CHAPTER 28. Pediatric Trauma
Autumne Bailey Mayfield and Kate Copeland
Despite scientific advances in injury prevention and treatment, traumatic injury continues to be the leading cause of death in children older than 1 year of age. Each year approximately 20,000 children and teenagers die as a result of injury. For every child who dies from an injury, 40 others are hospitalized and 1120 are treated in emergency departments (EDs). An estimated 50,000 children acquire permanent disabilities each year, most of which are the result of closed head injury. Pediatric trauma continues to be one of the major threats to the health and well-being of children. 1
Several factors influence childhood injuries, including age, sex, behavior, and the surrounding environment. Of these, age and sex are the most important factors affecting the patterns of injury. Male children younger than 18 years have higher injury and mortality rates, most likely due in part to their more aggressive behavior and exposure to contact sports. In the infant and toddler age-group, falls are a common cause of severe injury. The most common scene of pediatric injuries is the home environment, where approximately 35% of significant injuries occur. 1
The frequency of childhood injuries compels the emergency nurse to participate in primary, secondary, and tertiary prevention of pediatric injuries. This chapter highlights anatomic and physiologic differences in pediatric patients, describes patient assessment, reviews essential interventions, discusses treatment of selected traumatic injuries, and identifies specific injury prevention strategies.
EPIDEMIOLOGY
Blunt force trauma is the most common mechanism of pediatric morbidity and mortality, including motor vehicle crashes (MVCs), all-terrain and off-road vehicles, falls, pedestrian incidents, and bicycle crashes. 1 MVCs are the leading cause of death from blunt force trauma, 18 with most fatalities resulting from head injuries. 16 In 2005, MVCs killed 1946 child occupants under 14 years of age, with an average of 640 children injured every day. 35 Penetrating trauma accounts for 10% to 20% of all pediatric trauma admissions. Gunshot wounds are responsible for most penetrating injuries and carry a significantly higher mortality compared with blunt mechanism injury. 1 A rising incidence of pediatric penetrating trauma has occurred because of the proliferation of handguns and increased violence. 1 Access to firearms in the home increases the risk for unintentional firearm-related death and injury among children. Unintentional shootings cause more than 20% of all firearm-related deaths among children ages 14 and under. These two mechanisms of injury, blunt and penetrating, are interrelated in that blunt mechanical force can result in penetrating injury, such as that caused by fender edges, door handles, or shrapnel. 1
For children between the ages of 4 and 14, unintentional injury-related deaths occur most often when riding in a car. Children are most often injured, suffer more severe injuries, or die in MVCs when they are not properly restrained. Within this age-group, children 4 to 8 years of age are especially at risk for injury because of the improper use of safety belts in motor vehicles. Safety seats are the most effective protection against fatal injury to child motor vehicle passengers. Rear-facing infant safety seats reduce the risk for death in an MVC by 71%, forward-facing seats for toddlers reduce risk for death by 54%, and safety belts reduce risk for death by 45%. 36 However, parents must know how to correctly install and use child safety seats to achieve the most protection for their children. The American Academy of Pediatrics is a valuable resource for car safety seats for families. 8 As many as 85% of child safety seats are found to be improperly installed. Infants should be placed in rear-facing seats until they are at least 1 year of age and weigh at least 9 kg (20 pounds) because they have large heads, proportionally, and weak neck muscles, which place them at risk for cervical distraction and dislocation during frontal crashes. 39 Children do not fit in adult shoulder and lap belts (without a booster seat) until they are 58 inches tall and weigh 36 kg (80 pounds). However, children between the ages of 4 and 8 years who have outgrown their child safety seat often are placed too soon in adult lap and shoulder belts without a booster seat. It is estimated that only 5% of children in this age-group are properly restrained with booster seats in motor vehicles. Children restrained with a lap belt and shoulder harness are susceptible to certain injuries. Young children have a shorter sitting height than adults and a higher center of gravity above the lap belt. A greater proportion of body mass is located above the safety belt, which may cause more forward motion and increase the risk for head and neck injury. Children can jackknife over restraints, causing an airway or hanging injury. Similarly, a child can “submarine” under the restraint system, leading to neck and airway injuries. The lap belt itself can also cause injuries. During sudden deceleration, children are thrown forward with their full body weight going into the lap belt. Resulting injuries include lumbar spine fractures, small bowel injuries, and abdominal bruising.
Sitting in the rear seat of a car offers significant protection during an MVC. Restraint use enhances this effect4; therefore parents must be encouraged to restrain children with proper child safety devices in the vehicle’s rear seat for optimal protection in the event of an MVC.
Other high-risk motor vehicle situations are trunk entrapment and leaving children unattended in cars. Unintentional trunk entrapment leads to death in 35% to 40% of cases. When left unattended, children may be able to start the vehicle or put the vehicle in neutral. In addition, they can suffer from hypothermia and hyperthermia dependent on environmental temperature.
In 2005, a total of 414, or 21%, of the fatalities among children age 14 and younger occurred in crashes involving alcohol. Over half were passengers in vehicles with drivers who had blood alcohol levels of 0.01 g/dL or higher. An additional 48 children under the age of 14 were killed by drinking drivers when they were pedestrians or on bicycles. 35
Annually approximately 1000 16-year-old drivers are involved in fatal crashes, and traffic injury is the leading cause of death of adolescents. Graduated driver-license programs, which place restrictions on new drivers, have reduced the incidence of fatal crashes by 11%. The more comprehensive programs have the greatest effect on decreasing fatalities and injuries among this age-group. 14
Children and adolescents sustain injuries as passengers or operators of all-terrain vehicles, two-wheeled off-road vehicles, and go-carts/buggies. These children had a mean age of 12.7 years, and 77% were male. Most injuries occur from disruptions in the driving surface, such as bumps, holes, and uneven terrain. 10 Young children riding as passengers can be crushed by the adult driver on impact with a stationary or moving object. Older children who are not the appropriate size or weight to operate such vehicles can flip vehicles onto themselves and sustain serious multisystem injuries.
Falls are the most common mechanism of injury in children and the leading cause of nonfatal injuries in children below the age of 14. 1 Many serious falls among children occur on playgrounds and during sports and recreational activities. Falls in the youngest children happen more often in the home environment, on stairs, furniture, and out of windows, from varying heights. 21 They also fall while running, playing, and participating in sports. Injuries sustained from falls vary from mild to severe single-system or multisystem trauma.
Injuries associated with shopping carts occur especially among children younger than 5 years. Injuries to children occur via several mechanisms, including falling from carts, carts tipping over, becoming entrapped in a cart, and being run over by a cart. 33 Head injuries account for approximately two thirds of all injuries associated with falls from shopping carts. 32
Pedestrian injuries are a common cause of morbidity and mortality in the pediatric population. As pedestrians, children are struck by moving vehicles while playing, walking, running, crossing the street, or entering or exiting a school bus. Rates of childhood pedestrian injuries have been reported as 2.5 times higher on one-way streets compared to two-way streets. 37 Most injuries occur in the afternoon and early evening hours on urban streets. Lower socioeconomic status and urban domicile have also been implicated in pedestrian incidents, with a rate three times higher for children from poorer neighborhoods compared with those from wealthier neighborhoods. 37
Young children struck by motor vehicles in driveways are at risk for severe injury and death. During 2001-2003, an estimated 7475 children between the ages of 1 and 14 years were treated for nonfatal motor vehicle back-over injuries. 21 Approximately 100 children suffer fatal injuries per year in driveways or parking lots, often when relatives or family friends back over them. 31 Children younger than 5 years of age struck in their driveway had a higher Injury Severity Score (ISS), were more likely to sustain a closed-head injury, and were more likely to die compared with children older than 5 years of age struck in their driveway. 27
Bicycle crashes are a common mechanism of fatal and nonfatal injuries. Approximately 373,000 children are treated in hospital EDs for bicycle-related injuries each year in the United States. More than 40% of all bicycle-related deaths are due to head injuries with the largest percentage among children under the age of 14. Other injuries associated with bicycle crashes are long bone fractures and abdominal, thoracic, and facial injuries. Wearing a bicycle helmet can reduce the likelihood of head injury by 85% and brain injury by 88%. Universal use of bicycle helmets by children ages 4 to 15 would prevent between 135 and 155 deaths, between 39,000 and 45,000 head injuries, and between 18,000 and 55,000 scalp and facial injuries annually. Helmet use significantly reduces morbidity and mortality associated with bicycle-related head injuries. Primary and secondary prevention are equally important in the use of helmets among children. Children who present following a minor injury provide an opportunity for educating the child and family on the importance of proper helmet use. 18
