Intrapartum
Basic Definitions
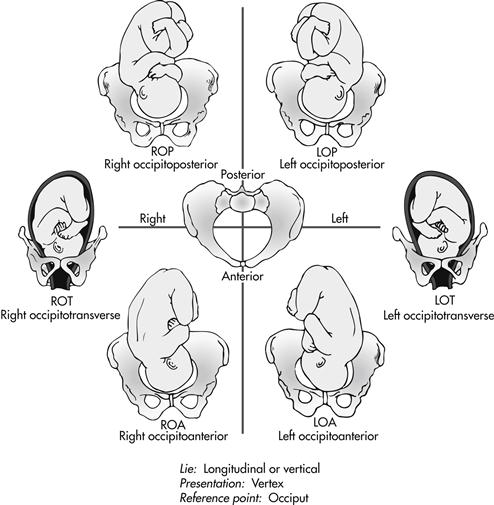
position: relationship of a reference point on the presenting part of the fetus, such as the occiput, sacrum, chin, or scapula, to its location in the front, back, or sides of the maternal pelvis (Fig. 3-1)
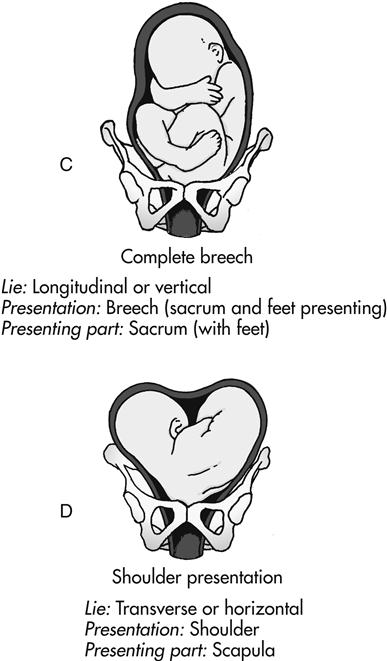
presentation: that part of the fetus that first enters the pelvis and lies over the inlet; the three main presentations are cephalic (head first), breech (buttocks or feet first), and shoulder (Fig. 3-2)
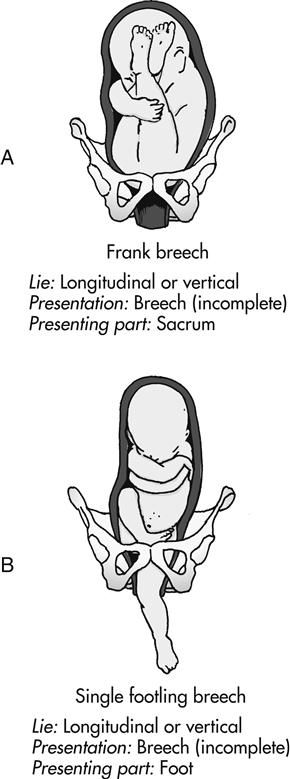
station: relationship of the presenting fetal part to an imaginary line drawn between the maternal ischial spines; a measure of the degree of descent of the presenting part of the fetus through the birth canal; the placement of the presenting part is measured in centimeters above or below the ischial spines (Fig. 3-3)
Stages of Labor
The length of the first stage of labor varies greatly but is usually shorter as parity increases. Full dilation may occur in less than 1 hour in some multiparous pregnancies. In first-time pregnancy, complete dilation of the cervix can take up to 20 hours.
The second stage of labor lasts an average of 20 minutes for a multiparous woman and 50 minutes for a nulliparous woman.
Management of the First Stage of Labor
Admission to the Labor and Birth Unit
 Use the agency’s triage and/or admission forms (may be paper or electronic) as a guide for obtaining important assessment information. These forms usually address:
Use the agency’s triage and/or admission forms (may be paper or electronic) as a guide for obtaining important assessment information. These forms usually address:
 Chief complaint: “Why did you come at this time?”
Chief complaint: “Why did you come at this time?”
