CHAPTER 28. Electrical, Thermal, and Inhalation Injuries
Janet Barber Duval and with contributions by Patrick E. Besant-Matthews
Electrical and thermal injuries are capable of causing extensive tissue trauma and death. Forensic nurses must understand the various types of burns and their effects on human tissue. This information is vital for forensic investigators who must gather the physical evidence required to reconstruct the forensic scenario and to help law enforcement and judicial teams in deciding whether the injuries or death were results of accidents, suicidal intentions, or malfeasance. The sources of thermal agents, chemical agents, or electrical energy must be considered in context of the history of injury. An important part of the forensic analysis is determining whether or not the history of the incident and the resulting tissue injury seems to logically coincide.
Electrical burns and lightning strikes pose unique problems at either the accident or death scene. The pathophysiology of electrical injuries and their associated wounds will be considered, along with the characteristic wounds they produce. On-scene safety, of course, is a major concern for the forensic team.
Thermal Burn Wounds
Classifications
Burn wounds are typically classified according to the damage they create to tissue. Formerly the classifications related to degrees of burned tissue. First-degree burns affect only the epidermis and the patient experiences redness and pain; second-degree burns impact the dermis, too, and are additionally characterized by the formation of blisters. Third-degree burns involve the subcutaneous tissue. A fourth-degree burn is associated with deep tissue loss. The current, more popular burn classification refers only to partial thickness or superficial burns (first and second degree) or full thickness (third degree) associated with whitish skin changes, charring, or, ultimately, deep tissue loss (fourth degree).
Direct skin contact with hot objects such as curling irons, cigarettes, radiators, or hair dryers easily results in full-thickness burns. Differentiation of accidental burns from those intentionally induced by caretakers is based on the pattern of the burn. Accidental burns have uneven patterns of contact as the victim quickly pulls away from the hot object; a regular, even pattern of injury typically indicates that the individual was purposefully pressed again the object for an extended period of time (Olshaker, Jackson, & Smock, 2007).
Scalding burns
These hot liquid–related burns are divided into three classifications: immersion, splash or spill, and exposure to steam. These can be either accidental or deliberately induced (e.g., human abuse or torture). It takes up to six hours of continuous contact to produce a burn with low water temperatures at 111°F; however, at 130°F water can cause full-thickness burns in only 10 seconds. At 140°F, burns may occur after only a second (Olshaker, et al., 2007). Patterned burn injuries are easily detectable by experienced forensic personnel (Geberth, 2006). Scalding and immersion are commonly associated with child abuse. These are characterized by burns of the lower extremities, the buttocks, or perineal areas from dipping the child into hot water. There may be irregularities at the demarcation zone from splashing actions of the victim in an attempt to escape the scalding water. Although circumferential burns are invariably associated with intentional acts of abuse, elderly individuals or those with altered sensory perception may accidentally suffer immersion burns from scalding water in a sink or bathtub. There is a uniform degree of burn, the margins are distinct, and there are seldom any related satellite splash marks (Fig. 28-1).
Burns with Inhalation
Even though the patient’s visible burns may be dramatic, it is imperative that forensic nurses in the prehospital and emergency department settings perform a thorough assessment for signs and symptoms of inhalation injury, because its contribution to morbidity and mortality may be greater than the burn wounds on other parts of the body. All clothing, even though it may have been extensively damaged in the fire or explosion, should be salvaged. It often provides valuable clues about the nature of the fire and the presence of any accelerants or volatile chemicals that might have been present at the scene. Any burn victim should have all body surfaces thoroughly inspected, and photographs should be obtained initially and periodically postburn to record evidence about the burn wounds. Other evidentiary specimens may include blood, sputum, bronchial washings, and swabs from the nasal and oral cavities.
