CHAPTER 4. Forensic Epidemiology and the Forensic Nurse
Steven A. Koehler
A new field of science has emerged that is part forensic science and part epidemiology. It is called forensic epidemiology. This chapter provides an overview of the development of the field; roles within the forensic and public health fields; their functions in different settings; how forensic epidemiologists identify, collect, examine, and present forensic data; and how those within the fields of forensic, law enforcement, nursing, public health, and medical research utilize the data collected by the forensic epidemiologist. This chapter also examines the roles that nurses and forensic nurses play in the identification, collection, and documentation of forensic evidence and how those data are used within the field of forensic epidemiology with emphasis on death investigations conducted by the medical examiner/coroner’s (ME/C) office.
Development/Definition of Forensic Epidemiology
In the past, there was not much interaction between the investigations carried out by law enforcement and those conducted by public health authorities. The classic health inspector would examine a restaurant and had the power to fine or even close the establishment without involvement of the police. The risk to the public was mainly from food contamination resulting from improper storage, cross-contamination, or poor hygiene practices. However, in today’s society, the deliberate contamination of water, food, air, or land as an act of bioterrorism has become very real. Working alone, law enforcement may not initially recognize these incidences as a bioterrorism threat; the same holds true for public health personnel. The problem is that law enforcement personnel are not trained to spot these types of crimes. On the other hand, public health care personnel are able to detect abnormal or unseasonable increases in illness or types of death but are ill-equipped in the proper protocols in identifying, collecting, and preserving forensic evidence. An unusual or off-season increase in a specific strain of virus would not raise suspicion among police officers, but it would be alarming to those in the public health setting. In turn, public health personnel are not trained in the legal methods and procedures of collecting, preserving, and chain-of custody documentation required to bring a case to trial.
Beginning in the late 1970s, joint investigations involving law enforcement and public health authorities began (Goodman, 2003). These investigations centered on health problems that were suspected to have been intentionally caused or crimes that had potentially significant public health consequences. Examples include foodborne outbreaks caused by intentional contamination of food products (Torok, Tauxem, & Wise, 1997) or, in the case of the “Angel of Mercy” syndrome, where healthcare providers deliberately assisted patient deaths by administering lethal doses to their patients (Buehler, Smith, & Wallace, 1985; Franks, Sacks, & Smith, 1987; Istre, Gustafson, & Baron 1985; Sacks, Herdon, & Lieb, 1988; Sacks, Stroup, & Will 1988; Stross, Shasby, & Harlan, 1976).
During the late 1990s, the term forensic epidemiologists typically referred to traditionally trained epidemiologists who functioned as expert witnesses in civil trials. They testified to issues relating to methodology of the study: number of subjects, subject selection and exclusions, length of the study, methods of analysis, interpretation of the results, and any other limitations. They were also frequently called on to address issues relating to association, such as exposure levels of certain chemicals to certain birth defects or the association of performing a task repeatedly and carpal tunnel syndrome (Last, 1988; Lane, 2004).
The term forensic epidemiology was first associated with bioterrorism in 1999 when the former chief deputy of the USSR bioweapon program, Ken Alibek, used the term. Forensic epidemiology was defined then as the activity that would help distinguish natural from manmade epidemics. After the anthrax attacks in September and October of 2001, Dr. Julie Gerberding, a senior official with the Centers for Disease and Control (CDC) National Center for Infectious Disease, defined forensic epidemiology as that practiced by an epidemiologist who would be trained to respond to bioterrorism attacks as well as other public health emergencies.
The events of 2001 underscored the need for law enforcement and public health personnel to work together to conduct joint investigations, especially those centered around a possible bioterrorism event. In 2002, the CDC developed the “The Forensic Epidemiology: Joint Training for Law Enforcement and Public Health Officials on Investigation Reponses to Bioterrorism.” A joint collaboration was also conducted between the CDC and the Federal Bureau of Investigation (FBI) that resulted in the “Criminal and Epidemiological Investigation Handbook” (Criminal and Epidemiological Investigation Handbook, 2005). Many states have developed courses specifically designed to help law enforcement officers operate closely and more effectively with public health officers when investigating a public health problem that may have been caused intentionally or with crimes that have a public health consequence. This is accomplished by familiarizing officers with the basic principles of public health and the epidemiological approach to investigation (Forensic Epidemiology, 2007).
In 2002, several definitions of forensic epidemiology emerged. They included (1) the use of epidemiological methods as part of an ongoing investigation of a health problem for which there are suspicions or evidence regarding possible intentional acts or criminal behavior as factors contributing to the health problem and (2) the use of epidemiological and other public health methods in conjunction with or an adjunct to an ongoing criminal investigation (Koehler & Brown, 2009).
Roles of Forensic Epidemiology
The field of forensic epidemiology, while initially developed to focus on acts of bioterrorism, has expanded its role to include the investigation of deaths and various types of crimes. A forensic epidemiologist can play a vital role in many other types of health emergencies and further threats to public health by examining a number of diverse crimes ranging from environmental to foodborne offenses. Some examples include the following:
• Environmental crimes, such as the improper disposal of hazardous waste that may result in human illness (cancer) or death
• Foodborne disease outbreaks, such as that caused by a food-processing plant that intentionally ignores safety protocols (Buchholz, Mermin, & Rios, 2002)
• Automobile repair shops that use inferior parts to save money, resulting in the increase of motor vehicle accidents
• Natural and unnatural deaths investigated by the ME/C office
Forensic epidemiologists are employed in ME/C’s offices, local or state health departments, public health sectors, schools of public health, private organizations (as private consultants), and as expert witnesses (Wecht, 2004).
Medical examiner/coroner’s offices
The roles of forensic epidemiologists within a ME/C office includes systematic coding of the vast amount of forensic data collected during death investigations; conducting detailed data analysis; and providing data summaries of the deaths for the general public, the news media, law enforcement, and public health officers. They also offer assistance in academic research by conducting research studies and preparing manuscripts for peer-review publications.
Health department
Functions of forensic epidemiologists employed in state and local health departments include the collection of data regarding the births and deaths of the residents by reviewing information contained on the birth records and death certificates, both fetal and non-fetal. These are used to create the vital statistic reports, which include live births and mortality data regarding the specific area, region, or state. The mortality data include a detailed listing of the cause of death differentiating each type of death (natural and unnatural) by age, sex, and race and are also listed based on the International Classification of Disease (ICD).
The ability of forensic epidemiologists, public health personnel, forensic nurses, researchers, and others in the health care community to examine multiple years of vital statistics data could assist them in gaining a comprehensive interpretation of the changes, patterns, and magnitude of illness, injury, or specific causes of death within a specific region or an entire state. In addition, vital statistics data allow for trend analysis, which is critical for highlighting changes in death patterns, recognizing the emergence of specific deaths in specific areas, and emphasizing areas to target prevention programs or a need for increased police presence.
Public/private organizations
Many organizations require mortality data in order to gain funding for their particular study. These organizations employ forensic epidemiologists to locate, collect, and analyze the data using scientific methodology. Grants or funding agencies typically require a forensic epidemiologist on projects that involve the ascertainment, collection, and analysis of forensic data. Some current examples of using a forensic epidemiologist in studies include the following:
SIDS Deaths
An organization is applying for funding to implement an intervention program with the goal of lowering the number of sudden infant death syndrome (SIDS) deaths in a specific region (Willinger, James, & Catz, 1991). The forensic epidemiologist’s role would be first to obtain copies of all SIDS deaths in that region over the previous five years in order to establish an annual baseline number of death from SIDS. Next, the forensic epidemiologist would construct a profile of the characteristics of the SIDS deaths and review the intervention protocol. She or he would then monitor the number and circumstances of the SIDS death during the intervention period. At the conclusion of the study, the number and rate of SIDS death before and after the intervention period would be compared in order to statistically prove any effect on the number of deaths and, more importantly, any decreases associated with the intervention or some other variables (American Academy of Pediatrics, Task Force on Infant Positioning and SIDS, 1996; American Academy of Pediatrics, Task Force on Infant Sleep Position and SIDS, 2000; American Academy of Pediatrics, Task Force on Infant Sleep Positioning and SIDS 1992).
Drug Prevention Program for Students of Middle- and High-School Age
An organization is interested in obtaining funding to implement a drug prevention program targeting students in high school and middle school. The first step is to determine the magnitude of the drug abuse problem in that age group. This involves the collection and review of all forensic data from the deaths of all persons between 12 and 18 years old examined at the ME/C office. The deaths would further be scrutinized to reveal deaths caused by drug overdose, motor vehicle accidents involving alcohol or drugs, suicides with a high level of drugs detected in the blood, or homicides that were directly related to dealing or buying drugs—all of which are related to the drug abuse problem. From these statistics, the forensic epidemiologist will provide an overview of the drug problem, develop a profile of the typical victim of drug abuse, and, most importantly, supply information on the target population for the prevention program in order to obtain the most significant outcome (Drug Abuse Warming Network: Development of a New Design, 2002).