Children can sustain injuries from skateboards and scooters. Children have a high center of gravity, which limits their ability to break a fall. The American Academy of Pediatrics recommends that children under the age of 10 years should not use skateboards without close supervision by an adult or responsible adolescent. Children younger than 5 years should not use skateboards. 34 These children do not have a well-developed neuromuscular system, do not have good judgment, and cannot protect themselves from injury. Skateboards should not be ridden in traffic. Proper protective wear, including helmets, elbow pads, and knee pads, should be worn. Skateboard-related injuries account for an estimated 50,000 ED visits and 1500 hospitalizations each year. Nonpowered scooter–related injuries accounted for an estimated 9400 ED visits; 90% of these were for children under the age of 15 years. 34 Proper protective gear for scooter safety includes a helmet, knee pads, and elbow pads; wrist guards are not recommended because they make it difficult to grip the handle and steer the scooter. Children less than 8 years of age should not use scooters without close adult supervision. Children should not ride scooters in streets, in traffic, or at night. 34
Drowning and near-drowning injuries resulted in 1178 deaths for all ages in 2002. 21 In 2003 approximately 4200 children ages 14 and under were treated in EDs for accidental drowning incidents. Bathtub drowning is most common in children younger than 1 year of age. In the preschool-age child, drowning occurs most commonly in residential swimming pools. Young adults typically drown in ponds, lakes, rivers, and oceans. Alcohol use has been involved with 25% to 50% of adolescent drownings associated with water recreation. 23 Children should never be unsupervised when in or around water.
ANATOMY AND PHYSIOLOGY
Children differ from adults developmentally, anatomically, and physiologically. Recognizing differences and implementing appropriate interventions to support these differences can result in increased survivability of the pediatric trauma patient.
Respiratory System
Crucial anatomic and physiologic differences exist between the adult and pediatric airway. The child’s oropharynx is relatively small; therefore the airway is easily obstructed by the large tongue. The U-shaped epiglottis protrudes into the pharynx, with the tonsils and adenoids often enlarged. Vocal cords are short and concave, with the larynx relatively cephalad and easily collapsible if the neck is hyperflexed or extended. In a child younger than 10 years of age, the narrowest portion of the airway is the cricoid cartilage. 28 Lower airways are smaller and supporting cartilage less developed in infants and small children, so airways are easily obstructed by mucus and edema. 28
Ribs are pliable and do not provide adequate protection and support for the lungs; therefore blunt trauma to the chest causes pulmonary contusions rather than rib fractures. If rib fractures are present, a high index of suspicion for severe internal trauma should be raised. The mediastinum is more mobile, causing greater susceptibility to great-vessel damage. Retractions are more likely when the child is in respiratory distress. These can be suprasternal, supraclavicular, infraclavicular, intercostal, or substernal. Breathing is primarily diaphragmatic or abdominal in children younger than 7 or 8 years of age. Crying children are more prone to swallowing air, which causes gastric distension and hampers respiratory excursion. A thin chest wall transmits breath sounds easily from one location or side of the thorax to another, which can make an accurate respiratory assessment difficult; it is challenging to detect the presence of a pneumothorax by auscultation alone in younger children. Respiratory rates are higher in children because of higher metabolic rates. Oxygen consumption in infants is 6 to 8 mL/kg/min compared with 3 to 4 mL/kg/min in adults; therefore hypoxemia can occur rapidly. 28
Cardiovascular System
The child’s estimated blood volume is 80 mL/kg. Although this absolute blood volume is small, it is larger than an adult’s on a milliliter per kilogram basis. Seemingly small amounts of blood loss can impair perfusion and decrease circulating blood volume. Because of their large cardiac reserve and catecholamine response, children can maintain a high to normal blood pressure even with significant blood loss. Hypotension is not observed until the child has lost 20% to 25% of circulating blood volume. 28 Hypotension is a late sign of hypovolemia in children and signals imminent cardiac arrest. The best assessment of perfusion is skin parameters (color, temperature, moisture) and capillary refill—normal is 2 seconds or less on all four extremities and checked at frequent intervals. Other assessment factors include the presence of bradycardia or tachycardia with decreased urinary output.
Children have a higher metabolic rate and oxygen requirement that requires a higher cardiac output per kilogram. 28 Tachycardia is the initial response to decreased oxygenation. When tachycardia fails to increase oxygen delivery, tissue hypoxia and hypercapnia occur, followed by bradycardia. 28 Bradycardia is a late sign of cardiac decompensation.
