CHAPTER 30. Respiratory Emergencies
Paula Works and Sharon A Graunke
This chapter will discuss the basic anatomy and physiology of the respiratory system, as well as frequent respiratory emergencies that occur in the adult population, including asthma, bronchitis, emphysema, pulmonary edema, pulmonary embolus, near-drowning, and spontaneous pneumothorax. Epiglottitis, bronchiolitis, and other respiratory emergencies seen more frequently in the pediatric population will be addressed in Chapter 47.
ANATOMY AND PHYSIOLOGY
The respiratory system can be divided into two parts: the upper airway and the lower airway. The upper airway includes the nasopharynx, oropharynx, and laryngopharynx. The structures within the upper airway are supported by cartilaginous rings to prevent collapse during respiration. Cartilaginous rings are replaced with smooth muscle fibers in the lower airways for stability and support. Connecting the upper and lower airways is the larynx, which acts as a gate to prevent aspiration. The lower airway comprises the larynx, trachea, bronchi, bronchioles, and alveoli. The functional unit of the pulmonary system is the alveolus, which interacts with adjacent capillaries to ensure oxygen transport from alveolus into blood.
Within the pleural cavity there is a negative intrathoracic pressure, which causes a vacuum effect, pulling air into the lungs during inspiration. During expiration, this negative pressure decreases and the air is passively expelled. During inspiration, air is filtered, warmed, and humidified as it travels through the upper and lower airways. Cilia, hairlike structures within the passageways, help to move air toward the alveoli. Cilia also help to move mucus and debris out of the pulmonary system, keeping the lower airways from being contaminated. The sterility of the lower airway is achieved with the help of mucus-secreting goblet cells. Mucus traps debris and keeps the airway moist. Gas exchange occurs in the alveoli and pulmonary capillaries. Oxygen and carbon dioxide are exchanged at this cellular level.
Cellular oxygenation is dependent upon several factors: (1) an adequate supply of oxygen carried to the cell, (2) the affinity of hemoglobin for oxygen, and (3) the ease with which hemoglobin releases oxygen to cells. The affinity of hemoglobin for oxygen is described by the oxygen-hemoglobin dissociation curve. If the curve shifts to the left, hemoglobin picks up oxygen more easily in the lungs but does not easily release oxygen to tissues. When the curve shifts to the right, oxygen uptake by hemoglobin is less rapid, but oxygen delivery to cells is easier. Oxygen dissociation is affected by temperature, acid-base balance, and carbon dioxide pressure (PCO 2) levels.
Normal gas exchange depends on adequate ventilation and perfusion. Respiration is divided into pulmonary ventilation, diffusion of oxygen and carbon dioxide across the alveolar capillary membrane, transport of oxygen and carbon dioxide to and from the cells, and regulation of ventilation. Ventilation refers to the mechanical flow of air into and out of the lungs. Respiration is the actual exchange of oxygen and carbon dioxide at the cellular level. Diffusion is a process in which particles in a fluid move from an area of higher concentration to an area of lower concentration, resulting in an even distribution of particles in the fluid. Perfusion relates to the transport of blood to the tissues. Ventilation/perfusion (V/Q) mismatch occurs when either ventilation or perfusion is inadequate. When there is an extreme imbalance, inadequately oxygenated blood is shunted into the arterial system.
PATIENT ASSESSMENT
When assessing a patient with a respiratory emergency, begin with airway patency. The patient must have a patent airway before proceeding. Once patency has been established, assess the patient’s work of breathing, looking for nasal flaring, retractions, accessory muscle use, tracheal tugging, or dyspnea. Be alert to other signs of distress, including abnormal color such as pallor or cyanosis, grunting, difficulty speaking in complete sentences, tripod positioning, or decreased mental status. Changes in the patient’s mental status can be an early warning sign of deterioration. Once airway, breathing, and circulation have been assessed, then perform a quick head-to-toe assessment. Listen for adventitious breath sounds, and obtain a full set of vital signs. While performing the assessment, observe the patient’s appearance. Physical characteristics such as a barrel chest and club fingers are often associated with chronic obstructive pulmonary disease (COPD). Although these findings can be normal in some patients, they can also indicate cardiovascular abnormalities, valvular heart disease, or congenital defects.
