Section 4 Common conditions in children and reasons for admission
4.1 General conditions in children: a systems approach
Principles of cellular death, injury and repair
Cellular death/hypoxic damage
 generalized ischaemia (hypovolaemia, hypoxaemia or conditions such as disseminated intravascular coagulation (DIC))
generalized ischaemia (hypovolaemia, hypoxaemia or conditions such as disseminated intravascular coagulation (DIC))
 ischaemia of an organ (acute tubular necrosis of the kidney)
ischaemia of an organ (acute tubular necrosis of the kidney)
 ischaemia of the skin or limb (compression bandages or constrictive devices, such as a tight cast that has been improperly left in place for extended periods of time, crush or pressure injuries, pressure ulcers, swelling of a foot, leg or arm due to fractures or compartment syndrome.
ischaemia of the skin or limb (compression bandages or constrictive devices, such as a tight cast that has been improperly left in place for extended periods of time, crush or pressure injuries, pressure ulcers, swelling of a foot, leg or arm due to fractures or compartment syndrome.
All of these and others can lead to hypoxic injury (Table 4.1), which can affect viability of tissue and its surrounding area. The hypoxic damage may either occur inside the body and is invisible to the naked eye or appear on the surface of skin and be visible. Those areas of hypoxic damage that are invisible are generally due to acute tubular necrosis. Hypoxic injury that is visible is due to occlusions of limbs or pressure ulcers, which may lead to the appearance of offensive unsightly necrotic wounds, which do not heal.
Table 4.1 The conditions that lead to cell death, injury and repair
| Inflammatory response | Hypoxic damage | Oedema |
|---|---|---|
| Trauma Head injury (cerebral oedema) Surgery/anaesthetic Renal/liver disease Pancreatitis Burns Gastro-intestinal disorders: ulcers hernia irritable bowel syndrome inflammatory bowel disease ulcerative colitis Infection / sepsis Pulmonary oedema Drugs Hypertension Heart failure Malnutrition Anaphylaxis Neoplasms Leg ulcers | Hypovolaemia/hypotension Tight compression bandages/casts Compartment syndrome Myocardial infarction/cardiac arrest Shock Heart failure Deep vein thrombosis Pulmonary embolism Acute tubular necrosis Pressure ulcers Cerebral thrombosis or bleed Peripheral vascular disease Neoplasms | Cancer Malnutrition Congestive cardiac failure Fluid overload Left ventricular failure |
These processes are not mutually exclusive. The inflammatory response can lead to interstitial oedema causing swelling which can cut off blood supply, leading to hypoxic damage and intracellular oedema. Hypoxic damage leading to intracellular oedema can lead to cellular damage and stimulation of the inflammatory response, which will stimulate the release of mediators. In addition, oedema can lead to hypoxia and stimulation of the inflammatory response.
Modified from Edwards 2003c.
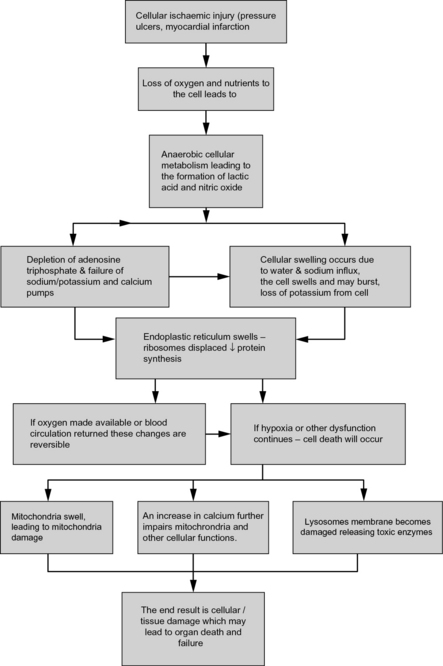
The interrupted supply of oxygenated blood to cells can result in cellular changes, which in turn can stimulate the inflammatory response (IR) (see later). The interrupted supply of oxygenated blood to cells results in anaerobic metabolism and cellular membrane disruption (Fig. 4.1).
