CHAPTER 29. Obstetric Trauma
Terri McGowan Repasky
The actual incidence of obstetric trauma is unknown, but it has been estimated that injuries occur in 6% to 7% of all pregnancies. 5 Trauma is the leading cause of maternal death from nonobstetric causes for women during their childbearing years. Most obstetric trauma involves minor injury, although significant trauma-related injuries can occur. Nursing priorities for the pregnant and nonpregnant trauma patient are the same, but interventions are intended to benefit two patients, the mother and the fetus.
Like their nonpregnant counterparts, pregnant patients sustain blunt, penetrating, burn, and submersion injuries. Blunt trauma is the most common, often due to motor vehicle crashes (MVCs), falls, and assaults. 5 Trauma secondary to battering is more common in pregnant patients. During the first 4 months of pregnancy 154 per 1000 women are assaulted by their partners. During the fifth through ninth month 170 per 1000 are assaulted. 4 Overexertion may also lead to injuries during pregnancy. 6
Most maternal deaths from trauma are secondary to head injury or hemorrhagic shock. Pelvic fracture is the most common maternal injury that results in fetal death. Abruptio placentae and premature delivery are the most common trauma-related causes of fetal demise.
Primary and secondary assessment and initial nursing priorities for the pregnant trauma patient are essentially the same as for a nonpregnant patient. However, anatomic and physiologic differences related to the gravid state must be considered during all stages of the trauma nursing process.
ANATOMY AND PHYSIOLOGY
Normal respiratory and circulatory changes during pregnancy can mask the typical signs and symptoms that emergency nurses rely on to guide care of their trauma patient. Optimal outcome for mother and fetus is based on sound knowledge of maternal anatomy and physiology and implications for interventions.
Uterine
Uterine size and blood flow are a concern in the gravid trauma patient. The uterus enlarges from a 7-cm and 70-g structure to a 36-cm and 1100-g walled organ (similar in size and weight to a bowling ball). As the uterus grows, its wall becomes thinner. Through the first 12 weeks of pregnancy the uterus remains a small, self-contained intrapelvic organ protected from abdominal injury by the bony pelvis. After 12 weeks the uterus becomes an intraabdominal organ as it enlarges and ascends, encroaching on the peritoneal cavity and confining the intestines to the upper abdomen. Figure 29-1 shows uterine size for various gestational periods. During the second trimester the uterus is susceptible to abdominal injury, although the fetus remains small and relatively cushioned by large amounts of amniotic fluid. By the third trimester the uterus is large and thin walled. During the last 2 to 8 weeks’ gestation, the fetus descends and the fetal head engages in the pelvis. The fetus occupies most of the intrauterine and abdominal space when the head becomes fixed in the pelvis. Maternal pelvic fractures during this trimester may be associated with fetal skull fractures and intracranial hemorrhage, as well as significant maternal blood loss.
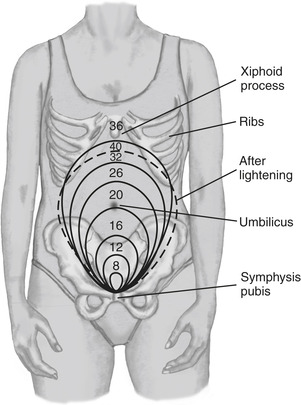 |
| FIGURE 29-1 Uterine growth patterns during pregnancy. (From Murray SS, McKinney ES: Foundations of maternal-newborn nursing, ed 4, Philadelphia, 2006, WB Saunders.) |
Uterine blood flow increases from a baseline of 60 mL/min to 600 mL/min during the third trimester. Uterine blood flow has no autoregulation and depends solely on maternal perfusion pressure. Uterine veins may dilate up to 60 times their prepregnant state; uterine injury may be a major source of blood loss. In response to trauma, maternal catecholamines are released by the sympathetic nervous system and cause uteroplacental constriction, which shunts blood to the mother and away from the fetus and leads to fetal distress. By the third trimester, vessels of the uterus and placenta have reached maximum vasodilatation and cannot increase blood flow in response to decreased perfusion.
