The Musculoskeletal System
Objectives
1. Recall the normal anatomy of the musculoskeletal system.
2. Describe how the musculoskeletal system provides the function of motion.
3. Explain how the musculoskeletal system provides protection for the body.
4. Identify the steps included in a nursing assessment of the musculoskeletal system.
5. Discuss the following diagnostic tests: bone scan, arthroscopy, electromyography.
6. List ways in which the elderly can increase musculoskeletal strength and protect bones.
2. Institute measures to reduce the chance of contracture for patients with musculoskeletal injuries.
3. Assist patients with musculoskeletal injuries with active or passive range of motion.
4. Provide care for a patient who has undergone an arthroscopy.
5. Teach a patient to properly use crutches.
6. Teach an elderly patient with a mobility problem about ways to prevent a fall at home.
Key Terms
ankylosis (ăng-kĭ-LŌ-sĭs, p. 728)
cartilage (KĂR-tĭ-lăzh, p. 716)
contractures (kŏn-TRĂK-chŭrz, p. 727)
crepitation (KRĔP-ĭ-tā-shŭn, p. 718)
isometric exercises (ī-sō-MĔT-rĭk, p. 728)
kyphosis (kī-PHŌ-sĭs, p. 724)
ligaments (LĬG-ă-mĕntz, p. 716)
orthopedic (ŏr-thō-PĒ-dĭk, p. 719)
ossification (ŏs-ĭ-fĭ-KĀ-shŭn, p. 718)
tendons (TĔN-dŏnz, p. 716)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Overview of Anatomy and Physiology of the Musculoskeletal System
What are the Structures of the Musculoskeletal System?
• A total of 206 bones make up the human skeleton (Figure 32-1).
• Bone is either compact or spongy. Spongy bone contains red bone marrow (Figure 32-2).
• Bones are classified as long, short, flat, or irregular.
• Each bone has markings on its surface that make it unique (Table 32-1).
• Ligaments join the bones of a joint together.
• Tendons are connective tissues that provide joint movement.
• A bursa is a fluid-filled sac that provides cushioning at friction points in a freely movable joint.
• Fascia is a connective tissue that surrounds and separates the muscles.
• The muscle coverings contain blood vessels and nerves.
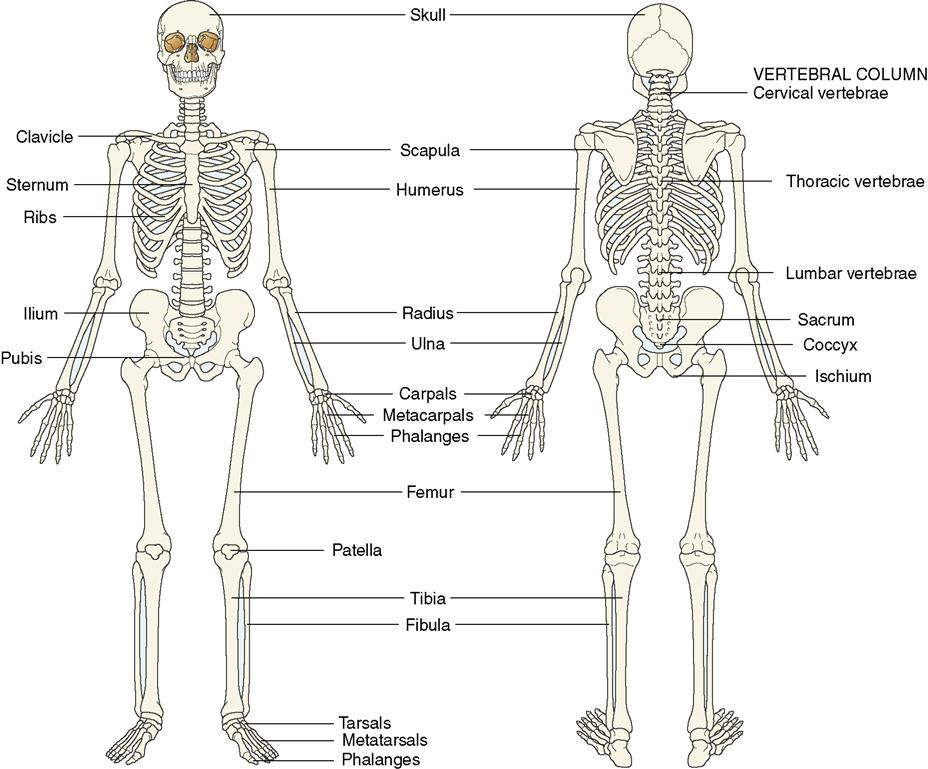
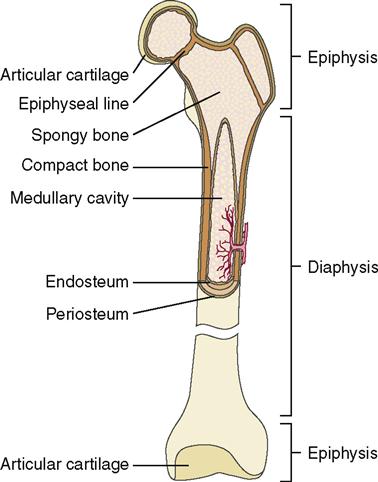
Table 32-1
Terms Related to Bone Markings
| Term | Description | Examples |
| Projections for Articulation | ||
| Condyle (KŎN-dīl) | Smooth, rounded articular surface | Occipital condyle on the occipital bone; lateral and medial condyles on the femur |
| Facet (FĂS-ĕt) | Smooth, nearly flat articular surface | Facets on thoracic vertebrae for articulation with ribs |
| Head (HĔD) | Enlarged, often rounded, end of bone | Head of the humerus; head of the femur |
| Projections for Muscle Attachment | ||
| Crest (KRĔST) | Narrow ridge of bone | Iliac crest on the ilium |