Tissue injury: the formation of oedema
Oedema is an abnormal collection of fluid in tissues, which can either collect in interstitial or intracellular spaces (Edwards 2003c). Oedema is a problem of fluid distribution and does not necessarily indicate fluid excess. The causes of oedema are varied (Table 4.1) and include hypoxia (leads to intracellular oedema) (see previous) and the inflammatory response (leads to interstitial oedema) (see later).
1. Stimulation of the inflammatory immune response (see later).
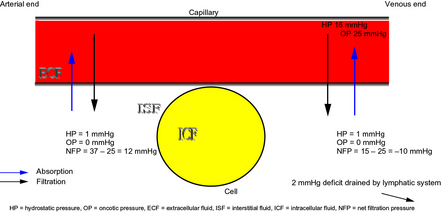
2. Changes in capillary dynamics (Fig. 4.2) due to increase or decrease in hydrostatic pressure is seen in conditions when the hydrostatic pressure is high (Table 4.2). Decreases in plasma oncotic pressure occurs in a number of conditions leading to poor healing and tissue viability may be affected (Table 4.3).
Table 4.2 The conditions that lead to changes in hydrostatic pressure and oedema formation
| Condition | Principles | Progression |
|---|---|---|
| Liver failure | In liver failure there is a general increase in pressure in the portal venous system and raised pressure in the portal vessels. | This may eventually lead to the formation of an ascites. |
| Heart failure | In heart failure the pressure can rise in either the systemic veins or the pulmonary veins, depending on which side of the heart is affected. Failure of the left ventricle causes pressure to rise in the pulmonary veins and can lead to oedema formation in the lungs as pulmonary oedema. | In right sided heart failure (complete heart failure) there is an increase in HP in the vena cava and other systemic veins. This tends to cause oedema in systemic tissues and oedema will form in the parts of the body that hang down, such as the wrists, ankles and sacrum. |
| Renal failure | Certain forms of damage to the kidneys interfere with their ability to eliminate excess water and solutes into the urine, which results in the accumulation of excess fluid in the body. | As a consequence, blood volume increases and blood pressure rises throughout the cardiovascular system. The increase in pressure raises capillary HP, which will increase filtration and reduce absorption processes and lead to the formation of oedema. |
Table 4.3 The conditions that lead to changes in colloid osmotic pressure and oedema formation
| Condition | Principles | Progression |
|---|---|---|
| Renal disease | Damage to the kidneys can cause increased elimination of plasma proteins in the urine (nephritic syndrome) | This loss of protein triggers a reduction in capillary absorption because of the drop in colloid osmotic pressure |
| Malnutrition | Starvation will reduce the amount of protein available to form plasma proteins. During malnutrition insufficient amounts of proteins are digested through the gastrointestinal tract. | If the malnourished state is allowed to continue, the proteins stored in the body are broken down and used as a source of energy by the liver to maintain cellular and organ function. This leads to a reduction in plasma proteins which are unable to produce effective colloid osmotic pressure. |
Tissue repair: activation of the inflammatory response
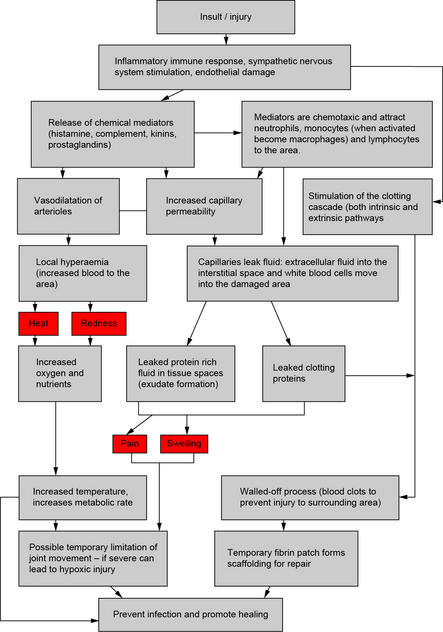
Cellular damage e.g. leg ulcers, surgical procedures, and trauma (Table 4.1) causes stimulation of the IR that ends with repair to damaged cells and tissues (Edwards 2006). Activation of the IR is part of the innate immune system, and represents a major physiological event in the body (Fig. 4.3). Following the damage tissues release mediators, the most important are:
The effect of treatments on the physiological processes
 The nurses’ role is to administer the prescribed fluid regimes for the immediate restoration of an effective circulating blood volume. This may require the use of blood, blood products, a balanced salt and/or water solution, colloid solution or a combination of all solutions.
