Drugs Used to Treat Lower Respiratory Disease
Objectives
1 Identify the structures of the lower respiratory tract and their functions.
3 Describe the physiology of respirations and identify components of blood gases.
4 Cite nursing assessments used to evaluate the respiratory status of a patient.
6 Distinguish the mechanisms of action of expectorants, antitussives, and mucolytic agents.
Key Terms
ventilation ( ) (p. 483)
) (p. 483)
perfusion ( ) (p. 484)
) (p. 484)
diffusion ( ) (p. 484)
) (p. 484)
goblet cells ( ) (p. 484)
) (p. 484)
obstructive airway diseases (
 ) (p. 485)
) (p. 485)
bronchospasm ( ) (p. 485)
) (p. 485)
chronic obstructive pulmonary disease (COPD) ( ) (p. 485)
) (p. 485)
chronic airflow limitation disease (CALD) (
 ) (p. 485)
) (p. 485)
restrictive airway diseases ( ) (p. 485)
) (p. 485)
arterial blood gases (ABGs) ( ) (p. 485)
) (p. 485)
oxygen saturation ( ) (p. 485)
) (p. 485)
spirometry ( ) (p. 485)
) (p. 485)
cough ( ) (p. 485)
) (p. 485)
asthma ( ) (p. 486)
) (p. 486)
bronchitis ( ) (p. 486)
) (p. 486)
emphysema ( ) (p. 486)
) (p. 486)
bronchodilation ( ) (p. 489)
) (p. 489)
expectorants ( ) (p. 489)
) (p. 489)
antitussives ( ) (p. 489)
) (p. 489)
mucolytic agents ( ) (p. 489)
) (p. 489)
bronchodilators ( ) (p. 489)
) (p. 489)
anti-inflammatory agents ( ) (p. 490)
) (p. 490)
immunomodulators ( ) (p. 490)
) (p. 490)
![]() http://evolve.elsevier.com/Clayton
http://evolve.elsevier.com/Clayton
Lower Respiratory Tract Anatomy and Physiology
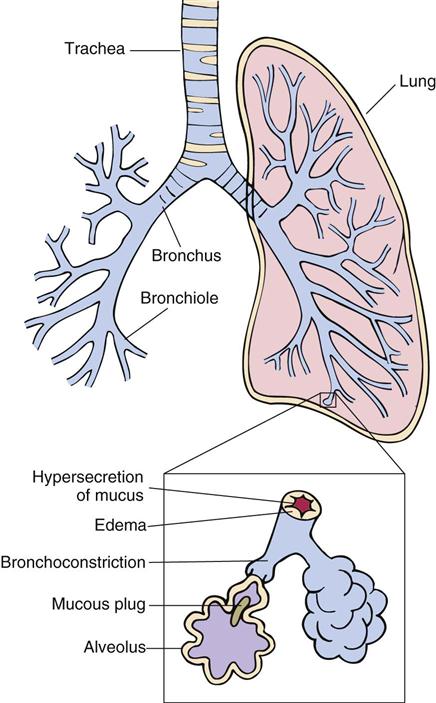
The respiratory system is a series of airways that start with the nose and mouth and end at the alveolar sacs. The nose and mouth airways connect at the pharynx. Passing out of the pharynx, the airways divide into the esophagus of the gastrointestinal tract and the larynx (voice box) and trachea of the respiratory tract. The trachea divides into the right and left mainstem bronchi, which enter the lungs. The bronchi subdivide in each lung into many smaller bronchioles, which further subdivide into many smaller airways called alveolar ducts that terminate in alveolar sacs. The alveolar sacs are surrounded by capillaries of the blood circulatory system. Human lungs contain 300 to 500 million sacs for gaseous exchange and have a surface area approximately equal to that of a tennis court. The anatomic parts of the body associated with the lower respiratory system are the larynx, trachea, bronchi, bronchioles, and alveolar sacs (Figure 31-1).
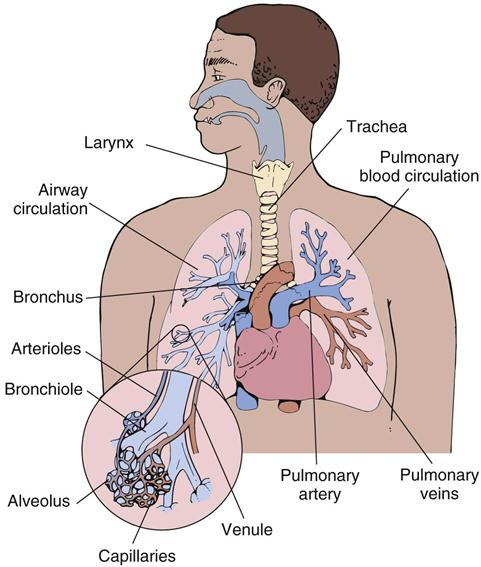
The primary function of the lower respiratory tract is the ventilatory cycle. Ventilation is the movement of air in and out of the lungs. Inhalation is the process of transport (inhalation) of air containing oxygen to the alveolar sacs, exchange of oxygen for carbon dioxide across the alveolar membranes containing blood capillaries, and exhalation of “stale air,” including carbon dioxide. Ventilation of the lungs is accomplished by contraction and relaxation of the diaphragmatic and intercostal muscles (muscles between the ribs). During inspiration, the diaphragmatic and intercostal muscles contract, creating a vacuum in the lungs and pulling air in through the mouth and nose. During exhalation, relaxation of the muscles allows the chest to return to its unexpanded position, forcing air out of the lungs.
