CHAPTER 35. Renal and Genitourinary Emergencies
Cynthia S Baxter
Genitourinary (GU) problems are a common complaint in the emergency department (ED). According to the National Institutes of Health (NIH), urinary tract infections (UTIs) are the second most common infection in the body and affect women more often than men. Up to one in five females will have at least one UTI in their lifetime; many will experience multiple UTIs. 5 Kidney stones are one of the most common disorders of the urinary tract. In 2000, kidney stones resulted in 2.7 million visits to health care providers and more than 600,000 visits to EDs. 10 Approximately 18.9 million new cases of sexually transmitted infections (STIs) occured in the United States in 2000. According to an incidence and prevalence study, 48% were among persons age 15 to 24 years, and three STIs (human papilloma virus, trichomoniasis, and Chlamydia) accounted for 88% of all new cases among this age-group. 12 Incidence of end-stage renal disease (ESRD) is rising in all industrialized nations, although the cause of this increase is not clear. ESRD affects African Americans three times more often than whites and is most prevalent in those with diabetes or hypertension, occurring six times more often in those with hypertension. In people 65 years of age or older, incidence of renal failure increases sixfold; however, 66% of all diabetes-induced renal failure occurs before age 64. Males account for 65% of the ESRD population. 7 Acute tubular necrosis, the most common type of acute renal failure (ARF), accounts for 5% of all hospital admissions. Patients with compromised renal function often arrive at the ED with life-threatening fluid and electrolyte imbalances.
ANATOMY AND PHYSIOLOGY
The GU tract consists of the kidneys, ureters, urinary bladder, urethra, and external genitalia. Urine is produced by the kidneys as a way to regulate fluid volume and electrolyte balance. Ureters transport urine to the bladder for temporary storage. The urine is drained from the bladder to the outside by the urethra. External structures of the male GU system have reproductive functions.
The kidneys are located on the posterior abdominal wall behind the peritoneum on either side of the vertebral column inside the rib cage. The medial aspect of each kidney contains the hilum, where the renal artery and nerve enter and the renal vein and ureter exit. Blood flow to the kidney is supplied by the renal artery, which branches off the abdominal aorta and enters the kidney through the renal sinus. Blood leaves the kidney through the renal vein, which empties into the abdominal inferior vena cava.
The nephron, the functional unit of the kidney, is composed of the renal corpuscle, proximal convoluted tubule, Henle’s loop, distal convoluted tubule, and collecting ducts. Each kidney contains an estimated 1 million nephrons that are individually capable of producing urine. These nephrons cannot be reproduced once destroyed. The renal corpuscle contains the glomerulus, a web of tightly convoluted capillaries, and Bowman’s capsule, which surrounds and supports these structures. Blood flows through the afferent arteriole into the glomerulus and out the efferent arteriole. Renal blood flow accounts for 21% of cardiac output, or 1200 mL/min. Without adequate renal blood flow the kidneys are unable to function adequately. Specialized cells called juxtaglomerular cells are located at the entrance to the glomerulus of the afferent arteriole in 15% of nephrons. These specialized cells sense changes in pressure and sodium concentration and play a role in the renin-angiotensin-aldosterone (RAA) system.
Filtration of plasma in the renal corpuscle is the first step in urine production and helps the kidneys rid the body of wastes and retain water and essential solutes. Pressure generated as blood courses through the tight web of capillaries in the glomerulus, along with oncotic pressure within the blood, is greater than pressure created by Bowman’s capsule, so plasma or filtrate and small solutes cross the semipermeable epithelial capillary lining. Injury to the glomerulus, such as ischemia or inflammation, increases permeability of the capillary membrane and allows larger molecules (red blood cells [RBCs], epithelial casts, protein, or white blood cells [WBCs]) to cross. Decreased oncotic pressure, often the result of decreased serum albumin levels, or decreased pressure within the glomerulus produced by systemic hypotension decreases glomerular filtration rate (GFR) and eventually urine output. GFR in the average adult is 125 mL/min or 180 L/day.
Tubules, Henle’s loop, and collecting ducts excrete waste products (e.g., urea, nitrogen, creatinine, drug metabolites), reabsorb water and solutes (potassium, sodium, chloride, hydrogen, glucose, and amino acids) from filtrate, and secrete excess solutes the body does not need into filtrate. Osmosis, diffusion, and active transport occur between the nephron and surrounding capillaries. Hormonal control regulates reabsorption and secretion in the nephron.
The RAA system and antidiuretic hormone (ADH) are feedback-loop systems within the body that maintain homeostasis. Serum osmolarity increases and causes stimulation of the hypothalamus, which releases ADH. Nephron permeability increases, so additional water is absorbed, serum osmolarity returns to normal, and ADH release stops. Pressure changes in the glomerulus are overcome by vasodilation and constriction of the afferent arteriole by a process called autoregulation. This autoregulation keeps pressure in the glomerulus within a wide range of systolic blood pressures. When range is exceeded, autoregulation fails and epithelial damage occurs with eventual scarring and sclerosis followed by decreased permeability, GFR, and urine output. Inadequate nephron perfusion stimulates the juxtaglomerular apparatus to secrete renin that converts angiotensinogen to angiotensin I, which stimulates aldosterone release from the adrenal cortex and reabsorption of sodium and water by the nephron. Conversion of angiotensin I to angiotensin II by an enzyme in the lung causes peripheral vasoconstriction. Perfusion increases to the nephron, and the cycle is altered.
Without a functioning kidney and adequate urine production, homeostasis is severely impaired. Fluid and electrolyte imbalance, accumulation of urea and creatinine, decreased excretion of drug metabolites, and inadequate reabsorption of amino acids and glucose occur. The kidneys help convert vitamin D into its active form to ensure calcium absorption from intestines and secrete erythropoietin for stimulation of RBC production in bone marrow. Consequently, altered renal function decreases bone mineralization and oxygen-carrying capacity of the blood.
The renal pelvis narrows to enter the ureter, where urine is moved to the bladder by peristaltic contractions. The muscular bladder stores urine until release to the urethra by the micturition reflex.
External genitalia are also part of the GU system. Female genitalia consist of the vestibule, the space into which the urethra and vagina open, and surrounding labia minora and majora. Anatomic position and the short length of the female urethra are responsible for the high frequency of UTIs in females.
Male external genitalia include penis, scrotum, and scrotal contents. Scrotal contents include the testes, tubules that carry developing sperm cells and secrete testosterone, and the epididymis, which lies along the posterior testes and is the final maturation area for sperm. The prostate is glandular muscle tissue that surrounds the urethra at the base of the bladder. Enlargement of the prostate can cause outlet obstruction and urinary retention. The penis consists of three columns of erectile tissue that become engorged with blood, producing erection. Two columns of corpora cavernosa form the dorsum and sides of the penis and the corpus spongiosum forms the base and glans. Clinical manifestations of GU disease frequently involve external genitalia.
PATIENT ASSESSMENT
Assessment of the GU system should determine history of hypertension, diabetes, previous infections, prostatitis, urethritis, bladder or urethral damage during childbirth, history of renal calculi, and recurrent UTIs. A detailed drug list, including prescription, over-the-counter (OTC), herbal preparations, and illicit drugs should be obtained. Identification of any history of exposure to occupational chemicals or toxins may identify contact with substances that could cause nephrotoxicity. Sexual history should include discussion of risk factors that can cause GU symptoms (e.g., use of contraceptive jellies or creams, multiple partners, abnormal penile or vaginal discharges, unsafe sexual practices, history of STIs). GU complaints often arise from changes in urinary patterns; for example, frequency, dysuria, urgency, dribbling, or incontinence.
Urinary disorders can be identified by the patient’s own subjective interpretation (e.g., changes in output, voiding pattern, location of pain). Obtaining a urine sample for analysis can validate the nurse’s suspicions. Gross visual examination for color, clarity, and amount should be done before urine is sent to the laboratory. Palpation and percussion of the kidneys may reveal costal vertebral tenderness, structural asymmetry, or the presence of masses.
Female patients, particularly those of reproductive age, warrant additional assessment for a broad spectrum of complaints. One should always consider the possibility of an unknown pregnancy and take a careful menstrual history, including use of contraceptives. If the patient is pregnant, fetal heart tones are assessed for presence, location, and rate. When a woman has a specific genital concern, a vaginal examination is indicated. Any discharge or bleeding should be noted and described by character and amount.
Males should be assessed for problems specific to their GU anatomy, including presence of a slow stream, inability to void, penile discharge, or warts.
Hematuria, the presence of blood in the urine, may be the primary complaint or may accompany other symptoms. A detailed medication and diet history may uncover other causes for discoloration of urine—foods such as beets, rhubarb, and blackberries and medications such as phenytoin are common nonhematuric causes of red or dark urine. Hematuria can be confirmed by urinalysis (UA); however, microscopic hematuria on a single test is common. Early-stream hematuria suggests bleeding from the urethra, hematuria throughout the stream indicates upper GU tract bleeding, and bleeding at the end suggests bladder neck or urethral bleeding. Complete urinalysis and urine cytologic study may indicate the need for further diagnostic testing for urologic cancer, renal disease, infection, or renal calculi as the source of hematuria.
Pain should be assessed using the PQRST mnemonic—provocation, quality, region or radiation, severity, and time. The most severe pain associated with the GU system is renal colic caused by calculi. Increased pressure and dilation of the kidney and urinary collecting system cause sudden, unbearable pain. The patient usually presents with restlessness and pallor and complains of flank pain that often radiates to the abdomen and groin. If the stone lodges in the bladder, urinary frequency and urgency develop. Pain can cause tachypnea and tachycardia with elevated blood pressure. Oliguria, defined as urine output less than 400 mL in 24 hours, or anuria, less than 75 mL in 24 hours, may be the presenting symptom. The cause is usually obstruction; however, blood chemistry values should be evaluated for azotemia, which indicates renal failure from prolonged obstruction leading to hydronephrosis or other causes. If the patient has a urinary catheter in place, patency should be assessed. A physical examination can identify urinary retention by palpating the bladder as a firm mass above the symphysis pubis, with an urge to void on palpation; bladder scanning using ultrasonography may also be used to detect bladder distention. History should be obtained to identify drugs that contribute to retention, including OTC nasal decongestants containing anticholinergic ingredients. A neurologic examination should be performed to rule out spinal cord injury or disease that can interfere with the micturition reflex. The prostate is examined for enlargement as the cause of obstruction. After the patient has attempted to void, a urethral catheter may be inserted for residual volume. Bedside bladder ultrasonography may avoid the need for catheterization and allow assessment of prevoid and postvoid volume. If the catheter cannot be inserted without resistance, a suprapubic bladder tap or assistance from a urologist may be necessary. With a residual volume greater than 500 mL, the catheter may be left in place to allow the bladder to regain muscle tone. If residual volume is minimal, further diagnostic evaluation is aimed at identifying the cause.
SPECIFIC CONDITIONS
Acute Renal Failure
Until recently, a systemic definition of ARF was lacking. In 2004 the Acute Dialysis Quality Initiative (ADQI) group published the RIFLE criteria for classification of ARF (Table 35-1). Because baseline values may not be available, the Crockcroft-Gault equation is used most often in the ED: GFR mL/min equals (140 − age in yrs)(weight in kg)(0.85 if female) divided by (72 × serum creatinine mol/L). Azotemia, or uremia, refers to accumulation of nitrogen waste products in the blood. Acute azotemia generally refers to the patient with ARF, which usually develops over a period of days; however, chronic renal failure (CRF) patients can experience acute episodes because of noncompliance or other medical conditions.
| ARF, Acute renal failure; GFR, glomerular filtration rate; UO, urine output. | |
| Risk (R) | Increase serum creatinine level × 1.5 or decrease in GFR by 25%, or UO <0.5 mL/kg/hr for 6 hours |
| Injury (I) | Increase serum creatinine level × 2 or decrease in GFR by 50%, or UO <0.5 mL/kg/hr for 12 hours |
| Failure (F) | Increase serum creatinine level × 3 or decrease in GFR by 75%, or serum creatinine level ≥4 mg/dL; UO <0.3 mL/kg/hr for 24 hours, or anuria for 12 hours |
| Loss (L) | Persistent ARF, complete loss of kidney function >4 weeks |
| End-stage kidney disease (E) | Loss of kidney function >3 months |
ARF has prerenal, intrarenal, or postrenal causes. Prerenal causes include syndromes that decrease blood flow to the kidney and therefore alter its ability to function. Those include hypovolemia, decreased cardiac output, decreased peripheral vascular resistance or obstruction of the renal vascular system. Intrarenal causes are those that cause damage to the kidney tubules (acute tubular necrosis) and include nephrotoxic agents (aminoglycosides, nonsteroidal antiinflammatory agents, contrast dye, crush injury, and rhabdomyolysis) or diseases that damage the vascular or interstitial tissue (hypertension, diabetes, lupus, and infectious processes). Postrenal causes are those diseases resulting in obstruction of the urinary tract such as calculi, prostatic hypertrophy, tumors, strictures, or neurologic causes affecting emptying of the urinary system. ARF is largely preventable.
