CHAPTER 26. Burns
Cheryl Wraa
Burn trauma continues to be an immense challenge to caregivers in the emergency department (ED), playing a critical role in the care of the burn patient. Every year in the United States an estimated 500,000 patients are treated in the ED for burn injury. Of these, approximately 4000 die with the majority of deaths, approximately 3500, due to residential fires. The majority of deaths, approximately 75%, occur at the scene or during initial transport. Admissions to the hospital due to burn injury number approximately 40,000 annually in the United States with more then 60% being admitted to hospitals with specialized burn centers. Decreases of burn incidence and hospitalization are attributed to fire and burn prevention education, regulation of consumer products, and implementation of occupational safety standards. The recent decline in mortality is attributed to early excision and closure of the burn wound. Other factors contributing to the decline are management of burn patients in specialty burn units, improved resuscitation, control of infection, and support of the hypermetabolic response. A significant portion of morbidity and mortality associated with burn injuries is due to associated injuries. Pulmonary pathology from inhalation injury is the major cause of burn trauma death, with the majority of deaths at the extremes of age. Burn injury and deaths associated with fires are the third leading cause of accidental death in children between the ages of 1 and 14 years. 2.3.4.5.7.14. and 16.
More than 90% of all burns are considered preventable. Education, particularly in the school-age population, combined with legislative efforts is helping decrease the number of burn injuries. The American Burn Association has developed effective public education programs. Legislation has been enacted that requires smoke alarms and sprinkler systems in public buildings, hotels, apartments, and new homes. For the caregiver an accurate classification of injury, timely intervention, and rapid transport to an appropriate burn facility significantly reduces burn injury mortality and morbidity. 5
ETIOLOGY
Not all burns are caused by fire. Tissue damage may be secondary to chemicals, hot liquids, tar, electricity, lightning, or frostbite. The location and duration of exposure to the source affects outcome, regardless of the specific source of burn injury. Specific mechanisms of burn injury are described in the following sections.
Thermal Burns
Thermal injuries represent the majority of all burns. They may result from flame, flash, steam, or scalding liquid. Figure 26-1 presents example of one cause of burn injury.
 |
| FIGURE 26-1 Burn injuries occur as a result of exposure to flame and smoke. (Courtesy Tacoma Fire Department, Tacoma, Wash.) |
Scald Burns
Scalds from hot liquids are the most common cause of all burns. Exposure to water at 140° F (60° C) for 3 seconds can cause a deep partial-thickness or full-thickness burn. If water is 156° F (69° C), the same type of burn occurs in only 1 second. As a comparison, fresh brewed coffee is about 180° F (82° C). Tap water scalds occur within seconds and often happen during routine activities, involve large body surface area (BSA) burns, and are the most common source of scald-related deaths. 14 Soups and sauces, which are a thicker consistency, remain in contact longer with the skin and cause deeper burns. Other liquids that cause scalds are cooking oil and grease. When used for cooking, oil and grease may reach 400° F (204° C). Immersion burns are usually deep and severe because of prolonged contact with a scalding liquid.