Blood flow through the pulmonary arteries to the capillaries surrounding the alveoli to the pulmonary veins is called perfusion. Diffusion is the process by which oxygen (O2) passes across the alveolar membrane to the blood in the capillaries and carbon dioxide (CO2) passes from the blood to the alveolar sacs. Oxygen is transported by combining with hemoglobin in red blood cells or by dissolving in the blood plasma. Blood circulation provides distribution of oxygen to the body’s cells for the sustenance of life. Ventilation and perfusion must be equal to maintain homeostasis.
The fluids of the respiratory tract originate from specialized mucous glands (goblet cells) and serous glands that line the respiratory tract. The goblet cells produce gelatinous mucus that forms a thin layer over the interior surfaces of the trachea, bronchi, and bronchioles. Secretion of mucus is increased by exposure to irritants, such as smoke, airborne particulate matter, and bacteria. The serous glands are controlled by the cholinergic nervous system. When stimulated, the serous glands secrete a watery fluid to the interior surface of the bronchial tree. There, the mucous secretions of the goblet cells and the watery secretions of the serous glands combine to form respiratory tract fluid.
Normally, respiratory tract fluid forms a protective layer over the trachea, bronchi, and bronchioles. Foreign bodies, such as smoke particles and bacteria, are caught in the respiratory tract fluid and are swept upward by ciliary hairs that line the bronchi and trachea to the larynx, where they are removed by the cough reflex. The expectorated (coughed up) material contains pulmonary mucous secretions, foreign particulate matter such as smoke and bacteria, and epithelial cells sloughed from the lining of the airways. Common names given to the expectorated mass are sputum and phlegm. If too much mucus is secreted as a result of chronic irritation, cilia are destroyed by chronic inhalation of smoke, dehydration dries the mucus, or anticholinergic agents inhibit watery secretions from the serous glands; the mucus becomes viscous, forming thick plugs in the bronchiolar airways (Figure 31-2). These thick plugs are difficult to eliminate. The resultant colonization of pathogenic microorganisms in the lower respiratory tract causes additional mucous secretions and the possible development of pneumonia from trapped bacteria.
The smooth muscle of the tracheobronchial tree is innervated by the parasympathetic and sympathetic branches of the autonomic nervous system. Stimulation of the cholinergic nerves causes bronchial constriction and increased mucus secretion. Sympathetic stimulation of adrenergic nerves causes dilation of bronchial and bronchiolar airways and inhibition of respiratory tract fluids. Both beta-1 and beta-2 adrenergic receptors are present, but the beta-2 receptors predominate.
Common Lower Respiratory Diseases
Respiratory diseases are often divided into two types, obstructive and restrictive. Obstructive airway diseases are those that narrow air passages, create turbulence, and increase resistance to airflow. Diseases cause narrowing of the airways through smooth muscle constriction (bronchospasm), edema, inflammation of the bronchial walls, or excess mucus secretion. Examples of obstructive lung disease are asthma and acute bronchitis. Chronic obstructive illnesses are also referred to as chronic obstructive pulmonary disease (COPD) and chronic airflow limitation disease (CALD); the terms are used interchangeably. COPD affects about 20% of U.S. adults and is the second most common cause of disability and the fourth leading cause of death. Restrictive airway diseases are those in which lung expansion is limited from loss of elasticity (e.g., pulmonary fibrosis) or physical deformity of the chest (e.g., kyphoscoliosis). Chronic bronchitis and emphysema are examples of both a restrictive and an obstructive lung disease.
