Learning outcomes
By the end of this section, you should know how to:
▪ prepare the patient for this nursing practice
▪ collect and prepare the equipment
▪ carry out stoma care for the patient
▪ help patients to accept and care for their stoma themselves, both at home and in an institutional setting.
Background knowledge required
Revision of the anatomy and physiology of the digestive system, with special reference to the small and large intestines
Review of local policy regarding the role of the stoma care nurse and the literature available for patient education in an institutional and a community setting
Knowledge of the information and level of counselling given to the patient before the operation to create a stoma.
Indications and rationale for stoma care
A stoma is an artificial opening from the small or large intestine or bladder onto the surface of the abdomen through which the bowel contents or urine is diverted for excretion (Fig. 39.1). The stoma is formed after surgical intervention for the treatment of intestinal or bladder disease. Different names are used according to the site of the stoma.
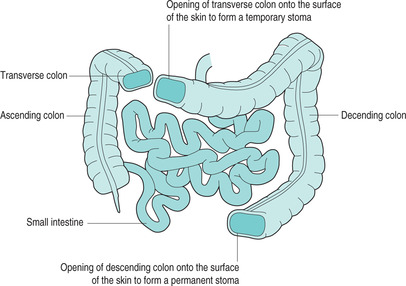 |
| FIGURE 39.1Sites that may be chosen for colostomy |
Stoma care involves cleansing the stoma and surrounding skin, and providing a suitable appliance for the safe collection and disposal of excreta. Nurses either perform this on the patient’s behalf or educate and support patients until they or a carer are able to competently care for the stoma.
A colostomy is an opening from the colon, usually the transverse or descending colon, and may be required:
▪ for patients who have malignant disease of the rectum or colon
▪ for patients who have diverticular disease of the colon
▪ for patients who have inflammatory disease of the intestine, e.g. Crohn’s disease or ulcerative colitis
▪ for patients who have suffered trauma to the abdomen or rectum
▪ for patients who suffer faecal incontinence.
An ileostomy is an opening from the ileum and may be formed for the same reasons as a colostomy, although it is more often seen in patients who have inflammatory disease of the intestine, for example Crohn’s disease or ulcerative colitis. In some cases, a temporary stoma may be formed so that once the disease has resolved, the stoma may be closed and the intestine anastomosed to function as before.
A urostomy is an opening from the bladder or ureter into a segment of the ileum, this being used as a channel for the urine to be diverted through an abdominal stoma. This is also known as an ileal conduit, and it may be required for the treatment of malignant disease of the bladder or in the management of the neuropathic bladder or urinary incontinence (Black 2000).
A stoma may be temporary or permanent. A temporary stoma is often created to divert faeces away from an operation site (anastomosis) to allow healing to occur. The stoma is then reversed by the surgeon with minimal or no loss of intestinal function. A permanent stoma implies that the bowel cannot be reconnected (Porrett & McGrath 2005).
 Equipment
Equipment1. Trolley or tray
2. Bowl of warm water (or warm water in sink if patient mobile to toilet)
3. Soft wipes
4. Suitable appliance (stoma pouch)
5. Scissors
6. Measuring guide
7. Measuring jug (if appropriate)
8. Gloves (non-sterile) and apron
9. Deodorant as required
10. Receptacle for soiled disposable items.
Stoma appliances
There is a wide range of appliances available, and, with the guidance of a stoma care nurse, the patient will choose the one most suitable for his or her needs. Stoma pouches may have pre-cut apertures or may have to be cut to fit individually. They may be closed pouches or open ended to allow emptying (Fig. 39.2).
 |
| FIGURE 39.2Examples of disposable stoma bags A Closed pouch B Open lower end to permit emptying of the contents |
Postoperatively, the surgeon will place a clear plastic appliance over the stoma. This allows the observation of the stoma and its function. It may be 2–5 days before the appliance needs to be changed for the first time.
 Guidelines and rationale for this nursing practice
Guidelines and rationale for this nursing practice▪ explain the nursing practice to the patient to gain consent and co-operation, and encourage participation in care
▪ ensure the patient’s privacy to maintain self-esteem and prevent embarrassment (Royal College of Nursing 2002)
▪ wash hands to reduce the risk of cross-infection (Nicol et al 2001)
▪ collect and prepare the equipment so that everything is ready
▪ help the patient into a comfortable position to reduce any distress and to help him or her see the area of the stoma
▪ help to adjust the clothing to expose the patient’s abdomen in the area of the stoma for easy access and so that the patient can observe the practice
▪ put on gloves and apron to prevent any contamination from body fluids
▪ place soft wipes appropriately to protect the surrounding area from spills or leakage
▪ observe the patient throughout this activity to monitor any adverse effects
▪ empty the appliance and, if required, measure its contents for an evaluation of the elimination fluid balance
▪ gently remove the appliance to expose the stoma area
▪ encourage the patient to look at the stoma and explain what you are doing so that he or she gradually accepts the change of body image and to encourage early independence
▪ observe the colour and condition of the stoma and the surrounding skin to evaluate the wound healing process
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