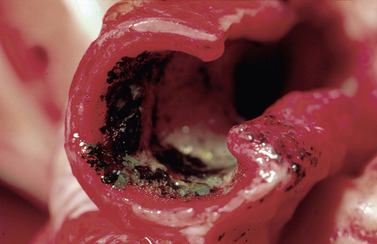
It is vital to determine the exact environment where the burn occurred. Many victims of smoke inhalation are firefighters and industrial workers who are exposed to products of combustion in confined or poorly ventilated spaces. The upper airway is damaged from toxic fumes, superheated gases, and irritating substances, both dry and moist. Facial burns, singed nasal hair, and carbonaceous deposits in the airway and sputum are hallmarks of inhalation injury, but the absence of these does not rule out inhalation injury. Factors such as blistering, edema, thick saliva accumulation, and glottic closure can lead to partial or complete airway obstruction. In living victims of inhalation injury, stridor, hoarseness, difficulty speaking, and chest retractions point to upper airway injury. Laryngospasm and sloughing of tissue may be present with severe exposures (Fig. 28-2).
The nose and mouth should be examined for soot and singed hairs. Sputum may be sooty; the patient may be hoarse and subjectively complain of difficulty swallowing and shortness of breath. A chest x-ray should be obtained as a baseline, but the initial film may be normal. Positive findings such as lung infiltrates, pulmonary edema, and other indications of inhalation damage do not become obvious for a day or two. If the victim becomes cyanotic, upper airway obstruction resulting from chemical insults and edema should be suspected (Lanros & Barber, 1997). Circumferential burns of the neck and chest with edema and eschar will also contribute to respiratory compromise by mechanically obstructing airflow and limiting chest excursions, respectively. If there is prolonged exposure to high concentrations of toxic fumes or irritating substances, the lower airways are also damaged.
In living fire victims, such conditions as tracheobronchitis, bronchospasm, bronchorrhea, and pulmonary edema can be observed if irritation has extended deep into the tracheobronchial structures. Bronchial blood flow will intensify, and the edema in the airways and alveolar tissue may be aggravated. Other problems include surfactant dysfunction, increased lung water, decreased lung compliance, increased airway resistance, and increased pulmonary vascular resistance leading to ventilation-perfusion (V/Q) mismatching and an increase in physiological dead space, which decreases the PaO 2, increases the P(A-a)O 2, and increases the necessary minute ventilation to normalize the PaCO 2. The central nervous system and myocardium respond to reductions in oxygen transport and its use at the cellular level; oxygen cannot exit readily from the hemoglobin, and the oxyhemoglobin dissociation curve shifts to the left. The anemia and hypoxia persist despite favorable plasma PaO 2. Cerebral edema occurs from hypotension and the impaired oxygen transport. In some cases, there is cell death resulting from the presence of certain toxins.
If the individual is encountered in an unconscious state, there is a high likelihood of carbon monoxide and hydrogen cyanide poisoning. First responders, forensic personnel, and emergency department staff must be able to promptly recognize the classic indices of these two life-threatening inhalation-related poisonings.
Carbon monoxide poisoning
This toxic inhalation injury occurs when individuals breathe the products of incomplete carbon combustion. Examples of where such fumes may be present include automobile exhaust and confined areas where gas-flame heating units and charcoal grills are used. Because carbon monoxide (CO) has a 200 times greater affinity for hemoglobin than oxygen, it will preferentially bind, thus limiting oxygen availability. Furthermore, studies indicate that CO may also bind to myoglobin and cytochrome oxidase, thus interfering with intracellular respiration (Ayres, Grenvik, Holbrook, & Shoemaker, 1995). If a fire or smoke-inhalation victim is pregnant, it is important to recall that carbon monoxide is readily taken up by a fetus because the fetal hemoglobin has even more affinity for CO than does the typical child or adult. Even at low levels of exposure to carbon monoxide, pregnant patients and their unborn are at significant risk. Blood should be drawn to determine carboxyhemoglobin levels (the normal level is 0 to 5 ppm). In living patients, arterial blood gases may reveal a low partial pressure of oxygen (PO 2) and a high partial pressure of carbon dioxide (PCO 2) in the blood (Levine & Fromm, 1995).