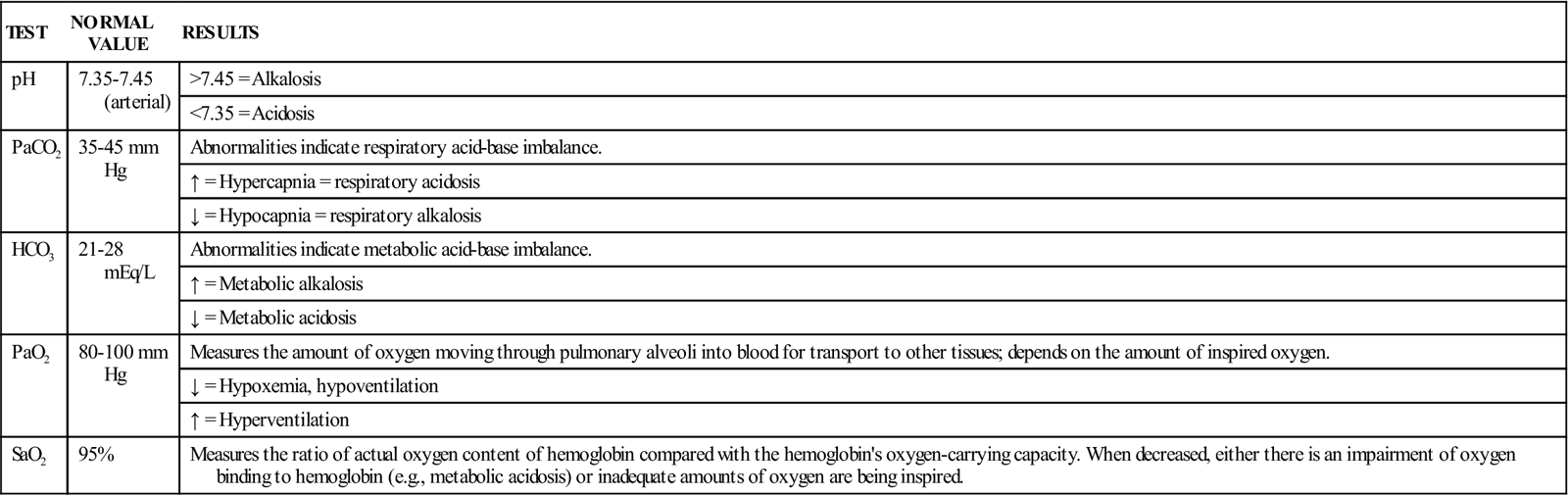
Pulmonary function tests have been developed to assess the ventilation and diffusion capacity of the lungs to assist in diagnosis and to give an objective assessment of improvement or deterioration of the patient’s clinical condition. The best indicators of overall pulmonary function (ventilation and diffusion) are the partial pressure of arterial blood gases (ABGs) (e.g., PaO2 and PaCO2) and pH (Table 31-1). To determine ABGs, a sample of arterial blood must be drawn and immediately analyzed to measure the pH and partial pressures of oxygen and carbon dioxide in the blood. Another measure that is more readily available and noninvasive is the oxygen saturation of hemoglobin. Oxygen saturation (SaO2) is the ratio, expressed as a percentage, of the oxygen actually bound to hemoglobin compared with the maximum amount of oxygen that could be bound to hemoglobin (see Table 31-1). Oxygen saturation is routinely used because a transcutaneous monitor (oximeter) is easily attached to the skin to measure and report oxygen saturation continuously.
Table 31-1
Laboratory Tests Used to Assess Respiratory Function
| TEST | NORMAL VALUE | RESULTS |
| pH | 7.35-7.45 (arterial) | >7.45 = Alkalosis |
| <7.35 = Acidosis | ||
| PaCO2 | 35-45 mm Hg | Abnormalities indicate respiratory acid-base imbalance. |
| ↑ = Hypercapnia = respiratory acidosis | ||
| ↓ = Hypocapnia = respiratory alkalosis | ||
| HCO3 | 21-28 mEq/L | Abnormalities indicate metabolic acid-base imbalance. |
| ↑ = Metabolic alkalosis | ||
| ↓ = Metabolic acidosis | ||
| PaO2 | 80-100 mm Hg | Measures the amount of oxygen moving through pulmonary alveoli into blood for transport to other tissues; depends on the amount of inspired oxygen. |
| ↓ = Hypoxemia, hypoventilation | ||
| ↑ = Hyperventilation | ||
| SaO2 | 95% | Measures the ratio of actual oxygen content of hemoglobin compared with the hemoglobin’s oxygen-carrying capacity. When decreased, either there is an impairment of oxygen binding to hemoglobin (e.g., metabolic acidosis) or inadequate amounts of oxygen are being inspired. |
Spirometry studies are routinely used to assess the capability of the patient’s lungs, thorax, and respiratory muscles for moving volumes of air during inhalation and exhalation. It is recommended that spirometry be used to diagnose airway obstruction in symptomatic patients, but it should not be used as a screening tool for asymptomatic patients. A spirometer measures volumes of air. Terms used with spirometry are listed in Table 31-2. Patients with obstructive disease usually have a normal total lung capacity (TLC), difficulty with expiration, decreased vital capacity (VC), and increased residual capacity (RC). Patients with restrictive disease have a decrease in all measured lung volumes. The forced expiratory volume in 1 second (FEV1) and the forced vital capacity (FVC) are the most commonly used pulmonary function tests. The FEV1 is used to determine the reversibility of airway disease and the effectiveness of bronchodilator therapy. The peak expiratory flow rate (PEFR) meter is not as accurate but is much less costly and more readily available than other pulmonary function test equipment. This meter is routinely used by patients at home and by health care providers to assess the benefits of therapy for treating acute and chronic asthmatic symptoms. A patient is considered to have significant reversibility of airway obstruction if there is a 15% to 20% improvement in the FEV1 or PEFR after bronchodilator therapy.