Specific groups of patients at risk for scald burns include those with preinjury comorbidities such as neurologic impairment, diabetes, and the extremes of ages. Adults older than 60 years disproportionately suffer burns from hot liquids. 1 The fact that older patients are at high risk for burn injury and experience worse prognoses than younger patients is well documented. This has been attributed to their compromised physical health status with chronic, debilitating conditions that increase the risk, exacerbate the extent of the injury, and impair recovery. 14
Flame Burns
Burns from flames are the next most common cause of burns. Fortunately, the number of house fires has decreased with increased use of smoke detectors. Most flame burns are caused by careless smoking, motor vehicle crashes, and clothing ignited from stoves or space heaters. Flame burns that occur outdoors are usually secondary to misuse of cooking stoves fueled by white gasoline, lanterns in tents, smoking in a sleeping bag, and gasoline or kerosene used in a charcoal fire. 4
Flash Burns
Explosions of natural gas, propane, gasoline, or other flammable liquids cause flash burns—the third most common type of thermal burn. The explosion causes intense heat for a very brief time. Flash burns are usually partial thickness, although depth is dependent on the amount and kind of fuel that explodes. Flash burns can be large and are often associated with significant thermal damage to the upper airway. 4
Contact Burns
Contact with a hot object such as metal, plastic, glass, or hot coals results in contact burns. The burns are usually not extensive but tend to be deep. People involved in industrial accidents often have contact burns associated with crush injuries from machine presses or hot, heavy objects. An increased incidence of contact burns has been seen in toddlers secondary to the increased use of wood-burning stoves. The most common injury is to the palm when a child falls against the stove with hands outstretched. 4
Electrical Burns
As electricity passes through the body and meets resistance from body tissues, it is converted to heat in direct proportion to amperage and the body’s electrical resistance. It initially passes through the skin, causing an external burn at the entry and exit sites, with extensive damage internally between these sites. Nerves, blood vessels, and muscle are less resistant and more easily damaged than bone or fat. The heart, lungs, and brain can sustain immediate damage. The nervous system is particularly sensitive to electrical burns. Damage to the brain, spinal cord, and myelin-producing cells causes devastating transverse myelitis. Autonomic dysfunction can cause pupils to appear fixed and dilated, but this finding should not cause resuscitation efforts to stop. The smaller the body part through which the electricity passes, the more intense the heat and the less it is dissipated. Consequently, extensive damage can occur in the fingers, hands, forearms, toes, feet, and lower legs. If the path is near or through the heart, damage to the heart’s electrical conduction system can cause spontaneous ventricular fibrillation or other dysrhythmias. Papillary muscle damage may lead to sudden valvular incompetence and cardiac failure. Alternating current is more likely to induce ventricular fibrillation than direct current.
Most lightning injuries do not traverse the body but flow around it, creating a shock wave capable of causing fractures and dislocations. Close to two thirds of patients sustain a ruptured eardrum. About 70% of patients who survive a lightning strike complain of paresthesia or paralysis. Fortunately, both conditions are usually temporary. 2.4. and 16.
Chemical Burns
Chemicals cause a denaturing of protein within the tissues or a desiccation of cells. Chemical concentration and duration of exposure determine extent of the burn. Alkali products usually cause more tissue damage than acids. A wet chemical should be removed as soon as possible by flushing with copious amounts of water. Dry substances should be brushed off the skin before the area is flushed. Care must be taken not to expose the caregiver to the chemical during this procedure. All fluids used to decontaminate the patient should be contained; the fluid should not be allowed to drain into the general drainage system. Chemical burns can be deceiving as to depth; appearances can be similar in surface discoloration until tissue begins to slough days later. Consequently, all chemical burns should be considered deep partial thickness or full thickness until proven otherwise. After chemical removal, wounds are managed in the same manner as thermal burns. 3. and 4.
Frostbite
Frostbite is actual freezing of tissue from exposure to freezing or below-freezing temperatures. In a cold environment the body attempts to maintain heat by vasoconstriction of peripheral blood vessels to reduce heat exchange. The longer the period of exposure, the more peripheral blood flow is reduced. When extremities are left unprotected, intracellular and extracellular fluids can freeze, forming crystals that damage local tissues. Blood clots may form and impair circulation to the area.
Signs, symptoms, and classification of frostbite are the same as thermal burns. The affected extremity should be rapidly rewarmed using warm water. Use of excessive heat such as steam is dangerous and can cause unnecessary damage. Dress the rewarmed extremity and immobilize it with a padded splint. As with flame burns, frostbite can be very painful, so pain management is needed. 3. and 4. For a more extensive review of frostbite, see Chapter 40.
Cold immersion of the foot or hand is a nonfreezing injury that occurs from chronic exposure to wet conditions at temperatures just above freezing. The extremity may appear black, but deep tissue destruction may not be present. Initially there is an alternating arterial vasospasm and vasodilation with the tissue first cold and numb, progressing to hyperemia in 24 to 48 hours. As the injury progresses to hyperemia, the patient experiences intense burning sensation and dysesthesia. Tissue damage occurs with resultant edema, blistering, redness, ecchymosis, and ulcerations. Attention to hygiene will prevent local infection, cellulitis, or gangrene. 3
Patients who have exposure to chronic repetitive damp cold may develop chilblain, or pernio. This is a dermatologic condition that usually occurs on the face, dorsum of the hands and feet, or any area chronically exposed to a cold environment. Signs and symptoms include pruritic, reddened skin lesions that with continued exposure, ulcerate or develop hemorrhagic lesions that progress to scarring, fibrosis, or atrophy with itching, tenderness, and pain. Symptoms are controlled by protection from further exposure, and the use of antiadrenergics or calcium channel blockers. 3
BURN ASSESSMENT
Burn depth and extent are assessed to determine the severity of burn injury. In many cases final determination is not made for several days.
