CHAPTER 39. Sudden Death During Restraint
Excited Delirium Syndrome
Theresa G. Di Maio and Vincent J.M. Di Maio
The sudden, unexplained death of an individual in custody presents a difficult challenge to the medicolegal community, especially if the individual dies during or immediately after a violent struggle, and a complete autopsy fails to reveal either an anatomical cause of death or evidence of sufficient trauma to explain death. Typically the struggle ends with employment of physical restraint. Most such deaths occur in conjunction with the use of illegal stimulants such as cocaine or methamphetamine or involve individuals with a history of intrinsic mental disease, usually schizophrenia. Similar deaths occur in emergency rooms and in mental health facilities where the individuals employing the restraint are medical personnel. A review of these cases reveals that the reason either police or medical personnel intervened was that the individuals in custody were in a state of excited delirium.
Delirium is characterized by an acute (minutes to hours), transient disturbance in consciousness and cognition. There is disorganized and inconsistent thought processes, disorientation, inability to distinguish reality from hallucinations, disturbances in speech, and disorientation to time and place. When the delirium involves combative or violent behavior, it is termed excited delirium (Di Maio & Di Maio, 2006). Most cases of delirium are due to natural disease and occur in the hospital setting. The cases we are interested in, however, are those that occur when police or medical personnel attempt to restrain an individual so as to protect the individual or the public from harm.
Deaths Associated with EDS
Excited delirium syndrome (EDS) involves the sudden death of an individual, during or following an episode of excited delirium in which an autopsy fails to reveal evidence of sufficient trauma or natural disease to explain the death. In virtually all such cases, the episode of excited delirium is terminated by a struggle with police or medical personnel and the use of physical restraint (Di Maio & Di Maio, 2006). The individual may go into cardiopulmonary arrest during or within minutes following cessation of the struggle. Attempts at resuscitation are usually unsuccessful. If a cardiac monitor is available at the time of the arrest, the rhythm noted is usually bradycardia, pulseless electrical activity (PET) or asystole. If resuscitation is “successful,” the individual is found to have suffered irreversible hypoxic encephalopathy and death usually occurs in a matter of days.
The concept of death as a result of “excited delirium” was introduced in 1849 by Dr. Luther Bell of the McLeon Asylum for the Insane in Somerville, Massachusetts (Bell, 1849). According to Bell, the patient was agitated and anxious, with increasing confusion that appeared suddenly. Any attempt to approach the patient resulted in a violent struggle regardless of the number who tried to restrain him or her. The physical and mental state of the patient continued to deteriorate over the course of weeks resulting in death. This entity became known as “Bell’s mania.” Deaths resulting from Bell’s mania continued to be reported in the medical literature until the early 1950s when they abruptly disappeared with the introduction of phenothiazines for treatment of mental illness (Cancro, 2000 and Lieberman et al., 2000). Although all of Bell’s patients had mental disease and their symptoms progressed over days to weeks before death, deaths seen today in association with excited delirium principally involve abusers of stimulants (e.g., cocaine or methamphetamine), with symptoms present for only hours. Deaths do still occur in patients suffering from mental illness, usually in individuals with schizophrenia and occasionally bipolar disease and usually outside medical facilities. In individuals with intrinsic mental disease, death usually occurs following the use of restraint because of an acute psychotic episode.
Mechanisms of death and use of restraint
The mechanism of death in emergency departments has been obscured by erroneous experiments and assumptions that appear superficially logical and correct but are wrong. Because such deaths almost always occur after restraint is either instituted or attempted, the cause of death has typically been attributed to “restraint/positional asphyxia,” even when there is neither testimonial nor physical evidence of this condition. Because of the circumstances surrounding deaths resulting from excited delirium, there are often charges of police or medical misconduct. In some cases, allegations of murder are made.
In 1988, Reay et al. conducted a series of experiments to determine the effects on peripheral oxygen saturation and heart rate when an individual is hog-tied and placed prone following exercise (Reay et al., 1988). They concluded that hog-tie restraint prolongs recovery from exercise as determined by changes in peripheral oxygen saturation and heart rate. In an article published in 1993 by O’Halloran and Lewman on the association of restraint and asphyxiation, hog-tying and death were codified in the concept of “restraint asphyxia” or “positional asphyxia” (O’Halloran & Lewman, 1993). Even with the elimination of hog-tying, however, the number of deaths due to EDS continued, if not increased. Almost immediately after the concept of positional/restraint asphyxia was offered, the concept was expanded such that whenever anyone is restrained and dies, positional or restraint asphyxia is said to be the cause of death whatever the position of the deceased, the method of restraint, or the presence of drugs.