Table 31-2
Terminology Used With Spirometry
| TERM | DEFINITION |
| Tidal volume (TV) | Volume of air inspired or expired during normal breathing |
| Vital capacity (VC) | Volume of air exhaled after maximal inspiration to full expiration |
| Residual volume (RV) | Volume of air left in lungs after maximal exhalation |
| Functional residual capacity (FRC) | Volume of air left in lungs after normal exhalation |
| Total lung capacity (TLC) | Vital capacity plus residual volume (VC + RV) = TLC |
| Forced expiratory volume (FEV) | Volume of air forced out of the lungs by maximal exhalation |
| Forced expiratory volume in 1 second (FEV1) | Volume of air forced out in 1 sec to give the rate of flow |
| Forced vital capacity (FVC) | Maximal volume of air exhaled with maximal forced effort after maximal inhalation |
| Peak expiratory flow rate (PEFR) | Maximal rate of airflow produced during forced expiration |
One of the first symptoms of a respiratory disease is the presence of a cough, a reflex initiated by irritation of the airway. It is a protective beneficial mechanism for clearing excess secretions from the tracheobronchial tree. The same irritants responsible for asthma or allergy may stimulate the cough receptors, or congestion of the nasal mucosa from a cold may cause a postnasal drip into the back of the throat that stimulates the cough.
A cough is productive if it helps remove accumulated secretions and phlegm from the tracheobronchial tree. A nonproductive cough results when irritants repeatedly stimulate the cough receptors but are not removed by the coughing reflex. Excessive coughing, particularly if it is dry and nonproductive, is not only discomforting but also tends to be self-perpetuating because the rapid air expulsion further irritates the tracheobronchial mucosa.
Asthma is a common chronic airway disease that affects more than 22 million people in the United States, including 6.5 million children younger than 18 years. It is the most common chronic illness of children and accounts for about 50% of emergency department visits by children younger than 18 years. It accounts for 100 million days of restricted activity, 500,000 hospitalizations, and 4000 deaths annually. Asthma is a highly variable disease in terms of onset and frequency of attacks, length of remission, and stimuli that cause attacks. For unknown reasons, the prevalence of asthma is increasing in the United States. Mortality rates have declined overall since 1995, but a disparity among ethnic groups remains; asthma mortality is nearly 3 times higher in African American males than in white males and is 2.5 times higher in African American females than in white females.
