Skill 26
Epidural Analgesia
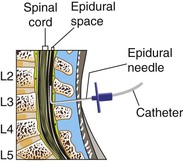
Administration of analgesics into the epidural space is an efficient intervention to manage acute pain (D’Arcy, 2011). The epidural space is a potential space that contains a network of vessels, nerves, and fat located between the vertebral column and the dura mater, the outermost meninges covering the spinal cord (Fig. 26-1). Analgesics delivered into this space are distributed by (1) diffusion through the dura mater into the cerebrospinal fluid (CSF), where they act directly on the receptors in the dorsal horn of the spinal cord; (2) circulation of blood vessels in the epidural space, from which they are delivered systemically; and/or (3) absorption by fat in the epidural space, creating a depot where the analgesia is slowly released systemically.
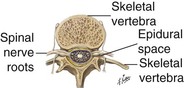
Fig. 26-1 Anatomical drawing of epidural space. (Reprinted from www.netterimages.com Elsevier, Inc. All rights reserved.)
Opioids and local anesthetics, separately or in combination, are often used in epidural analgesia. Opioids are delivered close to their site of action (central nervous system) and thus require much smaller doses to achieve the same degree of pain relief (D’Arcy, 2009; D’Arcy, 2011). Common opioids administered epidurally include morphine, hydromorphone (Dilaudid), fentanyl, and sufentanil.
A patient should be placed in the lateral side-lying or sitting position with the shoulders and hips in alignment and the hips and head flexed during insertion of an epidural catheter. An anesthesia provider places a catheter into the epidural space below the second lumbar vertebra, where the spinal cord ends (Fig. 26-2). However, epidurals may also be placed at the thoracic level of the spinal cord. Catheters intended for temporary or short-term use are not sutured in place and exit from the insertion site on the back. A catheter intended for permanent or long-term use is “tunneled” subcutaneously and exits on the side of the body (Fig. 26-3) or on the abdomen. Tunneling reduces the risk for infection and catheter dislodgement. A sterile occlusive dressing covers the catheter exit site and is secured to the patient. An x-ray film is the only way to confirm epidural catheter placement.
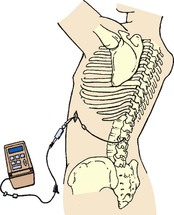
Fig. 26-3 Epidural catheter attached to ambulatory infusion pump. (Image courtesy Astra Zeneca Pharmaceuticals, Wilmington, Del. All rights reserved.)
The use of epidural opioids requires astute nursing observation and care. The catheter poses a threat to patient safety because of its anatomical location, its potential for migration through the dura, and its proximity to spinal nerves and vessels (Pasero and McCaffery, 2011). Catheter migration into the subarachnoid space can produce dangerously high medication levels. Monitor a patient’s motor and sensory function, including any onset of urinary retention. You should not administer other supplemental opioids or sedatives when patients have been administered an epidural because the combined effect may cause respiratory depression. In many health care agencies anesthesiologists and nurse anesthetists are the only health care providers who may initiate epidural opioid infusions or administer a medication bolus.
Delegation Considerations
The skill of epidural analgesia administration cannot be delegated to nursing assistive personnel (NAP). The nurse directs the NAP to:
▪ Immediately report to the nurse any change in level of consciousness.
▪ Report any catheter disconnection immediately.
▪ Immediately report to the nurse any change in patient status or comfort level.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree