AIRBORNE PRECAUTIONS
Airborne transmission involves infected microorganisms or dust particles that remain suspended in the air for long periods of time and can be dispersed widely by air currents. Depending on environmental factors, a susceptible host may inhale particles within the same room or over a longer distance from the source patient. Special air handling and ventilation are required to prevent airborne transmission. In addition to standard precautions, airborne precautions include placement of the patient in a negative pressure room, use of respiratory protection such as an N95 respirator, and limitation of patient transport.
DROPLET PRECAUTIONS
Droplets can be transmitted from coughing, sneezing, and talking, and during certain procedures such as suctioning and bronchoscopy. Transmission is via the host’s conjunctivae, nasal mucosa, or mouth. Droplets do not remain suspended in the air, and as such ventilation is not needed. Do not confuse with airborne transmission. In addition to standard precautions, droplet precautions include placement of the patient in a private room, use of a mask (especially when within 3 feet of the patient), and limited patient transport.
CONTACT PRECAUTIONS
Contact is the most frequent mode of transmission of nosocomial infections and is divided into direct- and indirect-contact transmission.
Direct-contact transmission involves a body-to-body contact resulting in the physical transfer of microorganisms, such as bathing or turning a patient.
Indirect-contact involves a susceptible host touching a contaminated object, such as instruments, needles, or dressings, or hands that are not washed and gloves that are not changed between patients. Gloves should always be utilized in contact precautions. Gowns should be worn if there will be body-to-body contact or the patient has diarrhea, an ostomy, or excessive wound drainage. Before leaving the room, remove gloves and gown and thoroughly wash hands; be sure to avoid contact with any contaminated surfaces.
Variant Creutzfeldt-Jakob Disease Precautions
Additional special precautions are necessary for handling and decontamination of blood, body fluids and tissues, and contaminated items from patients with confirmed or suspected variant Creutzfeldt-Jakob disease. See Variant Creutzfeldt-Jakob Disease later in this chapter, the latest College of American Pathologists (Northfield, Illinois) guidelines, or the WHO website. WHO has developed CJD infection control guidelines that can be a valuable guide to infection control personnel and other healthcare workers involved in the care of CJD patients. Destruction of heat-resistant surgical instruments that come in contact with high infectivity tissues, albeit the safest and most unambiguous method described in the WHO guidelines, may not be practical or cost effective.
QUARANTINABLE INFECTIOUS DISEASES
Federal law further stipulates that isolation and quarantine are mandated for certain communicable diseases through executive order of the President. These communicable diseases include the following:
• Cholera
• Diphtheria
• Infectious tuberculosis
• Plague
• Smallpox
• Yellow fever
• Viral hemorrhagic fevers (Lassa, Marburg, Ebola, Crimean-Congo, South American, and others)
• Severe acute respiratory syndrome
• Novel or reemergent influenza viruses that may cause a pandemic
See the following sections in Chapter 18: Isolation and Quarantine and CDC Quarantine Authority.
EMERGING INFECTIOUS DISEASE DESCRIPTIONS
This handbook covers the following emerging infectious diseases (EIDs):
• Avian influenza (bird flu)
• Monkeypox
• Nipah virus infection
• Norwalk-like viruses
• Pandemic influenza
• Severe acute respiratory syndrome (SARS)
• Variant Creutzfeldt-Jakob disease
• West Nile fever
For information on bioterrorism agents, please see Chapter 6.
For each disease, the following information is provided:
• Diagnosis synopsis
• Weaponization
• Transmission/isolation
• Incubation, onset, and mortality
• Patient assessment/recognition
• Clinical diagnostic tests
• Patient management
• Therapy
• Personal safety risk
• Precautions
• Family safety/leaving work
• Prophylaxis/vaccine
• Public health reporting
AVIAN INFLUENZA (BIRD FLU)
EID DESCRIPTION: AVIAN INFLUENZA (BIRD FLU)
Diagnosis Synopsis
Bird flu is an infection caused by avian influenza viruses. These flu viruses occur naturally among wild birds, which carry the viruses in their intestines. The H5N1 virus, a subtype of influenza A virus, circulates among birds worldwide and is very contagious and deadly to birds. To date, cases of wild birds and poultry with avian flu have appeared throughout Asia and have spread to birds in Europe and the Middle East.
The H5N1 virus does not usually infect humans; however, transmission from birds to people has been recorded. Most of these cases occurred from contact with infected poultry or contaminated surfaces.
Transmission of the H5N1 virus from person to person has been rare and has not continued beyond one person. However, since these viruses do not commonly infect humans, there is little or no immune protection against them in the human population. However, it is believed the virus may mutate over time, resulting in human-to-human transmission. This is referred to as “antigenic shift,” which is an abrupt, major change in the virus resulting in a new subtype for which most people have little or no protection. An antigenic shift may result in a global pandemic. A vaccine for H5N1 is currently in the testing stages through the National Institute of Allergy and Infectious Diseases.
Weaponization
Aerosol inhalation.
Incubation, Onset, and Mortality
• Incubation: 2 to 3 days
• Onset: 3 days
• Mortality: 50%
Transmission/Isolation
• Transmission between persons is rare.
• Isolate patients in a negative pressure room.
• Avian influenza is a federally mandated quarantinable disease.
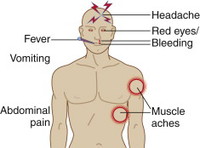
Patient Assessment/Recognition
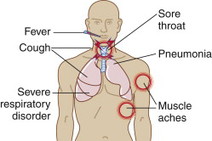
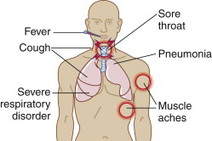
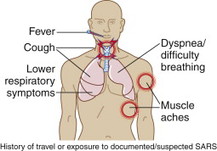
 |
Look for typical influenza-like symptoms such as fever, cough, sore throat, and muscle aches. In addition, one or more of the following symptoms may or may not be seen: conjunctivitis, pneumonia, severe respiratory disorder, viral pneumonia, and other severe complications.
Atypical presentations of avian influenza have been reported. Patients have developed nausea, vomiting, and diarrhea preceding acute respiratory failure.
Progression to acute respiratory distress syndrome (ARDS) and respiratory failure is common. Complications have included bacterial sepsis, pulmonary hemorrhage, and multi-organ failure.
The mortality of hospitalized patients has been high because of progressive respiratory failure.
Clinical Diagnostic Tests
• Viral culture
• Immunofluorescence antibody (IFA)
• Serologic studies
• Polymerase chain reaction (PCR)
Patient Management
Patients with H5N1 should receive care in single rooms to prevent direct or indirect transmission.
Therapy
• Is resistant to amantadine and rimantadine.
• Consider oseltamivir and zanamivir when treating patients, since both are thought to be effective in treatment and prevention of avian influenza.
Personal Safety Risk
 Currently, risk is low. However, if person-to-person transmission occurs, there will be a high risk to personal safety.
Currently, risk is low. However, if person-to-person transmission occurs, there will be a high risk to personal safety.Precautions
Droplet, contact, and airborne precautions.
Family Safety/Leaving Work
 Low: According to the CDC, the spread of avian influenza viruses from an ill person to another person has been reported very rarely, and transmission has not been observed to continue beyond one person. Despite low transmission risk, thorough hand washing and changing clothes before returning home are suggested.
Low: According to the CDC, the spread of avian influenza viruses from an ill person to another person has been reported very rarely, and transmission has not been observed to continue beyond one person. Despite low transmission risk, thorough hand washing and changing clothes before returning home are suggested.Prophylaxis/Vaccine
None available.
Public Health Reporting
Novel influenzas, including avian influenza, are reportable to state and local health departments.