Children can present with a variety of congenital heart defects (e.g., tetralogy of Fallot, large ventricular septal defect) that may impair circulatory status. If a child has had a shunting surgical procedure to redirect blood flow, blood pressure readings are unattainable in the arm from which the subclavian artery was used because that arm is perfused by collateral circulation. Children may also have functional or nonfunctional heart murmurs. Children with congenital heart defects may also experience heart failure and dysrhythmias.
Neurologic System
An infant’s head is larger in proportion to the rest of the body than an adult’s. The skull is more malleable, providing less protection to the brain. The posterior fontanel closes at age 4 months; the anterior fontanel is normally closed by age 18 months. Although open fontanels allow for release of increased intracranial pressure (ICP), they may allow direct injury to the brain or cause extensive bleeding. Infants bleed significantly from a scalp laceration because of the large surface area and increased vascularity. Finally, a young child has a higher center of gravity, which, together with the larger head, makes the child prone to head injuries.
Children’s cerebral tissues are thin, soft, and flexible compared with those of adults. Sulci are still deepening during childhood, and myelinization is still occurring. These differences make brain tissues more easily damaged, especially from shearing injuries. Several features make the cervical spine vulnerable to injury in children younger than 9 years of age12:
• The head is disproportionately large, making the child vulnerable to flexion-extension injury.
• The neck muscles are underdeveloped.
• The vertebral bodies are wedge shaped.
• The articulating facets are angled horizontally, resulting in subluxation from minimal force.
• The end plates are cartilaginous.
• The interspinous ligaments are elastic and lax, leading to increased spinal mobility.
Gastrointestinal and Genitourinary Systems
Young children have protuberant abdomens as a result of underdeveloped abdominal musculature. 29 Because solid abdominal organs are relatively larger in children compared with adults, there is an increased risk for direct organ injury following blunt and penetrating kinetic forces. 29 A pliable rib cage does not afford adequate protection to abdominal organs and can predispose children to further internal injuries. The large size of the organs in a relatively small space predisposes children to have multiple organ injury with trauma. Though partially protected by the flexible rib cage, the liver is still vulnerable to injury because of its large size and fragility. The transverse diameter of the abdomen is small, and lower abdominal organs are not well protected by the pelvis. 25 Renal injuries occur because the relatively large kidneys are not protected by the small amount of perinephric fat, weak abdominal muscles, and elastic rib cage. The kidneys also retain fetal lobulations, which may predispose these organs to separation and fracture. 29 Congenital abnormalities such as hydronephrosis, horseshoe kidneys, and ectopic kidneys make the child more susceptible to renal trauma. Many congenital anomalies are not diagnosed until abdominal trauma has occurred. Greater elasticity makes ureteral tearing rare. Ureteral injuries are suspected with penetrating trauma to the abdomen or flank area. The bladder is an abdominal organ and not well protected. In girls the bladder neck is also less protected. Tissues of a prepubescent girl are more rigid because of a lack of estrogen; they do not become more pliable until adolescence, when estrogen is released.
Musculoskeletal System
The periosteum in a growing child is stronger, thicker, and more osteogenic compared with the periosteum in an adult, which results in decreased fracture displacement and fewer open fractures. 21 Consequently, four unique bone fracture patterns are found in children: plastic deformity (the bone is deformed but not broken); torus (buckle) fracture (compression forces applied at the metaphysis and diaphysis cause bone to buckle rather than break because of its porous nature); greenstick fracture (an incomplete fracture in which the compressed side’s cortex and periosteum are intact); and physis fractures (injury to the growth plate, which can lead to angulation deformities if not diagnosed and treated properly). 21 Bone osteogenicity allows rapid callus formation, permitting bones to heal quickly. Even though bone is strong, fractures occur more frequently than muscle sprains or ligament tears because these structures are stronger than the bones themselves.