The patient history should include when the symptoms began, what occurred just before the event, history of similar episodes, past medical history, any treatments that have been used before arrival, smoking history, orthopnea, and nocturnal dyspnea. Not every patient will be able to provide a history because of his or her degree of breathing difficulty. Observe for silent clues such as use of accessory muscles or leaning over a bedside table. While obtaining the history, inquire about occupational hazards the patient may have been exposed to such as asbestos, beryllium dust, bird droppings, coal dust, iron oxide, or silica dust. These agents are associated with the following lung diseases, respectively, asbestosis, berylliosis, bird handler’s lung, black lung, siderosis, and silicosis.
If the patient smokes, determine how much the patient smokes and how long he or she has been smoking. Smoking decreases lung compliance because it damages the elastin and collagen fibers. Patients who smoke usually have a decreased sense of taste and smell along with increased secretions and cough. Cigarette smoke negatively affects the functions within the pulmonary system that are used to keep it clear. Smoking increases the likelihood of cancer, chronic bronchitis, emphysema, and the incidence of infection.
Patients who present with respiratory emergencies should be placed on a bedside monitor for continuous monitoring of oxygen saturation, cardiac rhythm, and vital signs. The patient’s oxygen saturation will often be decreased in respiratory emergencies. Always treat the patient—do not rely simply on a number on the bedside monitor. Many factors (e.g., artificial fingernails, nail polish, and cold extremities) can skew the numbers displayed on the bedside monitor. If the patient is having difficulty breathing, administer oxygen using the device (e.g., nasal canula, nonrebreather, bag-mask device) that is most appropriate for the situation. Chest radiograph, complete blood count (CBC), and arterial blood gas (ABG) levels should be obtained.
SPECIFIC PULMONARY EMERGENCIES
Acute Bronchitis
Acute bronchitis is an inflammatory process that is usually caused by a virus. Some of the common offenders include influenza virus A or B, parainfluenza virus, respiratory syncytial virus, rhinovirus, Coxsackie virus, and adenovirus. 1 Acute bronchitis is more common during cold and flu season and does not have age boundaries. Secondary infections are possible from organisms such as Mycoplasma pneumoniae, Haemophilus influenzae, pneumococci, and streptococci. The highest incidence of acute bronchitis occurs in smokers, older adults, young children, and during the winter months. Patients complain of sore throat, stuffy nose, and cough. Initially the cough will be dry and nonproductive and may worsen at night. Aggravating factors include exposure to cold, talking, deep breathing, and laughing. After a few days the patient’s cough usually becomes productive. Other symptoms can include low-grade fever, chest discomfort, and fatigue.
Diagnosis is based on the clinical presentation. Chest radiograph is needed to distinguish between acute bronchitis and pneumonia. Treatment of acute bronchitis includes increasing fluid intake, avoiding smoke or other irritants, cough preparations, and using a vaporizer to add moisture to the air. Antibiotics are not helpful except for secondary infections.
Pneumonia
Pneumonia is an inflammatory reaction usually caused by an acute bacterial, viral, or fungal infection. It may be preceded by an upper respiratory tract infection, ear infection, or eye infection. Pneumonia occurs primarily in young children, debilitated individuals, and those with an underlying chronic disease. It is the leading cause of death among older adults4 and is the sixth leading cause of death in the United States. 1
There are certain conditions that may lead to recurrent cases of pneumonia, including underlying cardiac or pulmonary disorder, compromised immune function, cystic fibrosis, esophageal abnormalities, bronchial obstruction, and bronchiectasis. 1 Patients who are immobile or bedridden and patients with rib fractures are at an increased risk. Other risk factors for pneumonia include smoking, steroids, immunosuppressive therapy, diabetes mellitus, and exposure to extreme changes in environmental temperature.
Patients present with complaints of fever, malaise, cough, hemoptysis, dyspnea, and pleuritic chest symptoms. On physical examination the patient will have crackles that do not clear with coughing, as well as consolidation. Older adult patients may not exhibit the classic symptoms of pneumonia. Instead, these patients may have a sudden mental status change. 1 Some patients with pneumonia experience abdominal distension, vomiting, and headache.