The nurses’ role is to administer the prescribed fluid regimes for the immediate restoration of an effective circulating blood volume. This may require the use of blood, blood products, a balanced salt and/or water solution, colloid solution or a combination of all solutions.
 Following injury a balance between oxygen supply and tissue demands is fundamental. Oxygen supply and demand is maintained in equilibrium as long as supplies of oxygen are available and carbon dioxide is eliminated through ventilation, perfusion, diffusion and cell metabolism. Any alteration of any part of these processes cause impaired gas exchange. The nurse, therefore, is responsible for administrating humidified oxygen, the continuous frequent monitoring of respiratory rate, depth and pattern of breathing and any signs of change.
Following injury a balance between oxygen supply and tissue demands is fundamental. Oxygen supply and demand is maintained in equilibrium as long as supplies of oxygen are available and carbon dioxide is eliminated through ventilation, perfusion, diffusion and cell metabolism. Any alteration of any part of these processes cause impaired gas exchange. The nurse, therefore, is responsible for administrating humidified oxygen, the continuous frequent monitoring of respiratory rate, depth and pattern of breathing and any signs of change.
 The use of all energy sources following an insult/injury causes an exhaustion of energy stores, deprives cells and tissues of nutrients to support organ function. The loss of energy stores especially protein depletion will contribute to morbidity and mortality of patients following an insult. It is therefore imperative to initiate feeding early in children.
The use of all energy sources following an insult/injury causes an exhaustion of energy stores, deprives cells and tissues of nutrients to support organ function. The loss of energy stores especially protein depletion will contribute to morbidity and mortality of patients following an insult. It is therefore imperative to initiate feeding early in children.
Neurological
Epilepsy
Types of seizures
 Generalized – where both sides of brain are involved:
Generalized – where both sides of brain are involved:
 Partial (focal) – where seizure starts in one part of the brain:
Partial (focal) – where seizure starts in one part of the brain:
Investigations
Care and management
 Time the length of the convulsion.
Time the length of the convulsion.
 Stay with the child and lie them on their side.
Stay with the child and lie them on their side.
 Cushion their head with something soft if they have collapsed to the ground.
Cushion their head with something soft if they have collapsed to the ground.
 Do not put anything in child’s mouth or try to restrain the child.
Do not put anything in child’s mouth or try to restrain the child.
 Remove any objects that could cause injury.
Remove any objects that could cause injury.
 When the seizure does not subside, this is known as status epilepticus (please read details in Section 1).
When the seizure does not subside, this is known as status epilepticus (please read details in Section 1).
 Anticonvulsant drugs are used for long-term treatment. Examples are: sodium valproate, carbamazapine, clonazepam, phenobarbital and phenytoin.
Anticonvulsant drugs are used for long-term treatment. Examples are: sodium valproate, carbamazapine, clonazepam, phenobarbital and phenytoin.
 The type of medication will depend on the type of seizure.
The type of medication will depend on the type of seizure.
 Children with epilepsy are usually controlled through the use of one anticonvulsant drug.
Children with epilepsy are usually controlled through the use of one anticonvulsant drug.
Long-term care of epilepsy
 Child should wear a medical alert bracelet or carry a card that identifies their condition.
Child should wear a medical alert bracelet or carry a card that identifies their condition.
 Medication must be taken as prescribed.
Medication must be taken as prescribed.
 Blood levels need to be checked periodically.
Blood levels need to be checked periodically.