The patient with CO poisoning cannot be properly evaluated with a pulse oximeter because oxyhemoglobin and carboxyhemoglobin have similar light absorption spectra. The documented pulse oximetry reading will be falsely elevated in carbon monoxide poisoning. Arterial blood gases are also unreliable because PO 2 is a measurement of the partial pressure of oxygen in millimeters of mercury, not of the oxygen saturation of hemoglobin (Ayres, et al., 1995). Carboxyhemoglobin spectrophotometry is the standard measurement for CO poisoning. Handheld carbon monoxide breath analyzers have also been shown to be highly reliable (Cunnington & Hormbrey, 2002).
The clinical manifestations of CO poisoning are obscure until the blood level reaches 20% to 40%. Up to that point, only mild headache and exercise-induced angina (in susceptible individuals) occur. However, at higher levels, these symptoms worsen and vomiting, muscular weakness, visual disturbances, dizziness, and impaired judgment are noted. Tachypnea, tachycardia, seizures, syncope, and irregular breathing follow when levels reach 40% to 60%. Above 60%, shock, coma, apnea, and death occur. The classic “cherry-red skin” sign of CO poisoning is an unreliable determinant of this life-threatening condition.
Burn victims, rescuers, and forensic personnel with suspected smoke inhalation injury should promptly receive 100% oxygen. Accumulated CO is eliminated through the lungs. The half-life of CO in room air is three to five hours; with 100% oxygen administration, it is 30 to 90 minutes. Hyperbaric therapy is used in some severe cases, but no controlled studies confirm its superiority to regular modes of oxygen therapy for the majority of patients. Considerations for its use include coma, cardiovascular involvement, pregnancy, and carboxyhemoglobin levels >40%.
Cyanide poisoning
Cyanide is extensively used in industrial and agricultural applications and is liberated in fires by the burning of wool, silk, nylon, and polyurethanes. It also occurs naturally in some plants and in fruit pits. Hydrogen cyanide gas has been associated with suicides, judicial executions, and mass executions (e.g., Nazi extermination camps, Jonestown massacre). Because cyanide can be inhaled, injected, ingested, or absorbed through intact skin and mucous membranes, it is of great concern in any extensive fire or a terrorist-related event such as the World Trade Center bombing in 2001.
Detection of the presence of cyanide is usually swift by noting the smell of bitter almonds, a hallmark of cyanide poisoning. However, only about 65% of all humans can detect this scent (Ayres, et al., 1995). On contact, it produces eye irritation and a burning sensation. Exposed individuals should be removed from any confined space and placed in fresh air. Mouth-to-mouth respiration should not be attempted because of risks to the rescuer. Cyanide is readily absorbed, so unprotected skin and mucous membranes must be flooded immediately with copious amounts of water to minimize systemic effects. Clothing should be placed in impervious containers and distinctively marked “hazardous” to prevent accidental exposure by other forensic investigators. Prompt emergency care at the hospital is essential to minimize cyanide’s potentially lethal effects (Haddad, Shannon, & Winchester, 1998).
Effects from cyanide poisoning can be immediate in confined spaces; in low-level exposures where fresh air is abundant, symptoms are usually delayed. Initially, the patient with cyanide poisoning exhibits nonspecific signs and symptoms including anxiety, agitation, flushing, tachycardia, tachypnea, and dizziness. Seizures, metabolic acidosis, coma, and death will rapidly ensue without specific emergency interventions. Definitive treatment includes respiratory support with supplemental oxygen and prompt use of the agents contained in a typical emergency “cyanide kit,” which includes nitrite, sodium nitrite, and sodium thiosulfate.
First responders, forensic investigators, and hospital personnel should wear protective clothes when dealing with suspected cyanide poisoning cases because skin, pulmonary structures, stomach contents, and other body fluids can contain the agent. This caution applies to both living and deceased victims.
A routine hospital autopsy sparked a hospital alert and a hazardous materials response when the stomach of the deceased was incised to facilitate examination of the contents. Potassium cyanide gas was released into the room. Personnel immediately experienced the agent’s classic bitter almond odor, along with headache, dizziness, and respiratory distress. Personnel took immediate action to ensure that airflow in the autopsy area was isolated and then reported promptly to the emergency department for further assessment. No personnel suffered serious injuries from the brief exposure. It was later learned that the deceased individual had intentionally ingested the potassium cyanide to commit suicide.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access