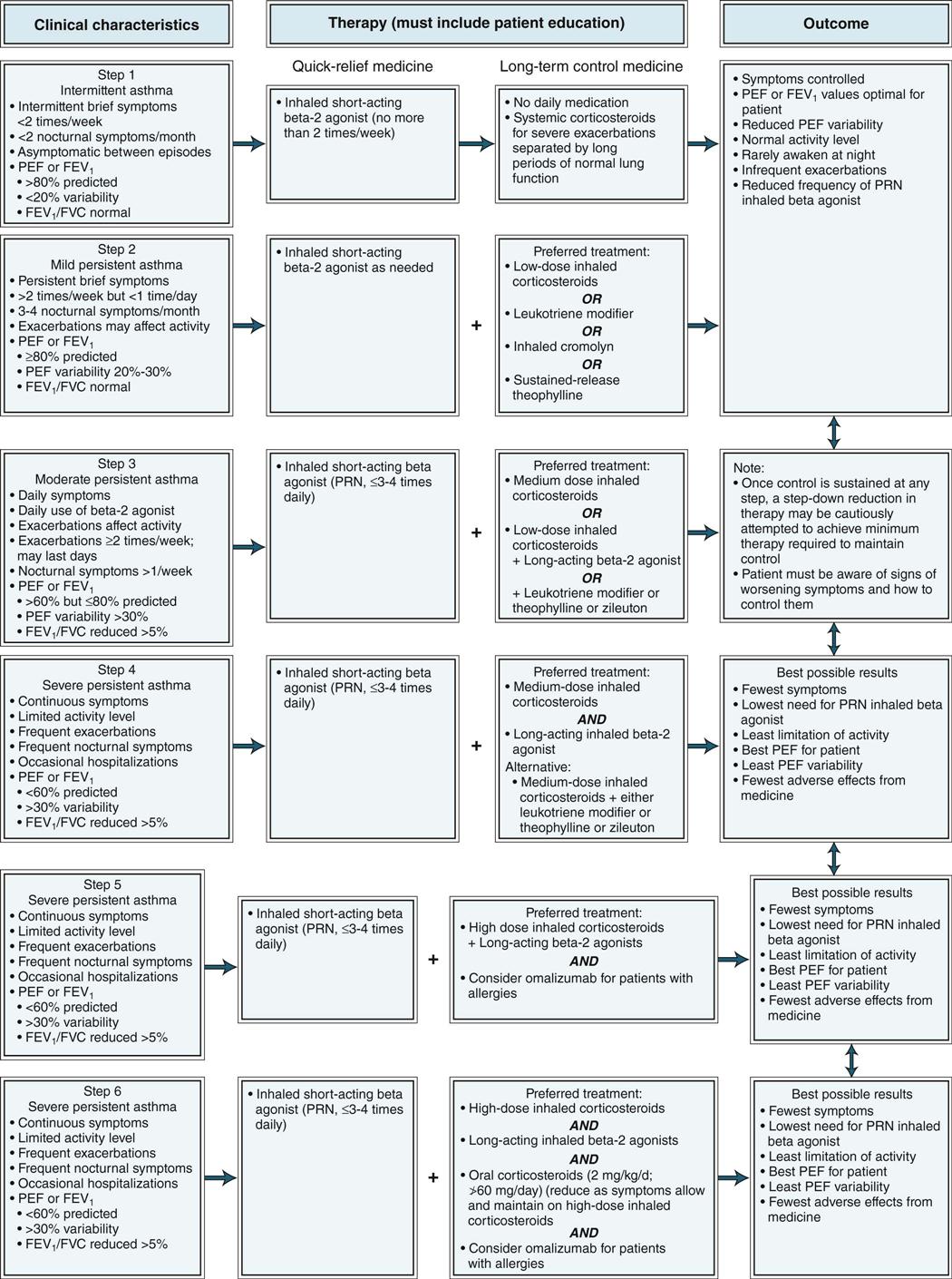
Asthma is an inflammatory disease of the bronchi and bronchioles. There are intermittent periods of acute, reversible airflow obstruction (bronchoconstriction) caused by bronchiolar inflammation and hyperresponsiveness to a variety of stimuli. Examples of stimuli that trigger bronchospasm and inflammation are respiratory viral infections, inhaled allergens, cold air, dry air, emotional stress, and smoke. Symptoms of asthma include cough, wheezing, shortness of breath, tightness of the chest, and increased mucus production. The exact causes of asthma are unknown. Asthmatic patients are often subdivided into categories based on severity of disease: intermittent, mild persistent, moderate persistent, and severe persistent (Figure 31-3).
Chronic bronchitis is a condition in which chronic irritation causes inflammation and edema with excessive mucus secretion leading to airflow obstruction. Chronic bronchitis refers to a chronic productive cough that is present for 3 months in each of 2 successive years and has no other identifiable cause. Common causes of chronic irritation are cigarette smoke, grain and coal dust exposure, and air pollution. A persistent productive cough present on most days is one of the earliest signs of the disease. The classic patient with chronic bronchitis has a chronic productive cough and moderate dyspnea, is often obese, and suffers from significant hypoxia with cyanosis. The ABGs will confirm hypoxia and respiratory acidosis. This type of patient is often called a “blue bloater.” Because of mucus overproduction and formation of mucus plugs, these patients are prone to recurrent respiratory infections. As this disease progresses, patients often develop polycythemia (increased red blood cell production) to transport oxygen and right-sided heart failure (cor pulmonale) secondary to the lung disease and pulmonary hypertension.
Emphysema is a disease of alveolar tissue destruction without fibrosis. Alveolar sacs lose elasticity and collapse during exhalation, trapping air within the lung. The classic patient with emphysema is dyspneic with minimal exertion (short of breath), breathes through pursed lips, is thin because of weight loss, is barrel-chested from increased use of accessory muscles, and has only scanty sputum production with a minimal cough. These patients are often called “pink puffers” because they maintain normal oxygenation by increasing their breathing rate. Table 31-3 classifies the severity of each stage of COPD based on symptoms and spirometry test results.