 Contraction status (time of onset, frequency, duration, intensity, resting tone)
Contraction status (time of onset, frequency, duration, intensity, resting tone)
 Fetal heart rate (FHR) and pattern
Fetal heart rate (FHR) and pattern
 Presence and character of vaginal discharge or show
Presence and character of vaginal discharge or show
 Vaginal examination to determine cervical effacement, dilation, and fetal station
Vaginal examination to determine cervical effacement, dilation, and fetal station
 Perform basic laboratory and diagnostic tests according to hospital protocol. These commonly include the following:
Perform basic laboratory and diagnostic tests according to hospital protocol. These commonly include the following:
 Rapid group B streptococci (GBS) test (if third-trimester test results are not available)
Rapid group B streptococci (GBS) test (if third-trimester test results are not available)
 Rapid human immunodeficiency virus (HIV) test (if third-trimester test results are not available)
Rapid human immunodeficiency virus (HIV) test (if third-trimester test results are not available)
 Review the prenatal record to determine the following:
Review the prenatal record to determine the following:
 Problems during the current pregnancy
Problems during the current pregnancy
 Laboratory and/or diagnostic test results
Laboratory and/or diagnostic test results
 Type of childbirth preparation
Type of childbirth preparation
 Determine if the woman is in true labor. See Box 3-1 for differences in true and false labor.
Determine if the woman is in true labor. See Box 3-1 for differences in true and false labor.
Common Characteristics of the First Stage of Labor
Common appearance and behavior of women during each phase of the first stage of labor are listed in Box 3-2.
Nursing Care in the First Stage of Labor
Nursing care for women during the first stage of labor is described in Box 3-3.
Fetal Assessment During Labor
Because labor is a period of physiologic stress for the fetus, frequent monitoring of fetal status is part of the nursing care during labor. The goals of intrapartum FHR monitoring are to identify and differentiate the normal (reassuring) patterns from the abnormal (nonreassuring) patterns, which can be indicative of fetal compromise. Fetal well-being during labor can be assessed by the response of the FHR to uterine contractions.
Monitoring Techniques
Intermittent Auscultation (IA)
 Uses listening to fetal heart sounds at periodic intervals to assess the FHR
Uses listening to fetal heart sounds at periodic intervals to assess the FHR
 Box 3-4 describes how to perform IA.
Box 3-4 describes how to perform IA.
Uterine Activity (UA) Assessment
Electronic Fetal Monitoring (EFM)
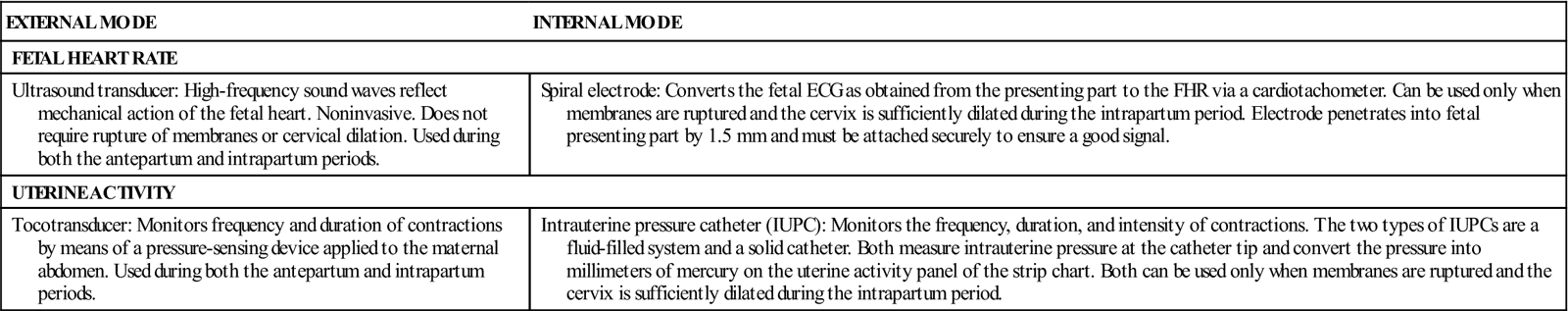
There are two modes of electronic FHR and contraction monitoring: external and internal. See Table 3-1 for differences in these monitoring modes.