Depth of Burn
Burns are described as partial thickness or full thickness. Identification of the depth of injury may be difficult initially because depth may actually increase over time as edema forms and circulation to the area of injury is compromised. This process usually peaks at 48 hours; therefore a more accurate determination of depth can be made between 48 and 72 hours. Depth determination is not a priority during initial resuscitation.
Extent of Burn
Extent of injury for thermal and chemical injuries is assessed by using formulas such as the rule of nines (Figure 26-2), Berkow formula, or Lund and Browder table (FIGURE 26-3 and FIGURE 26-4). The caregiver should remember that the rule of nines must be modified for children. As noted in Figure 26-2, B, the head and neck of an infant represent 18% of BSA, whereas legs represent 14% for each lower extremity. To correct for age 1% is subtracted from the head for each year of age through 10 years, and 0.5% is added to each lower extremity. To estimate scatter burns, the size of the patient’s palm (including fingers) is used to represent 1% of total BSA (TBSA). The palm is visualized over the burned areas. To obtain a more accurate estimate of the extent of burns, both burned and unburned areas are calculated. The two estimates should then be compared. If the total is more or less than 100%, the areas should be reestimated. Assessing extent of injury in electrical burns is more difficult because surface damage is minimal when compared with underlying damage. When discussing an electrical injury, describing the injury anatomically is more important than calculating percentage of BSA burned.
 |
| FIGURE 26-2 Rule of nines. A, Adult. B, Child. ( A from Ignatavicius DD, Workman LM: Medical-surgical nursing: critical thinking for collaborative care, ed 5, Philadelphia, 2006, WB Saunders. B from Sole ML, Klein DG, Moseley MJ: Introduction to critical care nursing, ed 4, Philadelphia, 2005, WB Saunders.) |
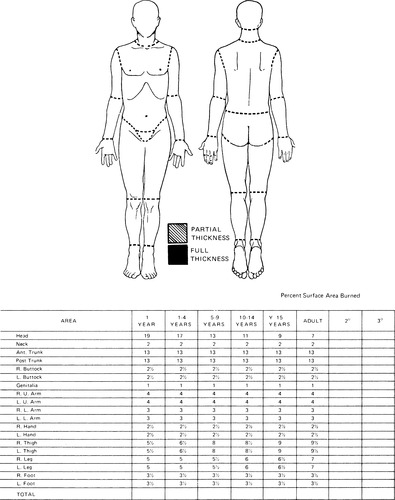 |
| FIGURE 26-3 Lund and Browder formula. (From Cornwell P, Gregory C: Management of clients with burn injury. In Black J, Hawks J, editors: Medical-surgical nursing, ed 7, St. Louis, 2005, Elsevier.) |
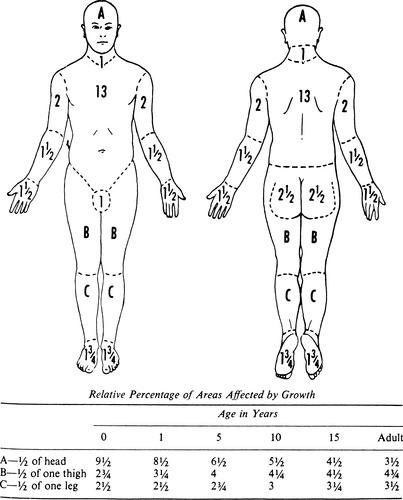 |
| FIGURE 26-4 Lund and Browder formula. (From Artz CP, Moncrief JA: The treatment of burns, ed 2, Philadelphia, 1979, WB Saunders.) |
Severity of Burn
The severity of burn injury is based on assessment of extent and depth of injury, patient age, presence of concomitant injuries, smoke inhalation, and preexisting diseases. The American Burn Association’s guidelines for classification of severity of burn injuries are listed in Table 26-1.