 Anticonvulsant medication can cause drowsiness and interfere with other medication so it is important that health professionals know all medications the child is taking.
Anticonvulsant medication can cause drowsiness and interfere with other medication so it is important that health professionals know all medications the child is taking.
 Seizures can be controlled by medication, surgery or a combination of both.
Seizures can be controlled by medication, surgery or a combination of both.
 Surgery may block the area where seizure begins, remove brain tissue or use vagal nerve stimulation (VNS).
Surgery may block the area where seizure begins, remove brain tissue or use vagal nerve stimulation (VNS).
 A ketogenic diet high in fat, low in carbohydrates and low in calories can reduce the number and severity of seizures for some children.
A ketogenic diet high in fat, low in carbohydrates and low in calories can reduce the number and severity of seizures for some children.
 Avoid or limit known triggers, e.g. flickering lights, lack of sleep, fatigue, noise, exercise, stress and non-compliance with medication.
Avoid or limit known triggers, e.g. flickering lights, lack of sleep, fatigue, noise, exercise, stress and non-compliance with medication.
 Some children can outgrow their seizures by their mid to late teens.
Some children can outgrow their seizures by their mid to late teens.
 Children are not allowed to swim alone.
Children are not allowed to swim alone.
 Children must always wear helmets when cycling, roller blades, or using scooters.
Children must always wear helmets when cycling, roller blades, or using scooters.
 Young girls may experience seizures prior to menstrual periods, thus medication may need to be adjusted when child reaches puberty.
Young girls may experience seizures prior to menstrual periods, thus medication may need to be adjusted when child reaches puberty.
 Alcohol can affect epilepsy, thus children need to be strongly advised against using alcohol or recreational drugs.
Alcohol can affect epilepsy, thus children need to be strongly advised against using alcohol or recreational drugs.
 Young people (18 years) are not allowed to drive until they have been seizure free for 3 months or more depending on the countries driving regulations.
Young people (18 years) are not allowed to drive until they have been seizure free for 3 months or more depending on the countries driving regulations.
High temperatures
For in an emergency see Section 1. There are four general states of increased body temperature (Edwards 1998b, 2003b):
 Pyrexia (fever) – involves a condition whereby the thermoregulatory mechanisms remain intact, but the body temperature is maintained at a high level. It generally has an infective aetiology, but there are other non-infectious causes of a hyperpyrexia. These include haemolysis (seen in reactions to blood transfusions) and thyrotoxicosis.
Pyrexia (fever) – involves a condition whereby the thermoregulatory mechanisms remain intact, but the body temperature is maintained at a high level. It generally has an infective aetiology, but there are other non-infectious causes of a hyperpyrexia. These include haemolysis (seen in reactions to blood transfusions) and thyrotoxicosis.
 Hyperpyrexia – the hypothalamus set point temperature is generally very high e.g. above 40°C, generally observed in conditions such as septicaemia and meningitis. A temperature between 41°C and 43°C produces nerve damage, coagulation, convulsions and death.
Hyperpyrexia – the hypothalamus set point temperature is generally very high e.g. above 40°C, generally observed in conditions such as septicaemia and meningitis. A temperature between 41°C and 43°C produces nerve damage, coagulation, convulsions and death.
 Hyperthermia – occurs when there is hypothalamic injury, due to neoplasms, surgery, central nervous system problems, and when overheating overwhelms the heat loss mechanisms – causes cerebral metabolism to increase and the brain has great difficulty keeping up with the increase in carbon dioxide production, does not respond to antipyretic therapy.
Hyperthermia – occurs when there is hypothalamic injury, due to neoplasms, surgery, central nervous system problems, and when overheating overwhelms the heat loss mechanisms – causes cerebral metabolism to increase and the brain has great difficulty keeping up with the increase in carbon dioxide production, does not respond to antipyretic therapy.