Private consultants
Forensic epidemiologists also function as forensic consultants. Forensic consultants are often contacted when there are questions regarding the determination of the cause or manner of death, whether the level of the death investigation conducted was substandard, or whether a private forensic autopsy is warranted. Families and attorneys typically hire them to review the components of the death investigation, including an evaluation of medical records, a review of autopsy reports, police reports, and technical data; and an interpretation of the level of investigation and appropriateness of evidence testing. Law firms and individual attorneys also hire forensic consultants to advise them; answer questions regarding medical, scientific, or forensic investigation procedures; or explain the results.
On completion of the evaluation, forensic consultants provide a written report indicating their professional judgment. This report helps those who hired the consultant to determine how to proceed with the case. This activity is conducted outside of the courtroom.
Expert witness
Forensic epidemiologists are playing an ever-increasing role as expert witnesses in the courtroom. An expert witness is an individual who, through training, experience, or education, has special and precise knowledge in a specific field. Lawyers need these expert witnesses to assist them during the pretrial evaluation of the evidence. Expert witnesses are also hired to testify in a court of law to express their opinions regarding a particular aspect of a case.
Basics of Forensic Epidemiology
Forensic epidemiologists use data collected from various sources, including the death scene investigations, police reports, autopsies, toxicology results, death certificates, and medical records. This information is used to present everything from a general overview of the death to detailed characteristics of various types of death. Types of death include suicide, homicide, motor vehicle accidents (MVAs), drug overdoses, industrial accidents, falls, fires, and medical misadventures. The following are some examples of the types of investigation generated by the data analysis conducted by forensic epidemiologists.
Natural deaths
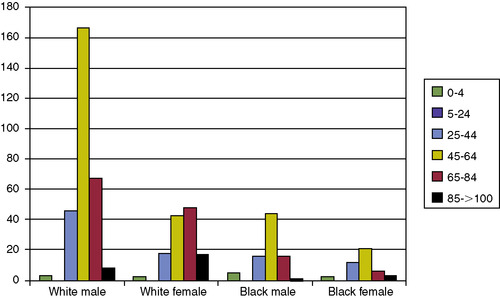
All forensic epidemiological analysis, regardless of the type or manner under investigation, begins by an examination of the demographic characteristics; these include the total yearly number, age, sex, and race. The basic epidemiological profile is important to show the characteristics of individuals who are at greatest risk of dying from a particular disease or injury. This information is also important for identifying the population most at risk in that specific region. Table 4-1 shows the demographic characteristics of natural death among cases examined at the coroner’s office between 1998 and 2005. The deaths are then displayed in terms of age, sex, and race. Figure 4-1 illustrates natural deaths, by age, sex, and race, that occurred in 2005 (Wecht, 2005). Building on this basic information, the forensic epidemiologist carries out more detailed examinations.
| Race/Sex | 1998 Number (%) | 1999 Number (%) | 2000 Number (%) | 2001 Number (%) | 2002 Number (%) | 2003 Number (%) | 2004 Number (%) | 2005 Number (%) |
|---|---|---|---|---|---|---|---|---|
| White male | 277 (57.5) | 226 (49.7) | 268 (52.5) | 264 (54.4) | 262 (51.5) | 313 (55.1) | 294 (53.2) | 260 (52.2) |
| White female | 101 (21.0) | 112 (24.6) | 108 (21.2) | 119 (24.5) | 128 (25.2) | 138 (24.3) | 130 (23.5) | 127 (25.5) |
| Black male | 61 (12.6) | 78 (17.1) | 85 (16.7) | 59 (12.2) | 76 (14.9) | 67 (11.8) | 84 (15.2) | 67 (13.4) |
| Black female | 40 (8.3) | 31 (6.8) | 47 (9.2) | 41 (8.4) | 39 (7.7) | 47 (8.3) | 44 (7.9) | 42 (8.4) |
| Other | 3 (0.6) | 7 (1.5) | 2 (0.4) | 1 (0.2) | 3 (0.6) | 3 (0.5) | 1 (0.2) | 2 (0.4) |
| Total | 482 | 454 | 510 | 485 | 508 | 568 | 553 | 498 |
The next level of forensic epidemiological investigation would be to examine the deaths in greater detail by grouping them according to information obtained from the death certificate. One method is to group the deaths into broad organ or system categories as shown in Table 4-2.