In 1997, Chan et al. published a study on restraint asphyxia (Chan et al., 1997). They repeated the experiments of Reay et al. (1988) using a more systematic approach and more sophisticated technology. Pulmonary function testing (forced vital capacity; forced expiratory volume in one second and maximal voluntary ventilation) was performed on individuals in the sitting, supine, prone, and restraint position (hog-tying). The subjects were then subjected to two exercise periods and two rest periods. During the rest periods, determinations of arterial blood gas, pulse rate, oxygen saturation by CO-oximetry and pulse oximetry, and pulmonary function testing (PFT) were performed. Determinations at the rest periods were made with the subject alternatively in the sitting position and restraint position. Placing individuals in the restraint position after exercise resulted in restrictive pulmonary functioning as measured by PFT. However, the PFT changes, although statistically significant, were not clinically relevant. Based on arterial PO 2 and CO-oximetry, oxygenation of blood increased with exercise, what one would expect and in contrast to Reay et al.’s findings. Most important was the fact that there was no evidence of hypoxia in the restraint position after exercise with no evidence of hypercapnia either during exercise or in restraint. Chan et al. concluded that there was no evidence that body position, while in the “hog-tie” or “hobble” restraint position, in and of itself causes hypoventilation or asphyxiation.
In an attempt to counter Chan et al.’s work, some individuals now claim that the death is due to compromise in ventilation occurring when an officer/medical worker applies body weight to the upper torso of an individual in an attempt to restrain the individual or prevent further struggle. This is usually accomplished by lying across an individual’s back or applying pressure on the back with a knee or hands. Because of this allegation, Michalewicz et al. (2007) conducted a series of experiments. They investigated ventilatory and metabolic demands in healthy adults when placed in the prone maximal restraint position (PMRP) (e.g., hog-tie restraint). Maximal voluntary ventilation (MVV) was measured in seated subjects, in the PMRP, and when prone with 90.1 to 102.3 kg (198 to 225 lb) of weight on the back. Subjects were then placed in the PMRP and struggled vigorously for 60 seconds. The authors found no clinically important restriction of ventilatory reserve when subjects were placed in the PMRP or when prone with up to 90.2 or 102.3 kg of weight on their back. Likewise, when subjects were maximally struggling for 60 seconds while in the PMRP, there were no clinically important limitations of metabolic or ventilatory functions. They stated: “Based on these findings, as well as previously published studies, we suggest that factors other than ventilatory failure associated with the restraining process may be responsible for the sudden unexpected deaths of restrained individuals” (Michalewicz, et al., 2007, p. 174).
Physiological effects
The question then arises as to what is actually causing these deaths. It is the conclusion of the authors that sudden death from excited delirium is due to the effects of the normal physiological changes seen in a struggle, combined with, depending on the case, the use of illicit drugs, cardiotoxic medications, and natural disease. In some individuals, polymorphism of cardiac adrenoreceptors with resultant exacerbation of the normal responses to violent physical activity may also play a role. In fatal cases of excited delirium, death usually occurs immediately after the individual is restrained and struggling ceases. This poststruggle period corresponds to the time of “postexercise peril” defined by Dimsdale et al. (1984), a time where an individual is susceptible to developing a fatal cardiac arrhythmia. An understanding of the physiological changes that lead to postexercise peril is important in understanding EDS. These changes, resulting in cardiac dysfunction and arrest, are due to the physiological effects of the catecholamines, epinephrine, and norepinephrine, as well as potassium, on the heart.
Dimsdale et al. (1984) found that in the three minutes immediately following cessation of strenuous exercise, epinephrine and norepinephrine continue to rise with norepinephrine at more than 10-fold baseline levels. Norepinephrine’s action on the heart is stimulation of alpha-1 and beta-1 receptors (McCance, 1994). Stimulation of beta-1 receptors increases heart rate, contractility, and velocity of conduction. Alpha-1 receptors are found in the coronary arteries. Norepinephrine interacting with alpha-1 receptors causes vasoconstriction, thus decreasing the amount of oxygenated blood being supplied to the myocardium at a time when an increased amount is needed because of greater demand being put on the heart resulting from the stimulation of the beta-1 receptors.
Excessive levels of catecholamines, especially norepinephrine, can be cardiotoxic, resulting in catecholamine (norepinephrine) cardiomyopathy with impairment of myocardial contractility (Powers et al., 1994). Cardiac injury from excessive norepinephrine may be permanent. The lesions seen in catecholamine cardiomyopathy are myofibrillar degeneration, leukocyte infiltration, and focal necrosis. The pathogenesis of catecholamine-induced cardiomyopathy is disruption of myocardial calcium transport with resultant high levels of intracellular calcium. This results in a decreased rate of ventricular relaxation and an increased rate of diastolic tension, with resultant left ventricular dysfunction. Both diastolic and systolic functions are acutely impaired. Systolic function improves within 48 hours, whereas diastolic function remains depressed.