| DPT, Deep partial thickness; SPT, shallow partial thickness; TBSA, total body surface area. | ||
| Classification | Characteristics | Treatment Facility |
|---|---|---|
| Minor | SPT DPT, <15% TBSA adult <40 years of age | Outpatient or inpatient (for 24 hr) |
| DPT, <10% TBSA adult >40 years of age | ||
| <10% TBSA burn in children <10 years of age | ||
| With <2% TBSA full-thickness burn and no cosmetic or functional risk to the face, eyes, ears, hands, feet, or perineum | ||
| Moderate | DPT, 15% to 25% TBSA adult <40 years of age | Community hospital |
| DPT, 10% to 20% TBSA adult >40 years of age | ||
| 10% to 20% TBSA burn in children <10 years of age | ||
| With <10% TBSA full-thickness burn without cosmetic or functional risk to the face, eyes, ears, hands, feet, or perineum | ||
| Major | DPT, 25% TBSA adult <40 years of age | Burn center |
| DPT, 20% TBSA adult >40 years of age | ||
| 20% TBSA burn in children <10 years of age | ||
| Burns of face, eyes, ears, hands, feet, and perineum | ||
| Burns with concomitant inhalation injury or major trauma | ||
| All major electrical injuries | ||
Care of patients with burns of different severity is determined by availability of specialized care facilities. Initial stabilization of the burn patient should be available in any community hospital with 24-hour emergency capabilities. Patients with minor burns may be treated as outpatients or admitted to the community hospital. Patients with moderate burns may be treated in a community hospital with appropriate staff and facilities to deliver burn care or transferred to a specialized burn care facility. Patients with major burns require care in a specialized burn care facility. Transfer agreements with special-care units should be developed in advance to facilitate timely and uneventful transfer. 11Box 26-1 summarizes criteria for transfer to a burn center. Any patient with concomitant trauma that poses increased risk for morbidity or mortality should be treated in a trauma center until he or she is stable and then transferred to a burn center as appropriate.
Box 26-1
C riteria for T ransfer to a B urn C enter
1. Partial-thickness and full-thickness burns greater than 10% total body surface area (TBSA) in patients less than 10 years or over 50 years of age.
2. Partial-thickness and full-thickness burns greater than 20% TBSA in other age groups
3. Burns that involve the face, eyes, ears, hands, feet, genitalia, perineum, or major joints.
4. Full- thickness burns greater than 5% TBSA in any age-group.
5. Electrical burns, including lightning injury.
6. Significant chemical burns.
7. Inhalation injury.
8. Burn injury in patients with preexisting medical disorders that could complicate management, prolong recovery, or affect mortality.
9. Any patient with a burn injury that has concomitant trauma poses an increased risk of morbidity or mortality, and may be treated initially in a trauma center until stable before being transferred to a burn center.
10. Children with burn injuries in hospitals without qualified personnel or equipment for the care of children.
11. Burn injury in patients who will require special social, emotional, or long-term rehabilitative intervention, including cases involving suspected child abuse and neglect.
Data from American College of Surgeons: Advanced trauma life support student manual, Chicago, 2008, The College.
PATHOPHYSIOLOGY
Burn injury occurs when skin is exposed to more energy than it can absorb. The cause of the burn may vary, but local and systemic responses are generally similar. To understand the pathophysiology of burns, one must first understand the functions of the skin, which consists of two layers: the epidermis and the dermis. The epidermis, the outer layer of the basement layer of cells, consists of cells that migrate upward to become surface keratin. The dermis, or inner layer, consists of collagen and elastic fibers and contains hair follicles, sweat and sebaceous glands, nerve endings, and blood vessels. The skin is the largest organ of the body and acts as an infection barrier, vapor barrier, and a heat regulator. 4. and 5.
Three zones of tissue damage occur at the burn site. First is the central zone of coagulation, an area of irreversible damage. Concentrically surrounding this area is the zone of stasis, where capillary and small vessel stasis occurs. The ultimate fate of the burn wound depends on resolution or progression of the zone of stasis. Edema formation and prolonged compromise of blood flow to this area cause a deeper, more extensive wound; therefore depth and severity of burn wounds may not be known for 2 or more days after the initial injury. The third zone of damage is the zone of hyperemia, an area of superficial damage that heals quickly on its own. 5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