Another unique feature of the pediatric musculoskeletal system is the presence of a physis or growth plate. This area of bone, which is responsible for longitudinal bone growth, is found between the epiphysis and metaphysis. The physis is cartilaginous and does not ossify until puberty; therefore treatment to attain proper anatomic alignment is critical to optimize bone growth and reduce the risk for deformity. 21
Integumentary System
Children have a larger ratio of body surface area to weight, which makes them prone to convective and conductive heat loss. Having less subcutaneous fat for insulation can increase heat loss through radiation, convection, conduction, and evaporation. Infants younger than 6 months of age do not have the fine-motor coordination to shiver and are unable to keep themselves warm. Nonshivering thermogenesis does occur in infants, in which brown fat is broken down slowly to produce warmth. Shivering is a high-energy-consuming, nonproductive muscular activity initiated for thermogenesis. 7 Shivering may not be possible in injured children receiving sedation or neuromuscular blocking agents. 7
PATIENT ASSESSMENT
Each ED should be equipped with personnel and supplies necessary to treat an injured child effectively and efficiently. Equipment should be readily available and prepared before patient arrival.
Initial assessment and stabilization of the pediatric trauma patient requires knowledge of developmental and physiologic differences among infants, children, and adolescents. Injured children are frightened—strange, painful things are happening. The patient may feel he or she is being punished for a real or imagined wrongdoing. Talking with the child in language he or she understands is essential for relieving anxiety and developing trust.
Initial assessment consists of a primary and secondary assessment. During primary assessment, airway with cervical spine protection, breathing, circulation, and disability (neurologic status) are assessed. Life-threatening injuries are identified and treated. Table 28-1 describes the primary survey in the preferred order. During secondary assessment, all other body systems are assessed and other injuries are treated. Table 28-2 details the secondary survey. Throughout the initial assessment and stabilization, airway, breathing, and circulation are continually reassessed.
| Component | Actions |
|---|---|
| Airway | Assess for patency; look for loose teeth, vomitus, or other obstruction; note position of head. |
| Suspect cervical spine injury with multiple trauma; maintain neutral alignment during assessment; evaluate effectiveness of cervical collar, cervical immobilization device, or other equipment used to immobilize the spine. | |
| Open cervical collar to evaluate neck for jugular vein distension and tracheal deviation. | |
| Breathing | Auscultate breath sounds in the axillae for presence and equality. |
| Assess chest for contusions, penetrating wounds, abrasions, or paradoxical movement. | |
| Circulation | Assess apical pulse for rate, rhythm, and quality; compare apical and peripheral pulses for quality and equality. |
| Evaluate capillary refill; normal is 2 seconds or less. | |
| Check skin color and temperature. | |
| Disability | Assess level of consciousness; check for orientation to person, place, and time in the older child. |
| In a younger child, assess alertness, ability to interact with environment, and ability to follow commands. Is the child easily consoled and interested in the environment? Does the child recognize a familiar object and respond when you speak to him or her? | |
| Check pupils for size, shape, reactivity, and equality. | |
| Remove clothing to allow visual inspection of entire body. | |
| Expose | Note open wounds or uncontrolled bleeding. |
| Component | Actions |
|---|---|
| Head, eye, ear, nose | Assess scalp for lacerations or open wounds; palpate for step-off defects, depressions, hematomas, and pain. |
| Reassess pupils for size, reactivity, equality, and extraocular movements; ask the child if he or she can see. | |
| Assess nose and ears for rhinorrhea or otorrhea. | |
| Observe for raccoon eyes (bruising around the eyes) or Battle’s sign (bruising over the mastoid process). | |
| Palpate forehead, orbits, maxilla, and mandible for crepitus, deformities, step-off defect, pain, and stability; evaluate malocclusion by asking child to open and close mouth; note open wounds. | |
| Inspect for loose, broken, or chipped teeth as well as oral lacerations. | |
| Check orthodontic appliances for stability. | |
| Evaluate facial symmetry by asking child to smile, grimace, and open and close mouth. | |
| Do not remove impaled objects or foreign objects. | |
| Neck | Open cervical collar, and reassess anterior neck for jugular vein distension and tracheal deviation; note bruising, edema, open wounds, pain, and crepitus. |
| Check for hoarseness or changes in voice by asking child to speak. | |
| Chest | Obtain respiratory rate; reassess breath sounds in anterior lobes for equality. |
| Palpate chest wall and sternum for pain, tenderness, and crepitus. | |
| Observe inspiration and expiration for symmetry or paradoxical movement; note use of accessory muscles. | |
| Reassess apical heart rate for rate, rhythm, and clarity. | |
| Abdomen/pelvis/genitourinary | Observe abdomen for bruising and distension; auscultate bowel sounds briefly in all four quadrants; palpate abdomen gently for tenderness; assess pelvis for tenderness and stability. |
| Palpate bladder for distension and tenderness; check urinary meatus for signs of injury or bleeding; note priapism and genital trauma such as lacerations or foreign body. | |
| Have rectal sphincter tone assessed, usually by physician. | |
| Musculoskeletal | Assess extremities for deformities, swelling, lacerations, or other injuries. |
| Palpate distal pulses for equality, rate, and rhythm; compare to central pulses. | |
| Ask child to wiggle toes and fingers; evaluate strength through hand grips and foot flexion/extension. | |
| Back | Logroll as a unit to inspect back; maintain spinal alignment during examination; observe for bruising and open wounds; palpate each vertebral body for tenderness, pain, deformity, and stability; assess flank area for bruising and tenderness. |
Initial Stabilization
Airway/Cervical Spine
The tongue is the most common cause of airway obstruction in the child. Opening the airway with the jaw-thrust technique to prevent hyperextension of the cervical spine is the initial step in relieving airway obstruction. Suction the oropharynx with a tonsil suction device if vomitus, blood, or loose teeth are present.
