The Gastrointestinal System
Objectives
1. Analyze major causative factors in the development of disorders of the gastrointestinal system.
2. Summarize measures to prevent development of disorders of the gastrointestinal system.
4. Describe the assessment of a patient with a possible gastrointestinal disorder.
5. Evaluate the care of the patient who is having a liver biopsy.
1. Perform an assessment of gastrointestinal status.
3. Evaluate the outcomes of care for a patient who is experiencing diarrhea.
Key Terms
absorption (ăb-sŏrp-shŭn, p. 623)
adhesions (ăd-HĒ-shŭnz, p. 623)
anabolism (ă-NĂB-ŏ-lĭzm, p. 623)
anorexia (ăn-ŏ-RĔK-sē-ă, p. 633)
ascites (ă-SĪ-tēz, p. 631)
catabolism (kă-TĂB-ō-lĭzm, p. 623)
chyme (KĪM, p. 621)
flatus (FLĀ-tŭs, p. 635)
mastication (măs-tĭ-KĀ-shŭn, p. 620)
metabolism (mĕ-TĂ-bō-lĭzm, p. 623)
pancreatitis (păn-krē-Ă-TĪ-tĭs, p. 624)
peristalsis (pĕr-ēs-TĂL-sĭs, p. 623)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Overview of Anatomy and Physiology of the Gastrointestinal System
What are the Organs and Structures of the Gastrointestinal System?
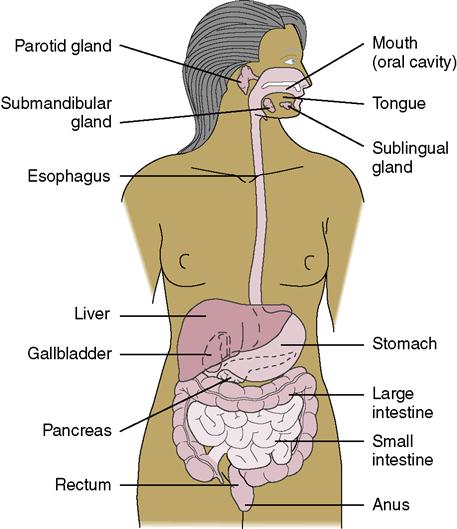
• Organs of the gastrointestinal (GI) system are the mouth, pharynx, esophagus, stomach, small intestine, large intestine, rectum, and anus (Figure 28-1).
• The accessory organs are the liver, gallbladder, and pancreas (Figure 28-2).
• The stomach lies in the upper left portion of the abdominal cavity (see Figure 28-1).
• The pyloric sphincter controls release of food substances into the small intestine (Figure 28-3).
• The small intestine is divided into the duodenum, jejunum, and ileum and is about 6 m long.
• The ileocecal valve controls the progress of substances into the large intestine.
• The colon has four portions: the ascending, transverse, descending, and sigmoid colon.
• The appendix is attached to the cecum and has no known function in the digestive process.


What are the Functions of the Gastrointestinal System?
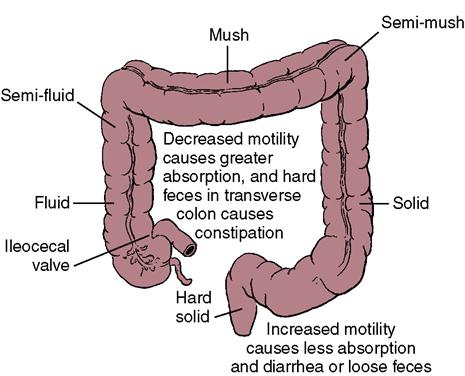
• The large intestine reabsorbs water and electrolytes, formulates some vitamin K, and eliminates waste products (Figure 28-4).
• The large intestine is populated with bacteria that aid in the breakdown of waste products.
• The rectum stores fecal material until it is eliminated through the anus.
What Effects does Aging have on the Gastrointestinal System?
What are the Structures and Locations of the Accessory Organs?
What are the Functions of the Gallbladder, Liver, and Pancreas?
• The liver manufactures and secretes bile and bile salts necessary to digest fat.
• The liver synthesizes albumin, fibrinogen, globulins, and clotting factors.