Cardiovascular
Anatomically, the heart is elevated and rotated forward by the ascending diaphragm and pushed up by the enlarging uterus. This cardiac displacement causes a 15-degree left axis deviation that is considered a normal change of pregnancy. An electrocardiogram may also show a flattened or inverted T wave in lead III and Q waves in III and aVF. Ectopic beats are also common during pregnancy.
Cardiovascular physiology is profoundly altered during pregnancy. Maternal blood volume increases by the tenth week of gestation and increases 40% to 50% by the twenty-eighth week, remaining at that level until delivery. Uterine blood flow increases to 600 mL/min by the end of pregnancy. Increased blood flow and volume increase maternal cardiac output by 1 to 1.5 L/min. After approximately 20 weeks’ gestation, cardiac output can decrease with compression of the vena cava and aorta by the fetus when the mother is in a supine position. This event is called inferior vena cava syndrome or supine hypotensive syndrome. Because the uterus at 20 weeks has grown and risen to the level of the inferior vena cava, compression of the vena cava by the uterus may decrease cardiac output by 28% and systolic blood pressure by 30 mm Hg. Sequestering blood in the venous system may decrease perfusion to the uterus; when maternal systolic blood pressure is below 80 mm Hg, the uterus and fetus will not be perfused. Displacing the gravid uterus to the side by placing the pregnant patient in a lateral decubitus position or manual displacement reverses aortocaval compression. When spinal injury is suspected, maintain spinal protection and tilt the patient 15 degrees laterally or manually displace the uterus.
Resting heart rate increases until the second trimester and remains 10 to 20 beats/min above baseline for the duration of the pregnancy. Systolic and diastolic blood pressures decrease in the first trimester, reach their lowest levels in the second trimester, then rise toward prepregnancy levels during the final 2 months of gestation. A decrease of 15 mm Hg for systolic and diastolic pressure is normal in the second trimester.
Hemodynamic measurements may be misleading. Signs of shock such as tachycardia and hypotension may be normal physiologic changes of pregnancy. Conversely, “normal” findings may mask an underlying shock state. Hypervolemia of pregnancy enables a woman to tolerate acute blood loss of 10% to 15% or gradual loss of 30% (1500 mL) without a change in vital signs. 5
Catecholamine release, caused by maternal hypovolemia, leads to vasoconstriction of peripheral and uterine vascular beds and shunting of blood to vital maternal organs. A 15% to 30% reduction of uterine blood flow can occur without obvious change in maternal blood pressure. Uterine hypoperfusion and fetal hypoxia can occur before evidence of maternal shock. Signs of fetal distress include fetal bradycardia, fetal tachycardia, and decreased or increased fetal movement.
Gravid women in shock may not have the cool, clammy skin typical of shock because of maternal vasodilatation during the first and second trimester. Vasoconstriction in response to stress occurs predominantly in the third trimester.
Adequate and appropriate fluid replacement is necessary to restore maternal and uteroplacental perfusion. Isotonic crystalloid solutions (e.g., normal saline or lactated Ringer’s) are acceptable for initial resuscitation. Blood transfusions should be given with Rh-compatible blood. In cases of impending shock, only O-negative or type-specific blood is acceptable. Vasopressors are not indicated for initial management of hypovolemic shock but may be used in management of cardiogenic shock secondary to cardiac contusion or distributive shock resulting from spinal cord injury.
Hematologic
Cautious interpretation of laboratory values is required. Dilutional anemia in pregnancy is caused by the disproportionate increase of plasma volume relative to erythrocyte volume. Dilutional states can decrease the hematocrit level to 31% to 34% and reduce hemoglobin to 11.0 g/dL. These changes are referred to clinically as “physiologic anemia of pregnancy.”2
Platelet levels may be normal or slightly decreased. Physiologic leukocytosis occurs during the second and third trimesters. An increase in white blood cells of 15,000/mm3 may occur by term and rise even higher during stress or labor. Sedimentation rate also increases during pregnancy. These increased levels may mask or falsely indicate an infectious process.