MONKEYPOX

EID DESCRIPTION: MONKEYPOX
Diagnosis Synopsis
Monkeypox is a rare zoonotic orthopox virus infection that is clinically similar to smallpox. Human monkeypox primarily has been limited to the rain forest areas of central and west Africa; however, in 2003 cases were reported in Wisconsin, Illinois, and northwestern Indiana. This was the first time that cases were reported in the western hemisphere. Patients from this outbreak reported direct or close contact with infected prairie dogs. To sustain the disease in the human population, it is believed repeated animal reintroduction of monkeypox virus is needed. The disease usually lasts between 2 and 4 weeks in humans.
Weaponization
Aerosol inhalation.
Incubation, Onset, and Mortality
• Incubation: 12 days
• Onset: 1 to 3 days
• Mortality: 1% to 10%
Transmission/Isolation
• Transmitted through direct contact with the infected animal’s blood, body fluids, or lesions.
• Can be spread from person to person by large respiratory droplets during direct and prolonged face-to-face contact or through direct contact with body fluids.
• Monkeypox is not as contagious as smallpox.
• Isolate patients in a negative pressure room.
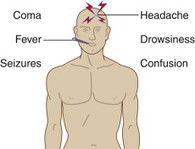
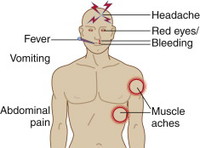
Patient Assessment/Recognition
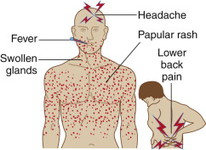
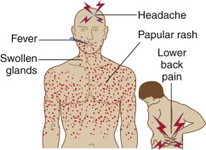
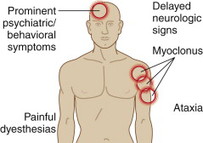 |
Look for fever, headache, backache, and swollen glands, as well as a papular rash covering the face, trunk, and extremities that typically progresses through stages of vesiculation, pustulation, umbilication, and crusting.
In some patients seen in the United States in 2003, early lesions became ulcerated. In addition to lesions on the head, trunk, and extremities, patients can have initial and satellite lesions on the palms, soles, and extremities. Rashes can generalize in some patients.
Clinical Diagnostic Tests
• Viral culture
• PCR
• Electron microscopy
• Immunohistochemical testing methods
Patient Management
• Therapy is primarily supportive.
• Cidofovir has been suggested as a possible treatment option in severe, life-threatening cases only.
• Patients who do require hospitalization should be placed in a negative pressure isolation room on contact, droplet, and airborne precautions; if a negative pressure room is not available, a private room should be used.
Therapy
The CDC recommends a smallpox vaccination within 2 weeks of exposure, ideally within 4 days, for exposed healthcare workers and household contacts of confirmed cases. People with weakened immune systems should not get the smallpox vaccine.
Personal Safety Risk
 Medium risk to personal safety.
Medium risk to personal safety.Precautions
Droplet, airborne, and contact precautions.
Family Safety/Leaving Work
 Low: Minimal risk to family since monkeypox is not highly contagious.
Low: Minimal risk to family since monkeypox is not highly contagious.Prophylaxis/Vaccine
Smallpox vaccine.
Public Health Reporting
Monkeypox is reportable in Massachusetts, Michigan, New York, North Carolina, and Virginia.
NIPAH VIRUS INFECTION

EID DESCRIPTION: NIPAH VIRUS INFECTION
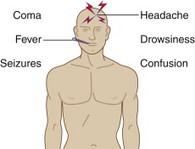
Diagnosis Synopsis
Nipah virus infection is caused by a zoonotic virus belonging to the Paramyxoviridae family. It is transmitted to humans by pigs; however, cats and dogs may also become infected. The natural host of the virus is believed to be fruit bats (genus Pteropus), although it is not known how the bats transmit the disease to animals. The disease can have subclinical presentations where patients are asymptomatic. Nipah virus infection has only been seen in Asia and has caused a relatively mild disease in pigs in both Malaysia and Singapore. Nearly half of all survivors suffer permanent neurological sequelae.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


