Learning outcomes
By the end of this section, you should know how to:
▪ prepare the patient for this nursing practice
▪ collect the equipment
▪ carry out skin care.
Background knowledge required
Revision of the anatomy and physiology of the skin
Revision of the predisposing factors for the development of a pressure ulcer
The health authority policy regarding risk assessment, pressure ulcer classification, care implementation and criteria for the use of aids to prevent pressure ulcers should be reviewed
Indications and rationale for skin care
This care involves the maintenance of a patient’s skin viability by ensuring skin cleanliness, relieving skin capillary pressure, ensuring adequate nutritional status and monitoring potential problems. Skin care is indicated for every patient, but specific circumstances increase the need for care when:
▪ the patient is incontinent
▪ the patient’s mobility is temporarily or permanently impaired, e.g. a bedfast, paralysed or unconscious patient
▪ the patient has a poor nutritional status
▪ the patient has impaired peripheral circulation.
 Equipment
Equipment1. Appropriate risk assessment scale, e.g. the Norton (Fig. 37.1), Waterlow (Fig. 37.2) or Braden (Bergstrom et al 1987) Scale
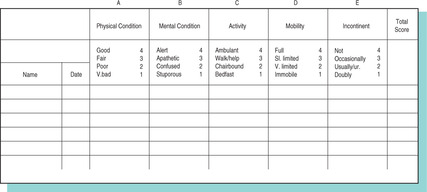 |
| FIGURE 37.1Norton ScaleFrom Roper et al 1985, with permission |
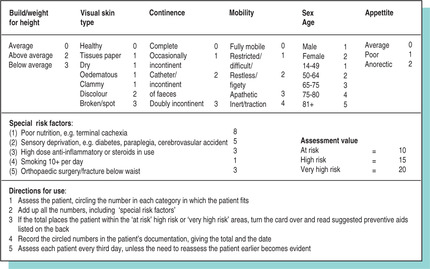 |
| FIGURE 37.2Waterlow Scale |
2. Pressure-relieving devices (Bale 2006).
 Guidelines and rationale for this nursing practice
Guidelines and rationale for this nursing practice▪ explain the nursing practice to the patient to gain consent and co-operation
▪ ensure the patient’s privacy to reduce anxiety
▪ wash the hands to reduce the risk of cross-infection (Jeanes 2005)
▪ observe the patient throughout this activity to note any signs of distress or discomfort
▪ assess the risk factor of the patient developing a pressure ulcer, utilising one of the assessment scales, such as the Norton (Fig. 37.1) or Waterlow (Fig. 37.2) Scale to permit preventive care to be implemented. This should be performed as part of the initial assessment process and at regular intervals throughout care when the patient’s condition alters (Waterlow 1992, Bale 2006)
▪ assess the patient using a nutritional risk assessment tool such as the Burton Score (Russell 2000) to assess the patient’s nutritional status as malnutrition increases the risk of skin breakdown
▪ identify individual patient problem areas, such as a patient with peripheral vascular disease whose affected limb may be at greater risk than the rest of his or her body as there will be increased risk of the development of a pressure ulcer (Royal College of Nursing 2001)
▪ when a risk factor is noted, institute preventive skin care (Royal College of Nursing 2001), which will reduce the risk of development of a pressure ulcer
▪ relieve the pressure exerted on the skin surface by regularly changing the patient’s body position (Lowthian 1987) and using pressure-relieving devices (Bale 2006) to prevent or reduce devitalisation of the healthy tissue
▪ support the patient’s body and limbs in natural positions to promote comfort and prevent damage, and maintain joint and muscle movement with passive and active exercises (seep. 135)
▪ a patient who is assessed as having a high risk factor will require frequent, for example 2 hourly, changes of position to relieve the pressure of the soft tissues against bone (Bale 2006). A turning chart may be used to record the time, position of the patient and signature of the nurse or carer
▪ reduce the pressure, friction and shearing forces on the skin by the use of any of the recommended aids available, such as static load distribution, posture changing or dynamic load distribution beds or mattresses (Lowthian 1995, Morison 2001), which reduce the factors contributing to pressure sore development
▪ cleanse the skin of an incontinent patient or a patient who is perspiring profusely as the number of micro-organisms will be greatly increased. Use soap with caution as the alkaline content tends to dry the skin and deplete it of its natural oils
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