Fibrinogen levels start to rise in the third month and double by term. An increase in clotting factors VII, VIII, IX, X, and XII produces hypercoagulability and increased thromboembolic risk. Deep vein thrombosis and pulmonary embolism are a significant risk, especially when the gravid woman is inactive. The pregnant woman who sustains trauma is at a high risk for disseminated intravascular coagulopathy if abruptio placentae or amniotic fluid embolism occur.
Pulmonary
Significant anatomic and physiologic alterations occur in the pulmonary system during pregnancy. Capillary engorgement of the mucosal lining of the respiratory tract predisposes gravid women to nosebleeds and airway obstruction. Gentle suction and intubation may be necessary to control epistaxis and prevent airway compromise. Complications of pregnancy such as pregnancy-induced hypertension (PIH) and gestational diabetes exacerbate normal airway engorgement, making intubation more difficult. Often a smaller-than-expected endotracheal tube is required.
The diaphragm elevates as the uterus enlarges, up to 4 cm with associated flaring of the ribs. During the third trimester, chest tubes, when needed, should be inserted in the third or fourth intercostal space to avoid diaphragm injury.
Diaphragmatic elevation reduces pulmonary functional reserve capacity by 20% at the end of pregnancy. Reduction is associated with increased maternal oxygen consumption and diminished oxygen reserve. Maternal tidal volume and minute ventilations decrease to 40% by late pregnancy. Respiratory rates will increase. Arterial oxygen pressure (PaO 2) levels increase to 101 to 104 mm Hg. Arterial carbon dioxide pressure (PaCO 2) levels decrease to approximately 30 mm Hg by the end of the second trimester and remain at this level until delivery. 5
The maternal respiratory center is especially sensitive to minute changes in PaCO 2 levels. Although normal arterial and venous pH levels are maintained because of increased renal excretion of bicarbonate, partially compensated respiratory alkalosis occurs during pregnancy, making the pregnant patient less able to cope with respiratory distress and acidosis associated with trauma. A diminished maternal oxygen reserve makes the gravid uterus vulnerable to hypoxia. Because maternal hypoxia affects fetal oxygenation, fetal compromise may occur with minimal maternal distress. Fetal heart rate changes are frequently the first indicator of maternal hypoxia. Maternal trauma may require blood gas analysis to determine hypoxia and acidosis. Supplemental oxygen at 100% F iO 2 is essential until maternal and fetal hypoxia are ruled out or resolved.
Gastrointestinal
Various anatomic and physiologic gastrointestinal (GI) changes occur during pregnancy. The small bowel is pushed up into the upper abdomen by the uterus, and the large bowel moves posteriorly. Diminished bowel sounds may be a normal finding in pregnancy or indicate intraperitoneal injury. Stretching of the abdominal wall due to uterine growth can impair maternal sensitivity to peritoneal irritation, so muscle guarding, rigidity, or rebound tenderness may be dulled or absent.
Increased progesterone and estrogen affect the GI tract, reducing motility and tone and relaxing the gastric sphincter. Gastric emptying is delayed, and gastroesophageal reflux occurs frequently. The lower esophageal sphincter is displaced into the thorax. Risk for aspiration is increased. As with all trauma patients, the pregnant patient is always considered to have a full stomach. A gastric tube should be considered early in the resuscitation to minimize risk for aspiration; nasal insertion of gastric tubes should be performed cautiously (to minimize the risk for epistaxis) using a smaller-size tube.
Genitourinary
Maternal susceptibility to traumatic bladder injury increases as the bladder moves from a pelvic organ to an intraabdominal position by 12 weeks’ gestation. Urinary frequency increases in the third trimester because of bladder compression by the uterus. Dilation of the ureters, renal calyces, and pelvis from compression by the ovarian plexus can result in urinary stasis. Glomerular filtration rate increases, causing a decrease in blood urea nitrogen and creatinine.