• The liver is responsible for how drugs are metabolized.
• The liver may store between 200 and 400 mL of blood.
• The liver synthesizes the prothrombin needed for normal blood clotting.
How does Aging Affect the Accessory Organs of Digestion?
The Gastrointestinal System
The intestinal tract and accessory organs of digestion perform the intake, absorption, and assimilation of food to provide nourishment for the body. The transfer of nutrients from the intestine into the blood is referred to as absorption. Food substances are moved along the intestinal tract by peristalsis (wavelike motions of involuntary muscles within the walls of the organs). Metabolism is the sum of many physical and chemical processes of the absorbed nutrients. Metabolic activities involve the synthesis of substances needed to build, maintain, and repair body tissues (anabolism). Metabolism is also responsible for the breakdown of larger molecules into smaller molecules so that energy is available (catabolism).
Gastrointestinal System Disorders
Causes
The gastrointestinal tract is subject to infection, inflammation, physical and chemical trauma, and structural defects. An intestinal tract problem may occur due to blockage of movement of food through the intestine (intestinal obstruction). Postoperative adhesions sometimes cause intestinal obstruction. Adhesions are bands of scar tissue that bind two anatomical surfaces together that are normally separate. Tumor may also cause intestinal obstruction. Obstruction of the bile or pancreatic ducts can cause interference with the flow of digestive juices and of the enzymes needed for digestion. Continued irritation and inflammation of the GI mucosa can lead to intestinal bleeding and to increased peristalsis, causing inadequate absorption of nutrients.
Psychological and emotional stresses greatly influence appetite and motility of the stomach and intestines. The secretion of digestive juices in amounts sufficient for the breakdown of food is regulated in part by the emotions. Excessive stimulation of digestive acid and enzymes can cause a breakdown in the integrity of the mucous membrane lining the digestive tract. The damage to the mucous membrane can result in gastric or duodenal ulcers and chronic colitis.
Some disorders, such as Crohn’s disease and ulcerative colitis, are correlated with a genetic predisposition. Both disorders are more common among the Jewish population. Certain forms of colon cancer have been identified as having a genetic link and there is a familial tendency for the occurrence of colon cancer. Esophageal and stomach cancer are linked to consumption of charred foods and those containing nitrites. Cigarette smoking is linked to stomach cancer.
Autoimmune diseases often affect the GI system, causing inflammation or fibrosis of organs. Treatments such as drug and radiation therapy may cause GI problems as a side effect. Some people who have undergone chemotherapy for cancer develop a mechanical form of sprue, a malabsorption problem that remains even after chemotherapy is complete. Lactose intolerance, which is not uncommon in the older adult, may cause continuous diarrhea and malabsorption.
Causes of Gallbladder Disorders
The formation of stones within the gallbladder can cause irritation and create areas susceptible to inflammation and infection. Stones can lodge in the common duct, causing obstruction to the flow of bile. Liquid weight loss diets or very rapid weight loss appears to be associated with developing gallstones. Women develop gallstones more frequently than men. The incidence increases with age; obesity and having several children. People who have diabetes mellitus or Crohn’s disease are at higher risk for the disorder.
Causes of Liver Disorders
The liver filters out many toxic substances and is constantly exposed to any infectious organisms circulating in the bloodstream. The hepatitis virus in particular attacks the liver, causing inflammation and damage to the tissue. Hepatitis B and C are implicated in liver cancer (Clin-eguide Guideline, 2010). Healthy People 2020 objectives include not only reducing the number of hepatitis infections, but also increasing the percentage of people who are actually aware that they have a hepatitis infection.
Many drugs and chemicals are toxic to the liver, and the nurse should always be aware of the drugs a patient is taking that may cause liver damage. Alcohol and other toxic substances are major factors in  the development of cirrhosis of the liver (Box 28-1) (Mehta & Rothstein, 2009).
the development of cirrhosis of the liver (Box 28-1) (Mehta & Rothstein, 2009).
Liver trauma or laceration may cause massive internal hemorrhage. However, the liver is resilient and will regenerate, if part of the liver remains functional and repair is performed quickly.
Parasites may cause cirrhosis, cysts or abscesses. Most parasites that damage the liver enter the body when people wade or swim in contaminated water in tropical countries, or eat contaminated food.