Symptoms of ARF include short-term weight gain or loss, nausea and vomiting, hematemesis, melena, dysrhythmias, dyspnea, stupor, or coma. Compromise of airway, breathing, circulation, and neurologic function requires intervention. Fever may be associated with infectious or inflammatory events. Fever reduction measures should be instituted to prevent continued rise of nitrogenous waste products by catabolic effect of fever.
Hyperkalemia, hyponatremia, hypocalcemia, hyperphosphatemia, and volume overload are the most common fluid and electrolyte imbalances resulting from loss of the kidney’s ability to excrete potassium and phosphorus, conserve sodium, and eliminate excess volume. Calcium is inversely related to phosphorus. In renal failure, calcium levels decrease because of the rise in phosphorus and the inability of the kidney to convert vitamin D to its active form, which facilitates calcium absorption from the gut. The electrocardiogram (ECG) may reveal tall peaked T waves, widened QRS, and prolonged PR interval secondary to hyperkalemia. Administration of intravenous (IV) calcium may be needed to antagonize the membrane and improve cardiac conductivity until removal of excess potassium by emergency dialysis can be initiated. IV calcium works within minutes, but duration is short, as evidenced by return of ECG changes. Administration of IV sodium bicarbonate (NaHCO 3), glucose, and insulin redistributes extracellular potassium into the intracellular fluid, works within 15 to 30 minutes, and lasts approximately 4 hours. Potassium can also be removed by cation exchange resin (e.g., sodium polystyrene sulfonate [Kayexalate]), but onset of action is 60 minutes when given rectally and 120 minutes after oral administration. Nebulized albuterol may also be administered to manage hyperkalemia.
Urine output may be increased or decreased. If ARF is nonoliguric, large volumes of fluid can be lost, so the patient may be dehydrated and hypotensive. Volume replacement with normal saline or volume expanders is guided by monitoring jugular vein distention, lung auscultation, and vital signs or by invasive lines such as central venous pressure and pulmonary artery catheters to monitor fluid status, avoiding further ischemic injury to renal tissue. If ARF presents with oliguria, the patient may be volume overloaded and hypertensive, so minimal fluid is given until the volume can be removed by diuretics or through hemodialysis. Metabolic acidosis occurs because renal tubules can no longer regulate concentration of hydrogen ions. IV NaHCO 3 may be used unless contraindicated by volume status.
Indications for emergency dialysis include stupor or coma (caused by rising nitrogen waste products in the blood and metabolic changes), volume overload and pulmonary edema, dangerous hyperkalemia, and acidosis. Emergency hemodialysis requires vascular access (usually a temporary femoral or subclavian dual-lumen catheter or internal shunt) and an artificial kidney (dialyzer) to act as a semipermeable membrane. The dialysate must be low in ions that the body needs to excrete and high in those to be reabsorbed. Hemodynamically unstable patients may require continuous renal replacement therapy, also called continuous extracorporeal renal therapy.
After initial stabilization, history and diagnostic testing focus on identifying the cause of ARF. Tests include serial blood chemistry values, UA with sodium and potassium concentrations, chest radiograph, renal ultrasonography and Doppler studies, or computed tomography (CT) scan. Imaging procedures are usually done without contrast media because of toxic effects of the media on renal tubules. When contrast is needed, acetylcysteine (Mucomyst) may be administered before and after the contrast study in patients with altered renal function to minimize toxic renal effects.