Place an oropharyngeal airway to help maintain airway patency in the child with altered level of consciousness who does not have an intact gag reflex. Oropharyngeal airways are measured from the corner of the mouth to the tragus of the ear. An oropharyngeal airway that is too small or too large will obstruct the airway, so correct size is critical. Use a tongue depressor to insert the airway directly. Do not rotate 90 degrees as in the adult patient because a child’s oropharyngeal tissues can be damaged and the tongue inadvertently pushed posteriorly, causing obstruction. A nasopharyngeal airway may be used for airway patency if there is no evidence of head and midface trauma. This airway is measured from the nares to the tragus of the ear.
In a child who requires continuous airway maintenance, endotracheal intubation using rapid-sequence induction (RSI) is necessary. RSI is “a technique in which a potent sedative or induction agent is administered virtually simultaneously with a paralyzing dose of a neuromuscular blocking agent to facilitate rapid tracheal intubation.”9 This procedure must be undertaken by a health care professional skilled in pediatric intubation. The orotracheal route is preferred because the nasotracheal route can be difficult or contraindicated in severe facial trauma or basilar skull fracture.
Before the intubation attempt, cardiac and pulse oximetry monitoring devices are placed on the child. Sedating medications followed by paralyzing agents are administered while the child’s lungs are ventilated with 100% oxygen. After the trachea is intubated, observe for rise and fall of the chest, auscultate breath sounds bilaterally in the midaxillary line, then over the epigastrium; listen high in the axilla because breath sounds are easily transmittable across the thin chest wall. Right mainstem bronchus intubations are a common complication with pediatric intubation; therefore bilateral chest wall movement should be observed during ventilation with a bag-mask device. Movement is best assessed by standing at the foot of the bed and watching the chest rise and fall during ventilation. Correct endotracheal tube placement is determined through auscultation of equal, bilateral breath sounds in all fields; observation of condensation in the endotracheal tube; and assessment of end-tidal carbon dioxide measurements with pediatric-specific equipment, while evaluating the child’s response. Final confirmation is made by chest radiograph. The tube must be secured with commercially available holders, tape, or ties and the measurement of the tube at the lip line documented. The tube should not press on the corner of the mouth (nares with nasotracheal intubation) because of the potential for tissue breakdown. Frequent suctioning may be necessary if aspiration is suspected or injury to the airway or lung tissue has occurred.
Children are diaphragmatic breathers, so compression on the diaphragm impedes lung expansion. A gastric tube is inserted to relieve gastric distension. The preferred method is to insert the tube orally. The tube should not be inserted nasally if the child has obvious facial trauma or signs of a basilar skull fracture. After the tube is inserted, it is taped to the child’s face and connected to low intermittent suction.
Cricothyrotomy and tracheostomy are reserved for severe cases of airway instability from facial, head, and neck trauma. Fortunately, these procedures are rarely required in children.
Strategies to protect the cervical spine in the multiply injured child include application of a rigid cervical collar and cervical immobilization devices. Care must be taken to prevent cervical spine flexion from the cervical collar or backboard (Figure 28-1). Movement can worsen spinal cord injury (SCI) and compromise the airway. Spinal protection is maintained until radiographic and clinical evidence demonstrate that SCI is not present.