TABLE 3-1
External and Internal Modes of Monitoring
| EXTERNAL MODE | INTERNAL MODE |
| FETAL HEART RATE | |
| Ultrasound transducer: High-frequency sound waves reflect mechanical action of the fetal heart. Noninvasive. Does not require rupture of membranes or cervical dilation. Used during both the antepartum and intrapartum periods. | Spiral electrode: Converts the fetal ECG as obtained from the presenting part to the FHR via a cardiotachometer. Can be used only when membranes are ruptured and the cervix is sufficiently dilated during the intrapartum period. Electrode penetrates into fetal presenting part by 1.5 mm and must be attached securely to ensure a good signal. |
| UTERINE ACTIVITY | |
| Tocotransducer: Monitors frequency and duration of contractions by means of a pressure-sensing device applied to the maternal abdomen. Used during both the antepartum and intrapartum periods. | Intrauterine pressure catheter (IUPC): Monitors the frequency, duration, and intensity of contractions. The two types of IUPCs are a fluid-filled system and a solid catheter. Both measure intrauterine pressure at the catheter tip and convert the pressure into millimeters of mercury on the uterine activity panel of the strip chart. Both can be used only when membranes are ruptured and the cervix is sufficiently dilated during the intrapartum period. |
Standardized Definitions for FHR Monitoring
Baseline Patterns
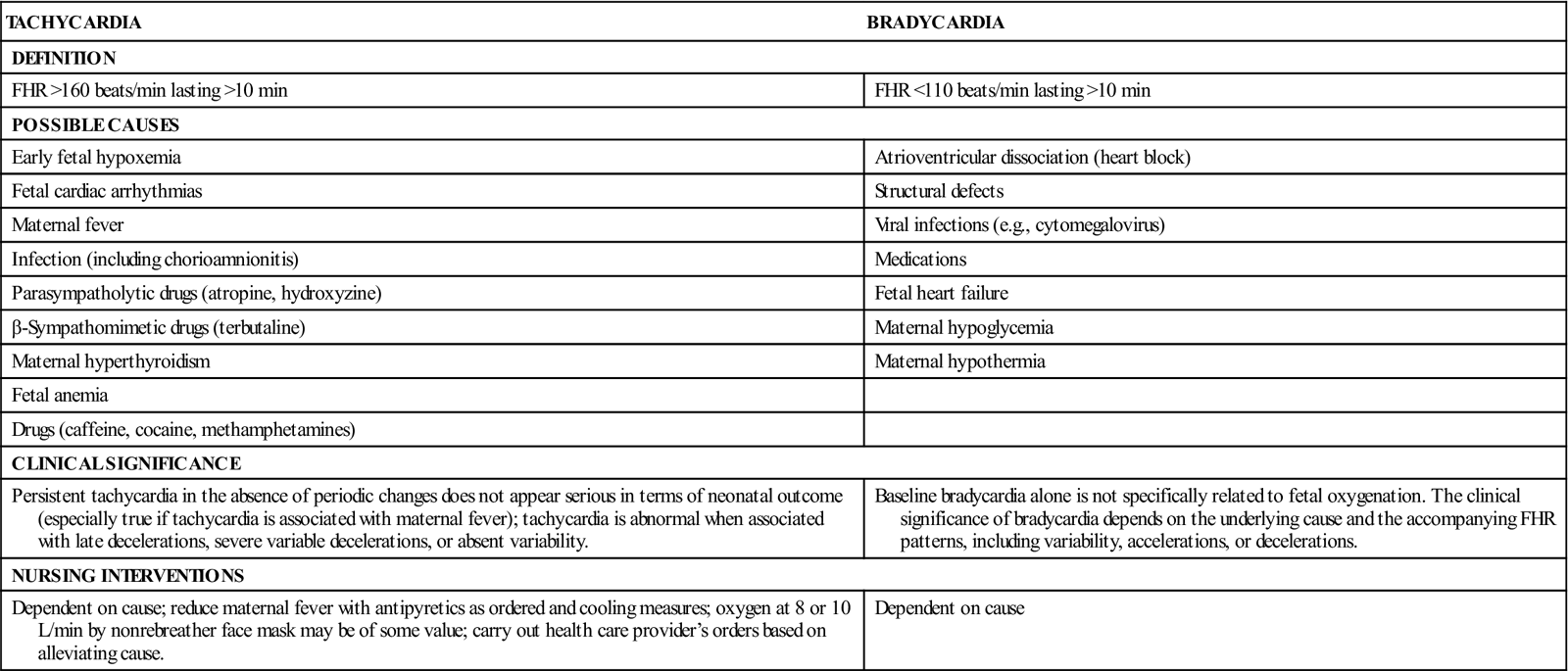
Bradycardia: baseline FHR less than 110 beats/min and lasting for 10 minutes or longer
Tachycardia: baseline FHR more than 160 beats/min and lasting for 10 minutes or longer
Causes, clinical significance, and nursing interventions for tachycardia and bradycardia are listed in Table 3-2.