Table 31-3
Classification, Characteristics, and Therapies for COPD*
| CHARACTERISTICS | THERAPY | |
| 0: At risk | Chronic symptoms Exposure to risk factors Normal spirometry | Active avoidance of risk factor(s); influenza vaccination |
| GOLD 1: Mild | FEV1/FVC <70% FEV1 ≥80% With or without symptoms | Add short-acting bronchodilator (when needed). |
| GOLD 2: Moderate | FEV1/FVC <70% 50% ≤ FEV1 <80% With or without symptoms | Add regular treatment with one or more long-acting bronchodilators (when needed). Add rehabilitation. |
| GOLD 3: Severe | FEV1/FVC <70% 30% ≤ FEV1 <50% With or without symptoms | Add inhaled glucocorticosteroids if repeated exacerbations. Add roflumilast if repeated exacerbations. |
| GOLD 4: Very severe | FEV1/FVC <70% FEV1 <30% predicted or FEV1 <50% predicted plus chronic respiratory failure | Add long-term oxygen if chronic respiratory failure. Consider surgical treatments. |
*Based on post-bronchodilator FEV1.
Data from the Global Strategy for Diagnosis, Management and Prevention of COPD 2011, Global Initiative for Chronic Obstructive Lung Disease (GOLD). Retrieved from www.goldcopd.org.
Treatment of Lower Respiratory Diseases
Cough
Treatment of the cough is of secondary importance; primary treatment is aimed at the underlying disorder. If the air is dry, a vaporizer or humidifier may be used to liquefy secretions so that they do not become irritating. A dehydrated state thickens respiratory secretions; therefore drinking large amounts of fluids will help reduce secretion viscosity (thickness). Patients can also suck on hard candies to increase saliva flow to coat the throat, thereby reducing irritation. If these simple measures do not reduce the cough, an expectorant or an antitussive (cough suppressant) may be used. The therapeutic objective is to decrease the intensity and frequency of the cough yet permit adequate elimination of tracheobronchial phlegm. In severe cases of pulmonary congestion, a mucolytic agent may be required.
Asthma
The National Heart, Lung, and Blood Institute: National Asthma Education and Prevention Program (NAEPP) has published Guidelines for the Diagnosis and Management of Asthma—Report 3, 2007 (updated 2012), which recommends the following goals of therapy for asthma: maintain normal activity levels; maintain near-normal pulmonary function rates; prevent chronic and troublesome symptoms (e.g., coughing or breathlessness in the night, in the early morning, or after exertion); prevent recurrent exacerbations; minimal use of short-acting inhaled beta2-agonist (<2 days/week); and avoid adverse effects from asthma medications. The guidelines describe four components to asthma therapy—patient education, environmental control, comprehensive pharmacologic therapy, and objective monitoring measures (e.g., regular use of a peak flowmeter). The guidelines also recommend a stepwise approach to asthma therapy for three different age groups, 0 to 4, 5 to 11, and 12 years and older. See Figure 31-3 for an algorithm for the recommended therapy for asthma patients age 12 years and older. Medicines used to treat asthma can be divided into two groups: long-term control medications to achieve and maintain control of persistent asthma and quick-relief medications to treat symptoms and exacerbations. Long-term control medications are the inhaled corticosteroids, cromolyn, long-acting beta-2 agonists, leukotriene modifiers, xanthenes, and immunomodulators. The quick-relief medications are inhaled short-acting beta-2 agonists, inhaled anticholinergic agents, and systemic corticosteroids.
Bronchitis and Emphysema
It is common for patients with obstructive lung disease to have symptoms of more than one of these diseases, but one usually predominates, and overall treatment is similar. According to the Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease, 2011 Update, the goals of effective COPD management are the following:
Management principles include ensuring that the patient understands the disease process, the rationale for various procedures used to treat the disease, and the goals of therapy. Spirometry tests should be completed periodically to assess treatment success. Patients must also be taught appropriate nutrition, exercise, proper coughing techniques, chest percussion and postural drainage to mobilize mucus secretions and plugs, and elimination of risk factors such as smoking, occupational dusts, fumes and gases, and indoor or outdoor pollutants. All these efforts must be balanced with the patient’s perceptions of quality of life.
None of the existing medications for COPD has been shown to modify the long-term decline in lung function associated with obstructive disease. Medicines are used for symptomatic relief and to minimize frequency of complications. Bronchodilators are the cornerstone of chronic obstructive pulmonary disease, but the extent to which they are effective depends on how much reversibility there is to the patient’s airway narrowing. Regularly scheduled treatment with long-acting inhaled bronchodilators is more effective and convenient than treatment with short-acting bronchodilators. Tiotropium, an anticholinergic agent, and the beta-adrenergic agonists are equally effective to start therapy. Oral long-acting theophylline may be added if additional bronchodilation is necessary.
Adding regular treatment with inhaled corticosteroids to bronchodilator treatment is appropriate for symptomatic COPD patients who are classified as having Global Initiative for Chronic Obstructive Lung Disease (GOLD) 3 or GOLD 4 disease. In some patients, such as those with both asthma and COPD, a corticosteroid (e.g., prednisone) may be added for short courses of therapy during an acute exacerbation of asthma or COPD. The phosphodiesterase-4 inhibitor roflumilast may be useful in reducing exacerbations in patients with GOLD 3 or GOLD 4 disease. Long-term treatment with systemic corticosteroids should be avoided. Each of these agents should be used sequentially and the patient reevaluated at each step before a new drug is added. If spirometry tests do not show improvement with a particular agent, it should be discontinued to avoid adverse effects of the medicine. Pulmonary rehabilitation may also be helpful in assisting the patient with COPD by reducing the frequency of exacerbations. The use of antibiotics is not indicated in COPD, other than for treating infectious exacerbations of COPD and other bacterial infections. Vaccination against pneumococcal disease and annual influenza vaccination may reduce the risk of serious infections.
Oxygen therapy may also be used if the patient is chronically hypoxemic, has nocturnal or exercise-induced hypoxemia, or has an acute exacerbation of obstructive disease and the O2 drops below 55 mm Hg. Normal doses for oxygen therapy are 2 to 3 L/min.
Drug Therapy for Lower Respiratory Diseases
Actions and Uses
Expectorants liquefy mucus by stimulating the secretion of natural lubricant fluids from the serous glands. The flow of serous fluids helps liquefy thick mucus masses that may plug the narrow bronchioles. A combination of ciliary action and coughing will then expel the phlegm from the pulmonary system. Expectorants are used to treat nonproductive cough, bronchitis, and pneumonia, in which mucus plugs inhibit the expulsion of irritants and bacteria that cause bronchitis or pneumonia.
Antitussives act by suppressing the cough center in the brain. They are used when the patient has a dry, hacking, nonproductive cough. These agents will not stop the cough completely but should decrease the frequency and suppress the severe spasms that prevent adequate rest at night. Under normal circumstances, it is not appropriate to suppress a productive cough, so antitussives should not be used in patients with a productive cough.
Mucolytic agents reduce the stickiness and viscosity of pulmonary secretions by acting directly on the mucus plugs to cause dissolution. This eases the removal of the secretions by suction, postural drainage, and coughing. Mucolytic agents are most effective in removing mucus plugs obstructing the tracheobronchial airway. They are used in treating patients with acute and chronic pulmonary disorders, before and after bronchoscopy, after chest surgery, and as part of the treatment of tracheostomy care.
Bronchodilators relax the smooth muscle of the tracheobronchial tree. This allows an increase in the opening of the bronchioles and alveolar ducts, which decreases the resistance to airflow into the alveolar sacs. Asthma and bronchitis cause reversible obstruction of the airways. The airway constriction associated with emphysema is somewhat reversible, depending on the severity and duration of the disease. The primary bronchodilators used in the treatment of airway obstructive diseases include beta-adrenergic agents, anticholinergic aerosols, and xanthine derivatives. Combining bronchodilators with a drug that has different mechanisms of action (e.g., combining a long-acting anticholinergic agent with a long-acting beta agonist) and duration of action may increase the degree of bronchodilation and lung function for equivalent or lesser side effects.
Anti-inflammatory agents play an important role in the treatment of asthma to reduce inflammation. Corticosteroids are the most effective agent and the mainstay of all asthma therapy. Most commonly used are those administered by inhalation because this places the medicine at the site of inflammation with minimal systemic adverse effects. Depending on the frequency and severity of acute attacks, some asthmatic patients will require short “bursts” of systemic steroids, usually prednisone, for 1 to 2 weeks of therapy. An occasional patient with asthma may require alternate-day or daily steroid administration to control symptoms. All efforts must be made to optimize other forms of treatment before resorting to regular systemic steroid administration because of the potential serious adverse effects that accompany steroid administration.
Other anti-inflammatory agents used are the leukotriene modifiers, cromolyn and roflumilast. Leukotriene modifiers are a class of anti-inflammatory agents that block leukotriene formation that are part of the inflammatory pathway that causes bronchoconstriction. Cromolyn acts as a mast cell stabilizer, preventing the release of histamines and other chemicals that activate the inflammation cascade. Roflumilast is the first of a new class of agents, the selective phosphodiesterase-4 (PDE4) inhibitors. This agent inhibits the release of inflammatory mediators and inhibits immune-cell activation. None of these anti-inflammatory agents has bronchodilating properties. Omalizumab is the first of a new class of agents, known as immunomodulators, used to treat patients with asthma exacerbations caused by reaction to airborne allergens.