Musculoskeletal
The pelvis becomes more flexible during pregnancy in preparation for fetal delivery. Hormonal changes loosen ligaments of the symphysis pubis and sacroiliac joints. By 7 months’ gestation, there is considerable widening of the pelvis. An unsteady gait, usually caused by the widening pelvis and heavy abdomen, predisposes the gravid female to falls.
Neurologic
Changes in the central nervous system (CNS) related to pregnancy are abnormal findings. PIH (formerly referred to as preeclampsia) may occur after 20 to 24 weeks’ gestation and is characterized by hypertension, proteinuria, and edema. CNS irritability can lead to seizures (eclampsia). Hypoxia from seizure activity places the mother and fetus at risk. Altered mentation, seizures, and hypertension may also indicate head injury; therefore meticulous neurologic assessment of the pregnant trauma patient is essential.
Endocrine
The pituitary gland doubles in size and weight by term, requiring a greater blood supply. Hypoperfusion causes ischemia and can lead to pituitary necrosis. Hemorrhage within the gland can occur with reperfusion. Sheehan’s syndrome, which is necrosis of the anterior pituitary gland, produces long-term complications related to decreased hormone levels. 5 Aggressive and rapid treatment of shock is required to prevent these serious complications.
PATIENT ASSESSMENT
The anatomic and physiologic changes of normal pregnancy can obscure the mother’s response to trauma. Maternal compensatory mechanisms preserve vital maternal functions at the expense of the fetus. Fetal survival depends on adequate gas exchange and uterine perfusion. Rapid and efficient assessment and appropriate intervention for specific abnormalities provides for an optimal maternal-fetal outcome.
The primary survey focuses on airway, breathing, and circulation. Repositioning the airway by chin-lift or jaw-thrust maneuvers may be enough to establish patency and should not interfere with cervical spine protection. Airway adjuncts should be used as needed to prevent secondary injury from hypoxia; nasal airways should be used with caution because the mother may be predisposed to nasopharyngeal bleeding that can lead to further airway obstruction.
Cervical spine protection is maintained until the neck is cleared. If injury is suspected, spinal protection should be maintained with a rigid cervical collar; the patient should be logrolled off the backboard as soon as possible and pillows or foam wedges used to tilt the patient 15 degrees laterally to deflect the uterus from the vena cava.
All trauma patients need supplemental oxygen. Injury can exacerbate existing pulmonary alterations related to pregnancy, such as decreased pulmonary reserve and increased maternal oxygen consumption, compromising the mother and fetus. Oxygen is critical for fetal survival because of fetal inability to tolerate hypoxia.
Assessment and intervention for external and internal hemorrhage is necessary to ensure maternal-fetal survival. Apply direct pressure to sites of uncontrolled external bleeding. The mother can lose 1500 mL of blood before signs of shock are evident. Retroperitoneal and uteroplacental injury can be sources of occult blood loss. Venous access with two large-bore catheters and aggressive fluid volume replacement optimize maternal blood volume and oxygen-carrying capacity. Initiate blood replacement with Rh-compatible blood if crystalloids do not stabilize circulatory status. Aortocaval compression can occur by 20 weeks’ gestation; therefore displacing the uterus can increase cardiac output by 20%. Insertion of an arterial line or central venous line provides accurate monitoring of circulation and response to treatment and may be used in some centers.
Primary assessment includes a brief neurologic assessment. If neurologic deficits are found, both PIH and trauma should be considered as potential causes.
Secondary assessment involves identification of other injuries. Thorough history includes standard trauma history and obstetric history—last menstrual period (LMP), expected date of delivery , parity, problems and complications of current or past pregnancies, presence of uterine contractions, and current fetal activity. Focused obstetric assessment in the secondary survey includes evaluation of the abdomen, uterus, and fetus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