| Epicondyle (ĕ-pĭh-KŎN-dīl) | Bony bulge adjacent to or above a condyle | Lateral and medial epicondyles of the femur |
| Process (PRĂH-sĕs) | Any projection on a bone; often pointed and sharp | Styloid process on the temporal bone |
| Spine (SPĪN) | Sharp, slender projection | Spine of the scapula |
| Trochanter (trō-KĂN-tŭr) | Large, blunt, irregularly shaped projection | Greater and lesser trochanters on the femur |
| Tubercle (TŪ-bŭr-kŭl) | Small, rounded, knoblike projection | Greater tubercle of the humerus |
| Tuberosity (tū-bŭr-ĂS-ĭ-tē) | Similar to a tubercle but usually larger | Tibial tuberosity on the tibia |
| Depressions, Openings, and Cavities | ||
| Fissure (FĬSH-ŭr) | Narrow cleft or slit; usually for passage of blood vessels and nerves | Superior orbital fissure |
| Foramen (fō-RĀ-mĕn) | Opening through a bone; usually for passage of blood vessels and nerves | Foramen magnum in the occipital bone |
| Fossa (FĂW-să) | A smooth, shallow depression | Mandibular fossa on the temporal bone; olecranon fossa on the humerus |
| Fovea (FŌH-vē-ă) | A small pit or depression | Fovea capitis femoris on the head of the femur |
| Meatus (mē-ĀT-ŭs) | A tubelike passageway; tunnel | External auditory meatus in the temporal bone |
| Sinus (SĪ-nŭs) | A cavity or hollow space in a bone | Frontal sinus in the frontal bone |
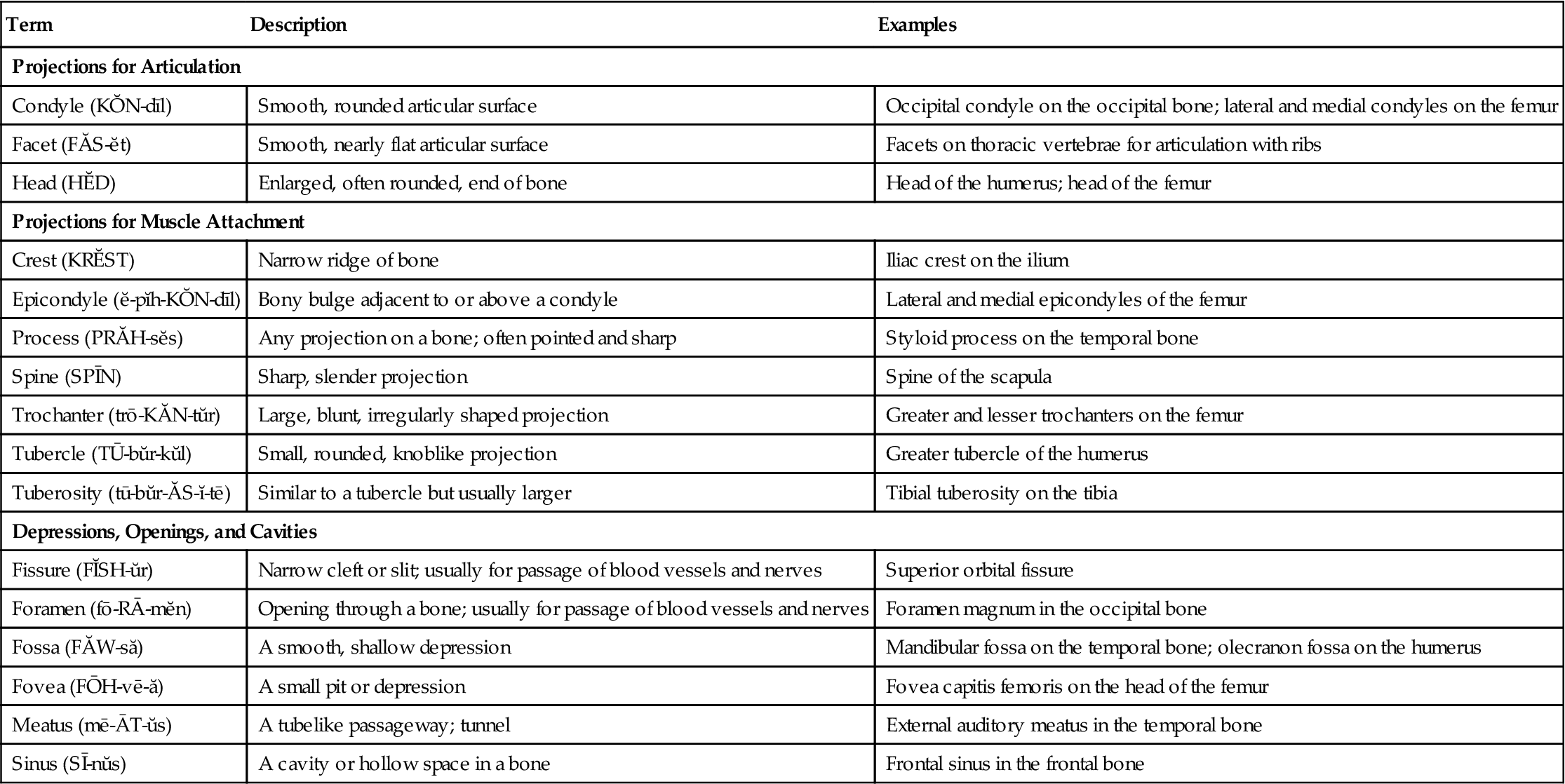
From Applegate, E.J. (2010). The Anatomy and Physiology Learning System (4th ed.). Philadelphia: Saunders.
What are the functions of the bones?
• Bones provide shape to the body.
• The skeleton provides a rigid framework that supports the internal organs and the skin.
• The skeleton protects the internal organs of the body.
• The skeleton provides attachments for tendons and ligaments and contributes to movement of the body.
• The red bone marrow in the spongy bones forms red blood cells, white blood cells, and platelets.
• The bones store and release minerals, such as calcium and phosphorus.
• The blood and lymph vessels in the canals transport nutrients to the bone cells and remove wastes.
What are the Functions of the Muscles?
What Changes Occur in the Musculoskeletal System with Aging?
• Bone density decreases because of the resorption of minerals.
• The loss of bone mass, or osteoporosis, occurs with aging and is more severe in women.
• The bones of elderly people are brittle and less compact; thus they break easily.
• Joint motion may decrease, limiting mobility; swelling may occur.
• Ligaments become calcified and lose their elasticity.
• Tendons shrink and become sclerotic, slowing muscle movement.
Musculoskeletal Disorders
Causes