Treatment for patients with pneumonia includes humidified oxygen, antibiotics, and monitoring of fluid and electrolyte balance. Diagnostic assessment includes sputum culture and Gram stain, chest radiograph, and CBC. Pulse oximetry is obtained initially and monitored over time to determine changes in the patient’s oxygenation. ABG values may be obtained as a baseline. Teaching should include the importance of pneumonia vaccinations to reduce the likelihood of future occurrences, as well as flu shots. Smoking cessation information should also be provided.
Hospital Core Measures for patients with community-acquired pneumonia (CAP) have been created by The Joint Commission as a means to improve patient outcome. 10 Each year, close to 3 million cases of CAP lead to physician visits, hospitalizations, and death. 10Streptococcus pneumoniae is one of the leading infectious causes of illness and death for young children, those with chronic conditions, and older adults. Patients who present to the ED with symptoms suggestive of pneumonia need to have an oxygen assessment either via pulse oximetry or ABG measurement. Most often pulse oximetry is used because it is less invasive and more cost-effective. During triage the patient’s pneumococcal vaccination and smoking history should be determined. Smoking cessation information should be provided to all patients with a smoking history. Blood cultures should be performed on all patients admitted with CAP before the first antibiotic dose, although this is still controversial. Antibiotic administration should not be delayed for blood cultures. Through the implementation of these core measures it has been found that those patients with CAP who receive antibiotics within 4 hours of arrival to the hospital have improved hospital course and 30-day mortality. 10
Asthma
Asthma is an obstructive disease of the lungs characterized by airway inflammation and hyperreactivity. Symptoms can range from mild to severe. Asthma can be controlled, not cured, and has an unpredictable course with increasing prevalence and hospitalizations. The majority of asthmatic patients are children with males being affected more than females. Thirty percent of those diagnosed with asthma during childhood will have it as adults. There is positive family history in more than one third of asthmatic patients. 3
Airway inflammation and hyperresponsiveness occur in response to certain triggers (Box 30-1). Immunologic triggers cause a humoral immune response with complex multicellular activation, including mast cells, eosinophils, and immunoglobulin E (IgE) antibodies (Figure 30-1). Inflammatory mediators cause smooth muscle contraction, vasodilation, mucosal edema, increased mucus secretion, and macrophage eosinophil infiltration. Acetylcholine directly increases airway resistance and bronchial secretions. This cholinergic response further stimulates histamine and inflammatory mediator release, with the exception of IgE.
Box 30-1
T riggers of A cute A sthma A ttacks
Allergen inhalation
Animal dander
House dust mite
Pollens
Molds
Air pollutants
Exhaust fumes
Perfumes
Oxidants
Sulfur dioxides
Cigarette smoke
Aerosol sprays
Viral upper respiratory infection
Sinusitis
Exercise and cold, dry air
Stress
Drugs
Aspirin
Nonsteroidal antiinflammatory drugs
β-Adrenergic blockers
Occupational exposure
Metal salts
Wood and vegetable dusts
Industrial chemicals and plastics
Pharmaceutical agents
Food additives
Sulfites (bisulfites and metabisulfites)
Beer, wine, dried fruit, shrimp, processed potatoes
Monosodium glutamate
Tartrazine
Hormonesmenses
Gastroesophageal reflux
Emotional stress
From Lewis SM, Heitkemper MM, Dirksen SR: Medical-surgical nursing: assessment and management of clinical problems, ed 7, St. Louis, 2007, Mosby.