 Nursing Implications for Lower Respiratory Diseases
Nursing Implications for Lower Respiratory Diseases
The nurse must first understand normal respiratory function before proceeding to the assessment of pathophysiologic conditions of the respiratory tract, such as asthma, chronic bronchitis, and emphysema. COPD and CALD are terms that are used interchangeably. Both emphysema and chronic bronchitis are progressive diseases with little reversibility, whereas asthma is an inflammatory process with reversible airflow obstruction.
Assessment
History of Respiratory Symptoms
History of Respiratory Medication
Description of Current Symptoms
Respiratory Assessment.
NOTE: The extent of the pulmonary examination (inspection, palpation, percussion, auscultation) must be adapted to the nurse’s education level and assessment skills (e.g., beginning student, practical nurse, registered nurse).
Rapid shallow breathing may be caused by an elevated diaphragm, restrictive lung disease, or pleuritic chest pain. Rapid deep breathing may be caused by exercise, anxiety, or metabolic acidosis. Kussmaul’s respiration is deep breathing associated with metabolic acidosis. It may be fast, normal, or slow. It is most often found in patients with diabetic ketoacidosis.
Breathing associated with obstructive lung disease has a prolonged expiratory phase because of increased airway resistance. If the respiratory rate increases, the patient lacks time for full expiration. The chest overexpands with trapped air and breathing becomes shallow.
Cheyne-Stokes respiration is a cyclic breathing pattern in which periods of deep breathing alternate with periods of apnea. Children and older people normally show this pattern while asleep. Other causes include heart failure, drug-induced respiratory depression, uremia, and stroke.
Inspection
Palpation.
Perform palpation of the chest, noting any tender or painful areas, masses, and increased or decreased tactile fremitus. Note diminished expansion of the chest wall on inspiration.
Percussion.
Note the presence of dullness, hyperresonance, and diaphragmatic excursion.
Auscultation.
Perform auscultation of the chest; note the intensity, pitch, and relative duration of inspiratory and expiratory phases. Identify additional sounds (e.g., crackles, rhonchi, wheezes). Are they inspiratory, expiratory, or both? Where are they located? Do they clear with deep breathing or coughing? Is bronchophony or egophony present?
Cardiovascular Assessment.
As appropriate to the symptoms and the diagnosis, perform a cardiovascular assessment (see Chapters 24 through 28). Whenever dyspnea is severe, do not overlook the possibility of cardiovascular involvement—perform a cardiac assessment.
Sleep Pattern.
Ask whether the individual has had difficulty sleeping; determine the number of pillows they require. Obtain details.
Psychosocial Assessment.
Ask specifically about the presence and degree of depression, anxiety, and social isolation experienced as a result of the disease process, as well as adaptive or maladaptive responses. Identify support systems in place to assist in providing for the individual’s care.
Laboratory and Diagnostic Data.
Review pulmonary function tests, ABGs, hematology, sputum tests, and x-ray reports as available and appropriate to the diagnosis. Allergy testing may be appropriate for some individuals. If alpha-1 antitrypsin deficiency is suspected, an alpha-1 antitrypsin test and Pi typing may be ordered to determine which type of alpha-1 antitrypsin deficiency is present.
Implementation
 Patient Education and Health Promotion
Patient Education and Health Promotion
Peak Flowmeter.
People with asthma are routinely taught how to use a peak flowmeter to measure the peak expiratory flow (PEF) to assess the severity of their symptoms. The following can be determined using the PEF as a guide:
Avoiding Irritants.
Smoking, pollen, and environmental pollutants commonly aggravate respiratory disorders. Check the home and work environment for allergens that may be precipitating or worsening an asthmatic attack. Medicines alone will not alleviate the problem. The control of triggers for the attacks is of paramount importance.
Activity and Exercise
Nutritional Status
Preventing Infections
Increased Fluid Intake.
Unless contraindicated, encourage patients to increase fluid intake. This will aid in decreasing secretion viscosity. Patients should drink eight to ten (or more) 8-ounce glasses of water daily as directed by the health care provider.
Environmental Elements.
People experiencing difficulty in breathing can benefit from proper temperature, humidification of the air, or ventilation of the immediate surroundings. Moist air from a humidifier can readily relieve nose or throat dryness.
Breathing Techniques.
If ordered by the health care provider, teach postural drainage and pursed-lip breathing or abdominal breathing and coughing; referrals to pulmonary rehabilitation may be indicated. Record peak flow readings, and institute prescribed treatments as indicated by the health care provider.
Sleep Patterns.
Discuss adaptations that the individual can make in daily routines to ensure adequate rest. As the disease progresses, sleeping in a recliner or in an upright position may be necessary.
Psychosocial Behavior
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 packs of cigarettes per day for 20 years, the patient is said to have a
packs of cigarettes per day for 20 years, the patient is said to have a  , 30 pack-year history of smoking.)
, 30 pack-year history of smoking.)