| Total Number of Deaths | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 |
|---|---|---|---|---|---|---|
| Heart-related deaths | 312 | 358 | 368 | 412 | 400 | 380 |
| Vascular system–related deaths | 4 | 13 | — | — | — | — |
| Respiratory system deaths | 45 | 38 | 40 | 35 | 44 | 37 |
| Hepatobiliary system deaths | 19 | 13 | 18 | 20 | 24 | 24 |
| Gastrointestinal tract deaths | 9 | 14 | 12 | 17 | 15 | 8 |
| Pancreatic disorder–related deaths | 1 | 2 | 1 | — | 1 | 1 |
| Lymphatic system–related deaths | 2 | 1 | — | — | — | — |
| Renal system–related deaths | 2 | — | 2 | 4 | 3 | 4 |
| Female reproductive system–related deaths | 6 | 4 | 4 | 1 | — | — |
| Endocrine system–related deaths | 5 | 6 | 9 | 8 | 7 | 6 |
| Nervous system–related deaths | 29 | 21 | 33 | 49 | 40 | 20 |
| Congenital deaths | — | 1 | — | — | — | — |
| Infectious deaths | — | 2 | 8 | 11 | 5 | 3 |
| Cancer deaths | 5 | 1 | 3 | 3 | 1 | 2 |
| Immunological disorder–related deaths | 1 | — | 1 | 1 | 2 | — |
| Connective tissue disease–related deaths | — | — | 1 | — | — | — |
| Psychiatric deaths | — | — | — | — | 3 | 1 |
| Systematic deaths | — | — | — | — | 2 | 1 |
| Blood-related deaths | — | — | — | — | — | 2 |
| Sudden infant death syndrome | 13 | 11 | 8 | 7 | 6 | 9 |
| Total deaths | 510 | 485 | 508 | 568 | 553 | 498 |
The next phase is to break down each general grouping to the specific disease condition or organism that caused the death. Table 4-3 presents examples of methods of breaking down deaths involving the respiratory system deaths and those involving the hepatobiliary system (Robbins, 1989).
| Causes of Death |
|---|
| Total Number of Respiratory System Deaths |
| Pulmonary embolism (PE) and infarction |
| Pneumonia (acute/bronchopneumonia/hemorrhagic) |
| Bronchitis |
| Chronic obstructive pulmonary disease (COPD) |
| Asthma |
| Pulmonary thrombosis |
| Carcinoma of the lungs |
| Suppurative pleuritis |
| Invasive squamous cell carcinoma |
| Total Number of Hepatobiliary System Deaths |
| Liver cirrhosis |
| Fatty liver |
| Steatosis of liver |
| End-stage liver disease |
| Liver cancer |
The next step would be to create a profile of the demographic features (age, sex, and race), location of death, and level of treatment within each subcategory. For example, what was the average age of victims who died from asthma? Did these individuals die in their residence, in the emergency department, or in the operating room, and was that condition diagnosed correctly on admission?
A psychiatric nurse at the VA hospital calls the medical examiner’s office to report the death of Mr. Fox, a 54-year-old patient with a history of schizophrenia. The ME was willing to release the body directly to the funeral home and have the patient’s physician sign the death certificate as a natural death due to complications associated with schizophrenia. However, the psychiatric nurse, who has cared for this patient for a number of years, insisted that he was compliant with his medications and showed periods of improvements and did not believe their assessment of the cause of death and strongly asked that a complete autopsy be conducted. The ME’s office acquiesced and asked the nurse to make a copy of his medical records and prepare the body for transport to the morgue. The results of the complete autopsy revealed that the heart was cardiomyopathy (583 grams) and there was 90% occlusion to the right coronary artery. Because of the nurses deep understanding of her patient’s history and insistence that a complete forensic examination be conducted, the death was correctly classified as a cardiac related death not a psychiatric death. This type of action and involvement ensures the accuracy of death certificates and the national vital statistics that rely on them.
Drug overdose
The investigation of accidental drug overdose (OD) begins by an examination of the demographic characteristics (total yearly number, age, sex, and race). This is used to create an epidemiological profile to show the individuals who are at greatest risk of dying from a drug OD. Table 4-4 shows the demographic characteristics of OD death by age, sex, and race among cases examined at the coroner’s office in 2005. The analysis revealed that accidental OD was predominant among white males and among individuals between 40 and 49 years old. The analysis also highlights the fact that there were no deaths among individuals younger than 20 years old. This type of data provides important information of where to target intervention programs (U.S. Drug Enforcement Administration). Once the basic profile of the victims has been established, the drugs involved are examined. Table 4-5 is a partial list of the drugs detected during the screening of accidental drug deaths. Building on this basic information, the forensic epidemiologist carries out more detailed examinations.