The effects of catecholamines and their role in sudden lethal cardiac arrhythmias were further expanded on by Young et al. (1992). They investigated not only the relationship between stress and catecholamine levels but potassium levels as well. Like Dimsdale et al., 1984 and Young et al., 1992 found that the highest levels of plasma catecholamines occurred during the three minutes postexercise. In addition, they found that during strenuous exercise, potassium increases dramatically. Postexercise, while norepinephrine continues to rise, potassium levels fell at a maximum rate for one to two minutes to hypokalemic or near-hypokalemic levels.
Blood potassium concentrations have a narrow range of safety. Fatal cardiac arrhythmias are associated with both hyperkalemia and hypokalemia. If sudden death occurs with increased levels of potassium, the question then arises as to why a fatal arrhythmia does not occur during the rising phase of potassium during exercise rather than postexercise. Paterson et al. found that exercise-induced increases in circulating catecholamines have a cardioprotective effect to the rapidly rising potassium levels (Paterson et al., 1993). This cardioprotective effect is not known to occur for falling potassium levels.
Thus, changes in catecholamine and potassium levels, independent of each other, are potentially lethal. Poststruggle, however, the lethal potential of these changes converge, increasing the possibility of sudden cardiac death. The low incidence of cardiac death among the exercising population, or even in individuals in excited delirium, indicate that in most instances changes in catecholamine and potassium levels poststruggle, in and of themselves, rarely cause fatal cardiac arrhythmias. For death to occur in the postexercise period, there must be either the presence of medications or drugs that potentiate the action of the catecholamines; cardiotoxic medications, including typical and atypical antipsychotic drugs (Ray, 2009); mental disease such as schizophrenia, which may be associated with elevated levels of catecholamines (Yamamoto & Hornykiewicz, 2004); or polymorphism of the alpha and beta receptors that result in abnormally high levels of norepinephrine (Small et al., 2002). These factors produce a cascade of biochemical actions that set a lethal course resulting in sudden cardiac death (Fig. 39-1).
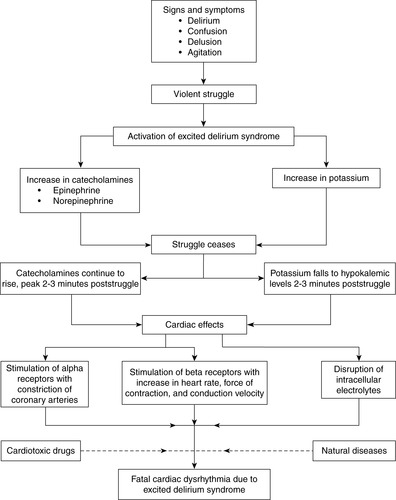 |
| Fig. 39-1 |
Taser Use Wrongly Linked to EDS Deaths
In a number of deaths resulting from excited delirium, a Taser has been used. In some cases, the cause of death has been attributed to the Taser. Tasers are handheld devices that fire two fishhook-like barbed darts attached to wires, simultaneously, up to a distance of 21 feet (Kroll & Tchou, 2007). The darts are propelled by a cartridge of compressed nitrogen. The wires are copper-clad steel wires with an insulated coating. At the end of each wire is a barb similar to a fishhook. The darts are designed to penetrate skin or lodge in clothing. On lodging in an individual or the individual’s clothing, a circuit is achieved and the Taser provides a series of electrical pulses for five seconds. When the dart strikes bare skin, it penetrates until the full flange on the dart stops it. Penetration of skin is not necessary because the electric pulse it delivers can penetrate up to 2 inches of clothing. A high-voltage (50,000 volt), low-amperage current is delivered down the wires to the target. Each time the trigger is pulled, a five-second pulse is delivered. The Taser is designed to produce electromuscular disruption (EMD) (i.e., muscular contractions) via externally applied electric fields, with uncontrollable contraction of the muscles and immediate collapse. The shocks can be repeated. The Taser records the exact number of seconds pulses are delivered and the time delivered.
One pull of the trigger generates five seconds of pulses. There are approximately 19 pulses per second. Each pulse is 2.1 milliamps and 0.36 Joules per pulse. For comparison, a bathroom ground fault circuit interrupter trips with 5 milliamps of current; household electrocutions require 75 to 100 milliamps.
There is no evidence that use of a Taser causes death. A Taser can be employed two ways. The most common way is as an EMD that causes neuromuscular incapacitation or strong muscle contractions through the involuntary stimulation of nerves. In the drive-stun mode, it is a pain compliance device. The second way is the drive-stun mode which does not incapacitate a subject but may assist in taking a subject into custody because of the induced pain. In neither mode does it interfere with respiration, as human experimentation has demonstrated. It has been estimated that approximately 750,000 law enforcement individuals have been voluntarily tasered with no deaths or fatal arrhythmias. There is no evidence that multiple use of the Taser in the EMD mode causes death.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