Disease, trauma, malnutrition, and aging all contribute to musculoskeletal problems. Trauma may cause bruising, strain, sprain, or fracture. Poor nutrition may deprive the body of sufficient calcium and phosphorus to build strong bones. Inadequate protein intake can cause muscle wasting. Malignant tumors place a large nutritional demand on the body, and nutritional imbalances may occur that cause muscle wasting. Tumor may invade bone as either a primary or metastatic cancer. The decrease in estrogen production after menopause in women is thought to be a contributing factor to the occurrence of osteoporosis.
Prevention
Preservation of motion and mobility are important to prevent long-term orthopedic (refers to the function and structure of the musculoskeletal system) disability. Weight training and exercise throughout life is needed to maintain bone mass and can decrease the incidence of osteoporosis and increase muscle strength, mass, agility, balance, and coordination, thereby preventing falls and consequent fractures. One of the proposed Healthy People 2020 objectives is to reduce hospitalizations related to osteoporosis-related hip fractures. For the older adult, maintenance of an exercise diary or personal interviews following workouts helped to increase adherence to recommended weight training and exercise programs (Yeom et al., 2009).
Learning to lift and move objects correctly by using large muscle groups can help prevent muscle strain and sprains. Using seat belts when riding in an automobile can reduce the incidence of trauma to bone and muscle during accidents. Wearing bicycle, motorcycle, and other sports helmets will reduce the incidence of skull fractures. Consuming recommended amounts of calcium throughout the life span, obtaining sufficient vitamin D from sunshine, and maintaining adequate protein intake all help build healthy bone and muscle (Kalro, 2009). Refraining from using steroids on a long-term basis can help prevent osteoporosis and fractures. In a study of retired National Football League players, steroid use
was linked to musculoskeletal disorders, particular joint health, and to the development of osteoarthritis, physical inactivity, depression, obesity, and diabetes (Brockenbrough, 2009).
Diagnostic Tests and Procedures
Specific diagnostic tests of the musculoskeletal system are listed in Table 32-2. Blood counts, blood cultures, and various tests for problems of the immune system may also be performed to detect rheumatoid arthritis or other connective tissue diseases. Other tests include an erythrocyte sedimentation rate (ESR), serum protein electrophoresis, and tests to determine the levels of serum complement and immunoglobulins (see Chapter 10).
Table 32-2
Diagnostic Tests for Musculoskeletal Disorders