Dialysis Access Complications
Chronic renal failure requiring dialysis is known as end-stage renal disease. Renal replacement therapy may be provided by peritoneal dialysis or hemodialysis. Peritoneal dialysis involves instilling 1 to 2 L of dialysate fluid containing varying amounts of glucose, magnesium, calcium, chloride, and lactate into the abdomen. The peritoneal membrane acts as a semipermeable pathway for exchange of solutes and water between the vascular peritoneal space and dialysate by osmosis and diffusion. Access to the peritoneal cavity is achieved through a plastic catheter held in place by a Dacron cuff. Peritonitis and exit site infections may bring the patient to the ED with complaints of abdominal pain, nausea and vomiting, fever, and cloudy dialysate fluid. Antibiotics may be given IV and added to dialysate. If this is unsuccessful, the catheter should be removed and hemodialysis initiated until peritonitis clears. Unless scarring impairs permeability of the peritoneal membrane, the catheter can be surgically replaced and peritoneal dialysis reinitiated. Care in the ED may include obtaining a sample of peritoneal fluid after installation of dialysate. During access of the peritoneal catheter, careful adherence to aseptic technique, limiting and masking persons present in the room, and use of sterile gloves to prevent contamination during access of the peritoneal catheter are extremely important to prevent infection and resultant peritonitis.
Clotted vascular access frequently brings patients with CRF to the ED. Arteriovenous fistulas are surgical connections of a native artery and vein in an extremity or insertion of Gore-Tex graft material to form the connection (Figure 35-1). Available sites suitable for vascular access become exhausted, so permanent subclavian dual-lumen catheters are placed for hemodialysis. Clotted vascular access should be emergently declotted with use of locally instilled or infused fibrinolytics or surgery. Grafts, fistulas, and insertion sites also become infected and may progress to septicemia. Local symptoms include redness, drainage, or edema. Blood cultures and a complete blood count (CBC) should be obtained to rule out systemic infection. Access removal may be necessary, so temporary subclavian or femoral access (replaced every 2 or 3 days) can be used until blood is free of infection. Some type of anticoagulant will reside in the lumens of a dual-lumen dialysis catheter to prevent clotting. When accessing the catheter, failure to withdraw this anticoagulant could cause serious bleeding complications due to alteration of coagulation status.
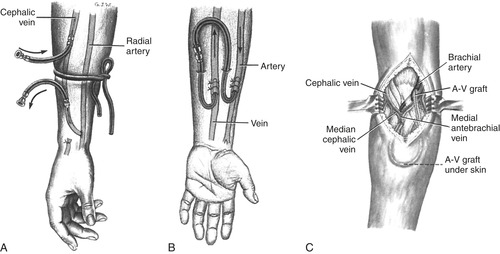 |
| FIGURE 35-1 Circulatory access for hemodialysis. A, External (temporary) arteriovenous cannula (shunt). B, Internal (permanent) arteriovenous fistula. C, Internal (permanent) arteriovenous (A-V) graft. (From Thompson JM, McFarland GK, Hirsch JE et al: Mosby’s clinical nursing, ed 5, St. Louis, 2002, Mosby.) |
Rhabdomyolysis
Skeletal muscle destruction with subsequent release of myoglobin into the circulatory system causes rhabdomyolysis, which can lead to ARF from hypovolemia and tubular necrosis. There are many different causes, including crush injuries, drug or toxin ingestion (including the statin drug class for hypercholesterolemia), infection, burns, or metabolic disturbances. Crush injuries may be caused by entrapment, such as prolonged compression of the abdomen or a limb after a motor vehicle crash. Fluid shifts from the intravascular space into the interstitial space in the area of injury or systemically and can cause the patient to become profoundly hypovolemic, leading to decreased blood flow to the kidneys and resultant decrease in function. Electrolyte imbalances are also associated with the fluid shift. Hyperkalemia is predominant, but hypocalcemia and hyperuricemia are also present. There is an increase in serum creatine kinase (CK), blood urea nitrogen (BUN), creatinine, phosphate (PO 4), uric acid, aspartate aminotransferase (AST), and alanine aminotransferase (ALT). Urine will have a reddish brown color as a result of myoglobinuria (brown urine and clear serum). Proteinuria and hematuria are noted on urinalysis; however, few or no RBCs are seen during microscopic examination.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