 Malignant hyperthermia – caused by certain drugs commonly used in patients, e.g. diuretics, antiseizure therapy, analgesics, some common anaesthetics, anti-arrhythmics and antibiotics. A malignant hyperthermia also presents in five other conditions:
Malignant hyperthermia – caused by certain drugs commonly used in patients, e.g. diuretics, antiseizure therapy, analgesics, some common anaesthetics, anti-arrhythmics and antibiotics. A malignant hyperthermia also presents in five other conditions:
 A compensatory response by the hypothalamus, which will produce heat-generating activities like chills and shivering.
A compensatory response by the hypothalamus, which will produce heat-generating activities like chills and shivering.
 Information sent to the hypothalamus that the body temperature is decreasing.
Information sent to the hypothalamus that the body temperature is decreasing.
 Compromising an unstable patient by depleting their metabolic reserve and can create a new temperature spike, which is as high or higher than the original one, and may even increase the patient’s temperature.
Compromising an unstable patient by depleting their metabolic reserve and can create a new temperature spike, which is as high or higher than the original one, and may even increase the patient’s temperature.
 The patient feeling weak, especially during the early stages when the temperature is still rising.
The patient feeling weak, especially during the early stages when the temperature is still rising.
Hypothermia
 Accidental hypothermia is a temperature below 35°C and is a result of sudden immersion in cold water or prolonged exposure to cold environments. Healthy subjects who experience hypothermia often survive profound hypothermia with medical support.
Accidental hypothermia is a temperature below 35°C and is a result of sudden immersion in cold water or prolonged exposure to cold environments. Healthy subjects who experience hypothermia often survive profound hypothermia with medical support.
 Therapeutic hypothermia is used to slow metabolism and preserve ischaemic tissue during surgery. It can also occur through exposure of body cavities to the relatively cool operating room environment, irrigation of body cavities with room temperature solutions, infusion of room temperature intravenous solutions, and inhalation of unwarmed anaesthetic agents. These types of therapeutic hypothermia can extend into the postoperative period.
Therapeutic hypothermia is used to slow metabolism and preserve ischaemic tissue during surgery. It can also occur through exposure of body cavities to the relatively cool operating room environment, irrigation of body cavities with room temperature solutions, infusion of room temperature intravenous solutions, and inhalation of unwarmed anaesthetic agents. These types of therapeutic hypothermia can extend into the postoperative period.
 passive external rewarming (removal of wet clothes, blankets, warm room)
passive external rewarming (removal of wet clothes, blankets, warm room)
 active external rewarming (radiant lights, convection air blankets)
active external rewarming (radiant lights, convection air blankets)
 active internal rewarming (warmed gases to respiratory tract, warmed intravenous fluids).
active internal rewarming (warmed gases to respiratory tract, warmed intravenous fluids).
Endocrine disorders
Diabetes insipidus
Types of diabetes insipidus
 Central or neurogenic diabetes insipidus – lack of antidiuretic hormone (ADH) being released into the circulation in response to an osmotic stimulus, e.g. osmoreceptors.
Central or neurogenic diabetes insipidus – lack of antidiuretic hormone (ADH) being released into the circulation in response to an osmotic stimulus, e.g. osmoreceptors.
 Transient usually incomplete central diabetes insipidus is noticed frequently in patients with head injury.
Transient usually incomplete central diabetes insipidus is noticed frequently in patients with head injury.
 Dipsogenic or psychogenic diabetes insipidus – precipitated by excessive intake of water very rare.
Dipsogenic or psychogenic diabetes insipidus – precipitated by excessive intake of water very rare.
 Nephrogenic diabetes insipidus – deficient action of ADH
Nephrogenic diabetes insipidus – deficient action of ADH
 Pregnancy-related diabetes insipidus is also known to occur.
Pregnancy-related diabetes insipidus is also known to occur.
Clinical presentation
 Thirst – generally the desire for cold drinks
Thirst – generally the desire for cold drinks
 Inability to replace water may result in signs of hypovolaemia
Inability to replace water may result in signs of hypovolaemia
 Low urine osmolality – SG 1.001– 1.005
Low urine osmolality – SG 1.001– 1.005
 High plasma osmolality due to dehydration
High plasma osmolality due to dehydration
 The essential feature is that urine osmolality is inappropriately low compared to plasma osmolality.