Cancer in the liver may be primary, or may be secondary to metastasis from a site elsewhere in the intestinal tract.
Causes of Pancreatic Disorders
Pancreatitis (inflammation of the pancreas) is associated with alcoholism, obstructive cholelithiasis, peptic ulcer, hyperlipidemia, and trauma. Pancreatic cancer incidence rises steadily with age. Although the cause of pancreatic cancer is not known, the incidence is higher in cigarette smokers. Obesity, chronic pancreatitis, and diabetes mellitus are also risk factors for this cancer. (See Chapter 38 for information on diabetes mellitus.)
Prevention of Gastrointestinal System Disorders
Eating a normal, well-balanced diet aids digestion. Maintaining good oral health is important to the health of the rest of the body (Kullberg et al., 2009). Consuming sufficient bulk in the diet helps maintain a healthy colon by enhancing passage of waste. A diet lacking in fiber is one factor in the development of diverticulosis, in which pockets form along the colon where waste material can lodge. Drinking at least eight glasses of fluid a day prevents constipation by helping to keep the stool moist.
Heeding the need to defecate promptly aids in keeping the gastrocolic reflex functioning well and prevents constipation and hemorrhoids. Straining at stool increases intra-abdominal pressure which causes the hemorrhoidal vessels to engorge and contributes to hemorrhoid formation. Decreased mobility in the elderly patient often leads to digestive problems; therefore ambulation is encouraged
Maintaining body weight within normal limits helps prevent hiatal hernia and esophageal reflux. Developing healthy coping mechanisms and keeping stress within acceptable limits may prevent ulcers and chronic irritability of the bowel.
Mechanical and chemical irritants that produce inflammation often can be identified by elimination diets to determine the foods that cause GI upsets. Once the offending foods are identified, the patient can learn to avoid those foods and to maintain adequate nutrition.
Following general rules of good hygiene and sanitation can prevent many infectious GI upsets: wash the hands before eating and clean cooking and eating utensils properly. Food poisoning can be prevented by adequate refrigeration and by proper canning, freezing, and food-handling methods. Meats, and foods containing mayonnaise or dairy products, should be kept chilled. When not in the refrigerator, food should be kept covered.
Prevention of Gallbladder Disorders
Maintaining a normal body weight, eating a low-fat, low-cholesterol, high fiber and high calcium diet, avoiding rapid weight loss diets, consuming alcohol moderately, and maintaining an active lifestyle all help prevent gallstones (Clin-eguide, 2009).  If gallstones are irritating the gallbladder, prompt surgery might help to prevent cancer.
If gallstones are irritating the gallbladder, prompt surgery might help to prevent cancer.
Prevention of Liver Disorders
Obtaining immunization against hepatitis A and hepatitis B helps to prevent these viral diseases. A vaccine against hepatitis C is under study at present. Using Standard Precautions (see Appendix B) when handling any body fluids, particularly blood, greatly reduces the risk of infection with hepatitis B and C, which may decrease the chance of developing liver cancer. Refraining from consuming excessive amounts of alcohol decreases the risk of developing cirrhosis of the liver. Avoiding exposure to known toxic or carcinogenic chemicals helps prevent liver damage and liver cancer.
Prevention of Pancreatic Disorders
Avoiding consumption of large quantities of alcohol may prevent pancreatitis. Removing a gallbladder that has gallstones can help prevent obstruction of the pancreatic duct with stones. Removal prevents backup of pancreatic enzymes that are thought to be a cause of pancreatitis. Compliance with therapy for a peptic ulcer helps prevent irritation of the pancreas and resultant pancreatitis. Smoking cessation decreases the risk of pancreatic cancer.
Diagnostic Tests, Procedures, and Nursing Implications
Diagnostic tests for disorders of the intestinal tract and accessory organs consist of x-rays, computed tomography (CT) scans, nuclear medicine scans, magnetic resonance imaging, ultrasound studies, endoscopy, biopsy, laboratory tests, tests of gastric secretions, and stool and urine studies (Table 28-1).
Table 28-1
Diagnostic Tests for Gastrointestinal (GI) Disorders