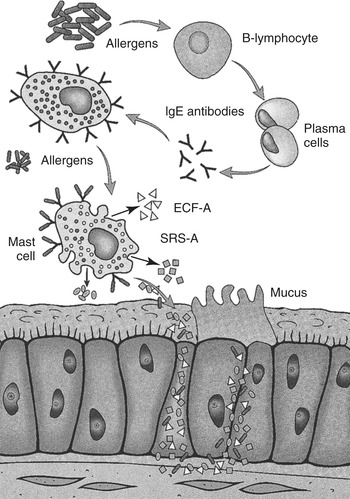 |
| FIGURE 30-1 Early-phase response in asthma is triggered when an allergen or irritant cross-links immunoglobulin E receptors on mast cells, which are then activated to release histamine and other inflammatory mediators. ECF-A, Eosinophil chemotactic factor of anaphylaxis; IgE, immunoglobulin E; SRS-A, slow-reacting substance of anaphylaxis. (From Lewis SL, Heitkemper MM, Dirksen SR et al: Medical-surgical nursing: assessment and management of clinical problems, ed 7, St. Louis, 2007, Mosby.) |
Nonimmunologic triggers stimulate the autonomic nervous system and cause mast cell and inflammatory mediator response. The pathway of emotional triggers is through the parasympathetic nervous system and stimulation of the hypothalamus. Aspirin sensitivity exacerbates asthma through reaction to prostaglandin synthesis. Exercise-induced asthma occurs after 10 to 20 minutes of vigorous exercise because of airway cooling secondary to decreased warming, reduced humidification, and increased respiratory rates. Exercise may be the only trigger for some patients and is usually limited to the early phase. Gastroesophageal (GE) reflux, a common condition associated with asthma, involves esophageal spasm with reflux of gastric acid causing spasm of nearby bronchial and esophageal structures.
Immunologic and nonimmunologic triggers cause increased mucus production, airway hyperresponsiveness, airway narrowing, and chronic inflammatory airway changes. These triggers can cause either an early or late response in asthmatic patients. Early-phase reactions involve rapid bronchospasms, whereas late-phase reactions involve inflammatory epithelial lesions, increased mucosal edema, and increased secretions. Complex interactions among lung cells cause a chronic inflammatory process that irritates airways. An acute exacerbation involves airway obstruction caused by spasms, inflammation, and mucus plugging.
There are no definitive tests to diagnose asthma. The diagnosis should be based on careful history, examination, and laboratory studies. The history should include symptoms, patterns, usual triggers, family history, and allergies the patient may have. Physical examination may reveal upper airway rhinitis, sinusitis, or nasal polyps, as well as wheezes and prolonged expiratory phase. Laboratory studies should include CBC with differential, nasal smears, and sputum specimen. The CBC may have elevated eosinophils. There may be increased hilar or basilar infiltrates or areas of atelectasis secondary to mucus plugging and alveolar collapse on chest radiographs. To aid in the diagnosis of asthma, patients over the age of 5 years should have spirometry, which evaluates the air capacity of the lungs using a spirometer and measures the volume of air inhaled and exhaled. Spirometry can demonstrate obstruction and assess reversibility of airway narrowing. Peak expiratory flow rate (PEFR) is the greatest flow velocity produced during forced expiration after fully expanding lungs during inspiration. It is measured using a peak flowmeter. PEFR is used to monitor response to therapy in acute episodes but is not designed as a diagnostic tool. 8 PEFR measurement is effort dependent, so the results need to be duplicated.
The 2007 National Asthma Education and Prevention Program (NAEPP) Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma expanded the 2002 guidelines and recommended some updates based on new evidence. There are new focus areas for monitoring asthma control and looking at impairment (i.e., the frequency and intensity of symptoms) and risk (i.e., the likelihood of exacerbations, progressive decline in lung function, or risk for adverse effects from the medication). There is a modification to the stepwise approach to long-term asthma management focusing on different age-groups. There is a new emphasis on patient education and control of environmental factors or comorbid conditions that affect asthma. There are also modifications to treatment strategies for managing asthma exacerbations, which include the following: simplifying the classification of severity of exacerbations; encouraging the development of prehospital protocols to allow administration of albuterol, oxygen, and with medical oversight, anticholinergics and oral systemic corticosteroids; adding levalbuterol; adding magnesium sulfate or heliox for severe exacerbations unresponsive to initial treatment; emphasizing oral corticosteroids; emphasizing that anticholinergics are used in emergency care, not hospital care; and considering initiation of inhaled corticosteroids at discharge. 7
Inhaled allergens are common triggers, particularly for patients less than 30 years of age. For patients who have persistent asthma, skin testing to assess sensitivity to indoor allergens is recommended. 7 Although patients may have positive skin reactions to food allergens, these usually do not lead to acute exacerbations. In addition to inhaled allergens, other triggers such as occupational exposures, viral illnesses, and GE reflux can stimulate an asthma attack. Gastroesophageal reflux disease (GERD) is associated with nocturnal exacerbations that do not respond well to inhaled nebulizers. When GERD is suspected, a thorough gastrointestinal workup is indicated.
Occupational asthma initially presents with rhinitis or eye irritation along with evening or nocturnal cough. With prolonged exposure the patient will note increased symptoms, such as coughing, wheezing, and dyspnea. These symptoms will diminish with time away from exposure to irritants. Smokers have a higher incidence of occupational asthma because of increased airway irritation.
Clinical manifestations of asthma include cough, wheezing, prolonged expiratory time, and reduced peak expiratory flow. Patients may also experience increased work of breathing and accessory muscle use. When a patient presents to the ED with decreased air movement, low oxygen saturation, altered level of consciousness, and increased work of breathing, immediate interventions are required. These patients require high-flow oxygen and continuous pulse oximetry, along with nebulizer therapy, in an effort to provide some relief of symptoms. Close observation is required because their symptoms can lead to respiratory failure if rapid interventions are not provided. Severity can be assessed by determining type and frequency of home medications required to control symptoms, prior intubation, recent hospitalizations, spirometric indexes of air flow obstruction, nocturnal symptoms, and number of prior ED visits. ABG values initially indicate reduced arterial oxygen pressure (PaO 2) and arterial carbon dioxide pressure (PaCO 2) from hyperventilation. PaCO 2 eventually rises, which creates further V/Q mismatching.
Management goals are to maintain near-normal pulmonary function and exercise levels, prevent chronic symptoms and acute exacerbations, and avoid adverse effects of medications. Therapy includes objective measurement of lung function, environmental control, avoidance of triggers, select drugs, and comprehensive patient education.
PEFR provides objective data for management, documents personal best and daily variations, detects impending exacerbation, guides medicine therapy, and helps identify triggers. To correctly obtain peak expiratory flow measurements the patient should stand, if able, take a deep breath, and forcefully blow out all inspired air. The highest of three readings is recorded. A diary of peak expiratory flow measurements, along with documentation of viral infections, weather, medicine changes, environments, and other possible triggers aids in management of asthma.
Avoidance and environmental control of allergens such as dust mite antigens, animal dander, pollens, and molds can greatly reduce symptoms. Encasing pillows and mattresses in dust mite–proof covers, washing bedding every week in water temperatures greater than 130° F, and carpet removal or antimite treatment aid in the reduction of dust mites. Keep pets outside the house to decrease dander allergens, outdoor pollens, and mold. Asthma patients should remain inside with air conditioning during early morning and midday hours to further reduce exposure.
Drugs for asthma reduce bronchial spasms, airway inflammation, mucosal edema, and airway hyperreactivity. These medications can be given orally, intravenously, subcutaneously, or inhaled. There are several forms of inhaled therapy, such as nebulizers and inhalers (Table 30-1). Advantages of inhaled therapy include smaller drug amounts, rapid onset of action, direct delivery to respiratory system, fewer side effects, and painless, convenient administration.
| CFC, Chlorofluorocarbon; CNS, central nervous system; HFA, hydrofluoroalkane (an environmentally friendly propellant); IM, intramuscular; IV, intravenous; PSNS, parasympathetic nervous system. | |||
| Medication | Actions | Strength/Dosage (Adults) | Side Effects/Comments/Precautions |
|---|---|---|---|
| BRONCHODILATORS | Stimulate β-receptors for bronchodilation | ||
| Epinephrine (Adrenalin, Primatene Mist) | As above | IM or subcutaneous: 0.2-1 mg (0.2-1 mL) of 1:1,000 solution; may repeat every 20 min (maximum three doses)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree

Get Clinical Tree app for offline access

| |