| Age | White Male | White Female | Black Male | Black Female | Total |
|---|---|---|---|---|---|
| 20-24 | 12 | 4 | — | — | 16 |
| 25-29 | 13 | 8 | 1 | — | 22 |
| 30-34 | 7 | 3 | 2 | — | 12 |
| 35-39 | 19 | 8 | 3 | 1 | 31 |
| 40-44 | 29 | 10 | 3 | 2 | 44 |
| 45-49 | 26 | 10 | 6 | 4 | 46 |
| 50-54 | 18 | 8 | 5 | 2 | 33 |
| 55-59 | 5 | 1 | 4 | 1 | 11 |
| 60-64 | — | 2 | 1 | — | 3 |
| 65-70 | — | — | 1 | — | 1 |
| >70 | 1 | — | 1 | — | 2 |
| Total (%) | 130 (58.3%) | 54 (24.2%) | 27 (12.1%) | 10 (4.5%) | 223 (223 total does not include one 23 year-old Asian male and one white male fetus) |
| ONE DRUG: TOTAL 90 | |
| Heroin | 25 |
| Cocaine | 28 |
| Alcohol | 13 |
| Morphine | 4 |
| Fentanyl | 3 |
| Oxycodone | 2 |
| Methadone | 4 |
| Metoprolol | 1 |
| Phenobarbital | 1 |
| Paroxetine | 1 |
| Opiates | 7 |
| Salicylate | 1 |
| TWO DRUGS: TOTAL: 77 | |
| Heroin + Alcohol | 8 |
| Heroin + Cocaine | 28 |
| Heroin + Methadone | 1 |
| Heroin + Hydrocodone | 1 |
| Heroin + Fentanyl | 1 |
| Alcohol + Zolpidem | 1 |
| Alcohol + Opiates | 2 |
| Alcohol + Methadone | 2 |
| Alcohol + Oxycodone | 4 |
| Cocaine + Methadone | 4 |
| Cocaine + Morphine | 3 |
| Cocaine + Opiates | 7 |
| Cocaine + Alcohol | 1 |
| Cocaine + Oxycodone | 4 |
| Cocaine + Fentanyl | 1 |
| Morphine + Olanzapine | 1 |
| Methadone + Morphine | 1 |
| Methadone + Fentanyl | 1 |
| Methadone + Alprazolam | 1 |
| Methadone + Nortriptyline | 1 |
| Oxycodone + Hydrocodone | 2 |
| Opiates + Benzodiazepines | 1 |
| Clozapine + Clomipramine | 1 |
| THREE DRUGS: TOTAL: 38 | |
| Heroin + Cocaine + Alcohol | 4 |
| Heroin + Cocaine + Methadone | 1 |
| Heroin + Cocaine + Diazepam | 1 |
| Heroin + Cocaine + Paroxetine | 1 |
| Heroin + Alcohol + Doxepin | 1 |
| Heroin + Alcohol + Benzodiazepines | 1 |
| Heroin + Methadone + Alprazolam | 1 |
| Heroin + Propoxyphene + Tramadol | 1 |
| Methadone + Benzodiazepines + Amitriptyline | 1 |
| Methadone + Alprazolam + Oxycodone | 1 |
| Methadone + Trazodone + Nortriptyline | 1 |
| Methadone + Diazepam + Alprazolam | 1 |
| Methadone + Alprazolam + Sertralines | 1 |
| Alcohol + Cocaine + Hydrocodone | 1 |
| Alcohol + Cocaine + Amitriptyline | 1 |
| Alcohol + Cocaine + Amoxapine | 1 |
| Alcohol + Cocaine + Methanol | 1 |
| Alcohol + Morphine + Trazodone | 1 |
| Alcohol + Methadone + Alprazolam | 1 |
| Alcohol + Codeine + Phenobarbital | 1 |
| Alcohol + Oxycodone + Benzodiazepines | 1 |
| Oxycodone + Alprazolam + Methadone | 1 |
| Oxycodone + Hydrocodone + Alprazolam | 1 |
| Oxycodone + Methadone + Meprobamate | 1 |
| Cocaine + Fentanyl + Phenobarbital | 1 |
| Cocaine + Fentanyl + Diazepam | 1 |
| Cocaine + Methadone + Opiates | 1 |
| Cocaine + Opiates + Benzodiazepines | 2 |
| Cocaine + Methadone + Alprazolam | 1 |
| Cocaine + Meprobamate + Methadone | 1 |
| Cocaine + Morphine + Methadone | 1 |
| Cocaine + Oxycodone + Alprazolam | 1 |
| Fentanyl + Tramadol + Diazepam | 1 |
| Hydrocodone + Alprazolam + Cyclobenzaprine | 1 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access