The essential feature is that urine osmolality is inappropriately low compared to plasma osmolality.
 Urine volumes over 4–6 l/day or 3 ml/kg over 2 consecutive hours (in neurosurgical patients may point toward diabetes insipidus).
Urine volumes over 4–6 l/day or 3 ml/kg over 2 consecutive hours (in neurosurgical patients may point toward diabetes insipidus).
Investigations
 Random plasma and urine osmolality.
Random plasma and urine osmolality.
 Plasma and urine osmolality relationships.
Plasma and urine osmolality relationships.
 Blood chemistry – blood glucose, 24 hour urine osmolality an electrolytes, blood and urine electrolytes, urea and creatinine.
Blood chemistry – blood glucose, 24 hour urine osmolality an electrolytes, blood and urine electrolytes, urea and creatinine.
 ADH test – if tests above are positive then ADH (usually as DDAVP nasally) is given.
ADH test – if tests above are positive then ADH (usually as DDAVP nasally) is given.
 Hypertonic saline – used to evaluate osmoreceptor mechanism.
Hypertonic saline – used to evaluate osmoreceptor mechanism.
Diabetes mellitus
The pancreas
A hyposecretion of glucagon leads to hypoglycaemia, hypersecretion leads to hyperglycaemia.
Type 1 diabetes mellitus
This used to be called insulin-dependent diabetes mellitus (IDDM).
 Dependent on insulin without it the patient would die.
Dependent on insulin without it the patient would die.
 Less than 25% of people with diabetes are insulin dependent.
Less than 25% of people with diabetes are insulin dependent.
 Thought to be an autoimmune disorder – beta cells in the pancreas are targeted by antibodies and eventually totally destroyed.
Thought to be an autoimmune disorder – beta cells in the pancreas are targeted by antibodies and eventually totally destroyed.
 Some individuals have a genetic predisposition – trigger factor is needed; this is generally a virus.
Some individuals have a genetic predisposition – trigger factor is needed; this is generally a virus.
 Highest incidence around 11–12 years but can occur at any age, uncommon over the age of 40 years.
Highest incidence around 11–12 years but can occur at any age, uncommon over the age of 40 years.
Type 2 diabetes mellitus
Type 2 diabetes used to be called non-insulin dependent diabetes mellitus (NIDDM).
 There is either insufficient production of insulin or an inability of the body to use the insulin adequately (insulin resistance).
There is either insufficient production of insulin or an inability of the body to use the insulin adequately (insulin resistance).
 Patients not dependent on insulin may receive some insulin to help control their diabetes, but can live without it.
Patients not dependent on insulin may receive some insulin to help control their diabetes, but can live without it.
 Different from type 1 and does not happen in the young, may have the disorder for years and not know it.
Different from type 1 and does not happen in the young, may have the disorder for years and not know it.
 Symptoms develop much more insidiously, incidence increases with age and as people are living longer, so the disease is getting more common.
Symptoms develop much more insidiously, incidence increases with age and as people are living longer, so the disease is getting more common.
 Disorder is linked to obesity, and can run in families.
Disorder is linked to obesity, and can run in families.
 Can be controlled by diet alone or by medication such as oral hypoglycaemic agents, to bring down blood glucose.
Can be controlled by diet alone or by medication such as oral hypoglycaemic agents, to bring down blood glucose.
Respiratory
Asthma
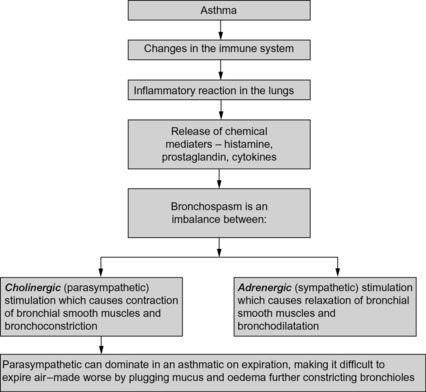
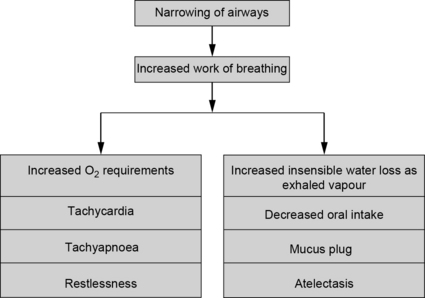
The most common diagnosis for children admitted to hospital is asthma and its related disorders. In the last 20 years, hospitals have dealt with a dramatic increase in both asthma-related admissions and readmissions in the paediatric population. Asthma admission rates are more frequent amongst girls, and the likelihood of readmission is higher amongst children under five years of age. Asthma is an inflammatory condition of the airways mediated by a wide range of stimuli usually the immunoglobulin IgE, the release of chemical mediators, leading to bronchospasm (Fig. 4.4), which is due to an imbalance between:
These actions contributes to plugging mucus and oedema (Fig. 4.5).
Acid–base changes occur
Pulmonary embolism (PE)
 90% of PE is the consequence of clots that are initially in the leg veins and the pelvis.
90% of PE is the consequence of clots that are initially in the leg veins and the pelvis.
 Half the people diagnosed with pulmonary embolism die within 2 hours of the diagnosis.
Half the people diagnosed with pulmonary embolism die within 2 hours of the diagnosis.
 PE is responsible for 10% of hospital death and 80% of the time PE go undetected.
PE is responsible for 10% of hospital death and 80% of the time PE go undetected.
 PE causes hypoxia, vasoconstriction, pulmonary oedema or decrease in surfactant.
PE causes hypoxia, vasoconstriction, pulmonary oedema or decrease in surfactant.
Diagnosis of PE
 Bloods are taken to examine leukocyte count and sedimentation rate, which is usually elevated in cases of infarction.
Bloods are taken to examine leukocyte count and sedimentation rate, which is usually elevated in cases of infarction.
 Impairment in gas exchange that is to say partial pressure of oxygen was low, partial pressure of carbon dioxide was normal and the pH was normal.
Impairment in gas exchange that is to say partial pressure of oxygen was low, partial pressure of carbon dioxide was normal and the pH was normal.
 Use of a VQ scan but results can be sometimes inconclusive. Angiography and echocardiography could then be used but they are not easily available in most hospitals.
Use of a VQ scan but results can be sometimes inconclusive. Angiography and echocardiography could then be used but they are not easily available in most hospitals.
 PE should be suspected in patients who collapse suddenly 1–2 weeks following surgery.
PE should be suspected in patients who collapse suddenly 1–2 weeks following surgery.
 If large PE is a medical emergency – leading to death
If large PE is a medical emergency – leading to death
 Clinical features depends on size of embolus:
Clinical features depends on size of embolus:
Treatment of PE
The aim of the therapy is to prevent further thrombus formation and embolization.
 The administration of oxygen is required to relieve shortness of breath and to supply oxygen to the affected areas of the lungs.
The administration of oxygen is required to relieve shortness of breath and to supply oxygen to the affected areas of the lungs.
 Morphine 10 mg may be given to relieve chest pain.
Morphine 10 mg may be given to relieve chest pain.
 A bolus of heparin is used as a fast-acting drug and then proceed with warfarin.
A bolus of heparin is used as a fast-acting drug and then proceed with warfarin.
Care of a patient with a PE
 Involves supportive measures and prevention of further emboli formation.
Involves supportive measures and prevention of further emboli formation.
 The primary excessive usage of heparin is bleeding of the gums when brushing teeth, excessive or easy skin brushing and unexplained nose bleeds.
The primary excessive usage of heparin is bleeding of the gums when brushing teeth, excessive or easy skin brushing and unexplained nose bleeds.
 The vital signs the nurse has to look for include when a child appears to be in shock or having difficulty in breathing and pain.
The vital signs the nurse has to look for include when a child appears to be in shock or having difficulty in breathing and pain.