Skill 37
Isolation Precautions
In 2007 the Hospital Infection Control Practices Advisory Committee (HICPAC) of the Centers for Disease Control and Prevention (CDC) published revised guidelines for isolation precautions (Box 37-1). These recommendations were based on current epidemiological information regarding disease transmission in health care settings. Although primarily intended for care of patients in acute care, you can apply the recommendations to patients in subacute care or long-term care facilities. HICPAC recommends that hospitals modify the recommendations according to their needs and as dictated by federal, state, or local regulations (CDC, 2007b).
Standard Precautions are the primary strategies for prevention of infection transmission and apply to contact with blood, body fluids, nonintact skin, and mucous membranes and with equipment or surfaces contaminated with these potentially infectious materials. The strategy of respiratory hygiene/cough etiquette applies to any person with signs of respiratory tract infection, including cough, congestion, rhinorrhea, or increased production of respiratory secretions when entering a health care site. Education of health care staff, patients, and visitors to cover the mouth and nose with a tissue when coughing, dispose properly of used tissues, and perform hand hygiene is among the elements of respiratory hygiene.
The second tier (Table 37-1) includes precautions designed for care of patients who are known or suspected to be infected, or colonized, with microorganisms transmitted by the contact, droplet, or airborne route (Brisko, 2011; CDC, 2007a) or by contact with contaminated surfaces. The three types of transmission-based precautions—airborne, droplet, and contact—may be combined for diseases that have multiple routes of transmission (e.g., chickenpox). They are used either singly or in combination when Standard Precautions are implemented.
TABLE 37-1
CDC Isolation Guidelines: Transmission-Based Precautions (Tier 2) for Use With Specific Types of Patients

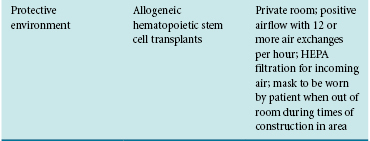
* HEPA, High-efficiency particulate air; MRSA, methicillin-resistant Staphylococcus aureus; VRE, vancomycin-resistant enterococcus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