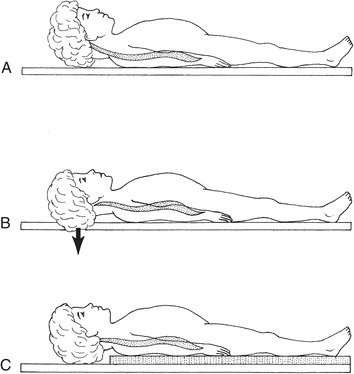 |
| FIGURE 28-1 A, Young child immobilized on a standard backboard; note how the large head forces the neck into flexion. Backboards can be modified by an occiput cutout (B) or a double mattress pad (C) to raise the chest. (From Roberts JR, Hedges JR: Clinical procedures in emergency medicine, ed 4, Philadelphia, 2004, WB Saunders.) |
Use of an appropriately sized cervical collar is essential to prevent SCI and airway compromise. A collar that is too large pushes the jaw backward, causes airway obstruction, and allows the child to move the head from side to side, which prevents cervical spine control. A collar that is too small does not provide appropriate alignment and may cause airway compromise from constriction. A cervical collar fits properly if the chin rests securely in the chin holder, the collar is beneath the ears, and the upper part of the sternum is not covered.
Infants and young children may arrive in the ED secured in their car safety seat. Children can initially remain in their car seats if there are no signs of distress and the car seat is intact. 11 Cervical protection with a collar, if possible, and towel rolls should be completed. 20 Although no evidence-based guidelines indicate that car seat immobilization is effective, it may be an option for emergency medical services personnel to transport stable, injured children. 11
Cervical spine radiographs from C1 through T1 are obtained in the anterior-posterior and lateral views to evaluate for vertebral fractures. The radiograph is assessed for vertebral symmetry, alignment, and spacing. Spinal protection can be discontinued if there is no radiographic evidence of cervical spine injury and the child has normal neurologic findings.
Breathing
Supplemental oxygen is administered to any child with multiple trauma. First, auscultate breath sounds at the midaxillary line. The child breathing spontaneously with effective air exchange can receive humidified oxygen via nasal cannula, partial nonrebreather face mask, or nonrebreather face mask.
Flow rate for a nasal cannula should be no more than 6 L/min of oxygen; higher flow rates will irritate the nasopharynx. A nasal cannula is used in children with minimal oxygen requirements. With infants and young children, it is important to secure the cannula in the nares and then initiate oxygen flow. (Remember that oxygen flow may frighten the child.) The final oxygen delivery to the patient is usually 30% to 40% through a nasal cannula. 24 A partial rebreathing mask set at a flow rate of 10 to 12 L/min delivers an inspired oxygen concentration of 50% to 60%. Blow-by oxygen can be used for children who do not tolerate the cannula or mask.
Nonrebreather oxygen masks are used for a child with greater oxygen requirements; flow rate is set at 10 to 12 L/min. A properly fitting face mask fits snugly on the face, covering nose and mouth without covering eyes or cheeks. In the child who is not breathing spontaneously or effectively, ventilations are assisted with a bag-mask device set at 15 L/min, which allows oxygen delivery up to 90%. 24 A bag-mask device needs to be self-inflating, in case there is no oxygen source available. Bag-mask devices are equipped with pop-off valves to avoid delivery of high pressures while bagging the patient. 24 When ventilations are assisted with a bag-mask device, the bag is squeezed until enough air volume is delivered to allow easy rise and fall of the chest. Care must be taken not to ventilate with extreme force because pneumothorax can occur.
A pulse oximeter sensor is applied to the child’s finger, earlobe, or toe to determine oxygen saturation. Pulse oximetry readings should be 95% or more (at sea level).
Circulation
To assess adequacy of circulation, palpate central versus peripheral pulses for quality, and assess capillary refill and skin temperature. Continuous cardiopulmonary and blood pressure monitoring devices are connected to the child immediately in a trauma situation. Vital signs should be measured every 5 minutes until the child’s condition stabilizes. Blood pressure readings should be evaluated against other vital signs. A properly fitting blood pressure cuff fits two thirds of the upper arm. A cuff that is too small gives false-high readings, whereas a cuff that is too large gives false-low readings.
It is important to apply direct pressure to open, bleeding wounds. Tourniquets are not recommended because direct tissue damage may occur.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