TABLE 3-2
| TACHYCARDIA | BRADYCARDIA |
| DEFINITION | |
| FHR >160 beats/min lasting >10 min | FHR <110 beats/min lasting >10 min |
| POSSIBLE CAUSES | |
| Early fetal hypoxemia | Atrioventricular dissociation (heart block) |
| Fetal cardiac arrhythmias | Structural defects |
| Maternal fever | Viral infections (e.g., cytomegalovirus) |
| Infection (including chorioamnionitis) | Medications |
| Parasympatholytic drugs (atropine, hydroxyzine) | Fetal heart failure |
| β-Sympathomimetic drugs (terbutaline) | Maternal hypoglycemia |
| Maternal hyperthyroidism | Maternal hypothermia |
| Fetal anemia | |
| Drugs (caffeine, cocaine, methamphetamines) | |
| CLINICAL SIGNIFICANCE | |
| Persistent tachycardia in the absence of periodic changes does not appear serious in terms of neonatal outcome (especially true if tachycardia is associated with maternal fever); tachycardia is abnormal when associated with late decelerations, severe variable decelerations, or absent variability. | Baseline bradycardia alone is not specifically related to fetal oxygenation. The clinical significance of bradycardia depends on the underlying cause and the accompanying FHR patterns, including variability, accelerations, or decelerations. |
| NURSING INTERVENTIONS | |
| Dependent on cause; reduce maternal fever with antipyretics as ordered and cooling measures; oxygen at 8 or 10 L/min by nonrebreather face mask may be of some value; carry out health care provider’s orders based on alleviating cause. | Dependent on cause |
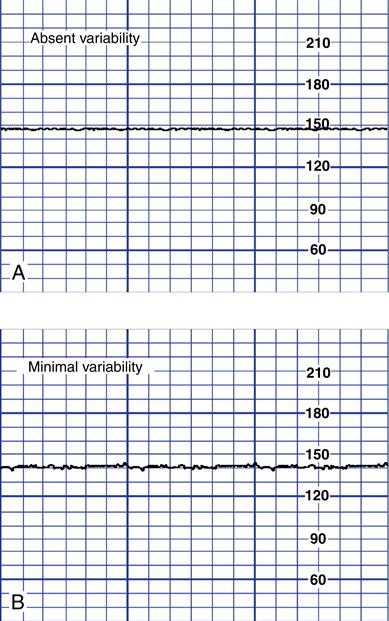
FHR variability: normal irregularity of fetal cardiac rhythm or fluctuations from the baseline FHR of two cycles or more; the four possible categories of variability are absent, minimal, moderate, and marked. Figure 3-4 shows the four possible categories of variability.
Periodic and Episodic Patterns
Figure 3-5 shows an example of accelerations. Box 3-5 lists causes, clinical significance, and nursing interventions for accelerations.
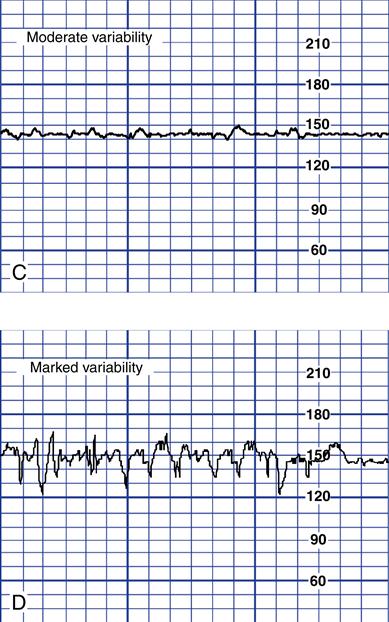
Figure 3-6 shows an example of early decelerations. Box 3-6 lists causes, clinical significance, and nursing interventions for early decelerations.
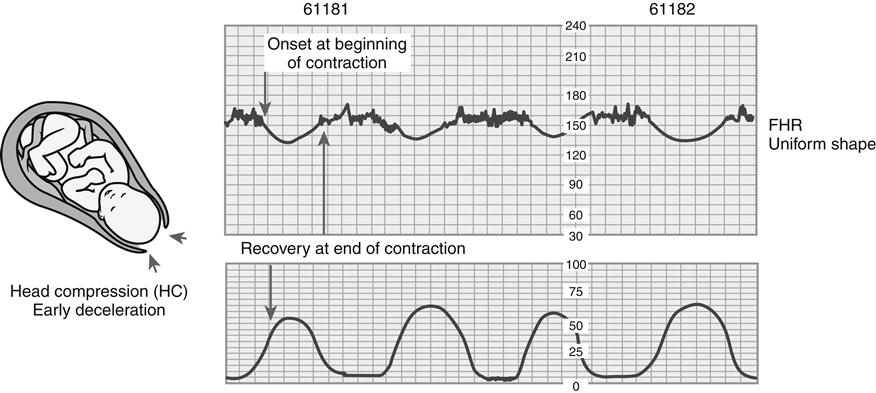
Figure 3-7 shows an example of late decelerations. Box 3-7 lists causes, clinical significance, and nursing interventions for late decelerations.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree