious drop in blood pressure can occur from the combination. If these methods fail to resolve ED, surgical interventions include inserting a penile implant that can be rigid or flexible. One type of implant includes a pump, inflatable cylinders, and a reservoir for emptying after erection. The erection produced is usually firm enough to enable intercourse (Figure 40-3). Complications of oral therapy include priapism, a persistent abnormal erection that can develop into a urologic emergency. Treatment options are presented in Table 40-2.
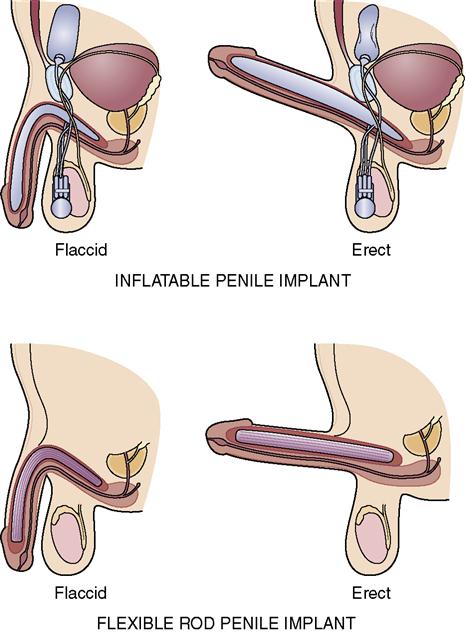
Table 40-2
Treatment Options for Erectile Dysfunction
| Option | Comment |
| Medications Taken About 1 Hour Before Intercourse | |
PDE-5 InhibitorsStay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |