CHAPTER 25. Orthopedic and Neurovascular Trauma
Mary Jo Cerepani
Musculoskeletal injury is one of the most common types of trauma seen in the emergency department (ED) and is a significant cause of disability. Primary mechanisms for these injuries include motor vehicle crashes (MVCs), assaults, falls, sports and recreation, and injuries sustained at work or home. Bone, soft-tissue, and associated neurovascular injuries are rarely emergent unless accompanied by a life-threatening hemorrhage as in certain amputations and pelvic fractures. Fractures and soft-tissue injuries are primarily designated as urgent because of potential neurovascular injury with resultant limb disability and pain. Early intervention enhances preservation of limb and function. This chapter focuses on common orthopedic and neurovascular extremity injuries and appropriate therapeutic interventions. Related anatomy and physiology are briefly reviewed.
ANATOMY AND PHYSIOLOGY
The musculoskeletal system and related neurovascular structures consist of bones, joints, tendons, ligaments, muscles, vessels, and nerves. The skeletal system contains 206 bones, which provide support, strength, movement, and protection to the body and organs. Bones store a number of minerals, including calcium and phosphorus, and are involved in blood cell production. Bones are characterized by shape as long, short, flat, or irregular with the shape of a particular bone suited for a unique function or purpose. The skeleton is composed of two types of bones: cancellous and cortical. Cancellous (spongy) bone is found in the skull, vertebrae, pelvis, and long-bone ends. Cortical (dense) bone is found in the long bones. Bones are supplied by blood vessels, nerves, and lymphatic vessels that nourish bone tissue and allow the bone to repair injuries. The periosteum covers the bones and provides a point for attachment of muscle, as well as the blood supply for underlying bone tissue.
Bone is connected to other bone by stabilizing bands of elastic, fibrous connective tissue called ligaments. Nonelastic fibrous cords that connect muscle to bone are tendons. Dense connective tissue found between the ribs, in the nasal septum, ear, larynx, trachea, bronchi, between vertebrae, and on articulating surfaces is known as cartilage. Cartilage has a limited vascular supply, whereas bone tissue has abundant vascular structures.
Joints are classified as nonsynovial (immovable and slightly immovable) and synovial (freely movable). Synovial joints have two articulating surfaces covered with cartilage and are surrounded by a two-layered synovial membrane sac. The entire joint is encapsulated by dense, ligamentous material. Joints provide mobility and stability, flexion and extension, medial and lateral rotation, and abduction and adduction. Joint movement is enhanced by muscles and ligaments that overlie the joint.
Nerves and arteries lie in close proximity to bones and muscle groups, with arterioles distributed throughout the periosteum to provide nutrients. Nerves provide sensation and movement. The closeness of arteries and nerves to bone structures increases their risk for injury with trauma to soft tissue, muscles, bones, or joints.
PATIENT ASSESSMENT
Assessment of orthopedic trauma begins with assessment of the airway, breathing, and circulation (ABCs). Rapid assessment identifies major injuries of the head, cervical spine, chest, and abdomen and prioritizes essential interventions. After ensuring that no life-threatening injury has been left unattended, the nurse assesses and stabilizes any extremity injuries. Assessment of orthopedic injuries includes inspecting for edema, obvious deformity, presence of contusions, abrasions, lacerations, or puncture wounds and palpating for crepitus and point tenderness. A focused neurovascular evaluation is conducted for any injuries identified, noting the presence and/or absence of pain, pulses, paralysis, paraesthesia, pallor, temperature, and capillary refill. 6
Before immobilization, open fractures should be stabilized and bleeding controlled. Open fractures with obvious bone protrusion or a deep laceration should be rinsed with sterile normal saline to remove gross contamination and covered with a dry sterile dressing.
Puncture wounds over a fracture site should not be irrigated because this can force bacteria deeper into the wound. Reduction of an open fracture should not be attempted in a prehospital setting because this may force contaminants into the wound, increasing risk for infection.
To control bleeding apply pressure directly to the injury site, edges of the wound, or an adjacent pressure point. Use of a tourniquet for hemorrhage control should be considered only as a last resort (life over limb) because of potential neurovascular compromise.
Immobilization
Immobilization should be accomplished as soon as possible to minimize further damage or complications secondary to bone fragments or neurovascular injury and to reduce pain in the injured limb. A splint should include the joints above and below the injury. Neurovascular status must be checked before and after immobilization. If neurovascular status is initially compromised, gradual traction may be used to promote return of neurologic or vascular function before splinting. If neurovascular status is compromised after splinting or traction, the splint should be removed and reapplied or the traction should be decreased. Angulation should be corrected only if it prevents immobilization or if neurovascular compromise is present. Splinting is best accomplished with an assistant to support the limb while a padded splint is placed and wrapped with a noncompressive bandage. Neurovascular status is rechecked after splinting.
Four basic types of splints exist, including soft splints such as pillows; hard splints such as padded board, cardboard, aluminum, plaster, fiberglass, or a ladder splint; inflatable air splints or vacuum splints; and traction splints, which reduce angulation and provide support. 5 Common splints that are used to immobilize the thumb/finger, wrist/forearm, elbow, and lower extremities are thumb spica, volar splint, boxer splint, sugar tong, and posterior splints (Figure 25-1).
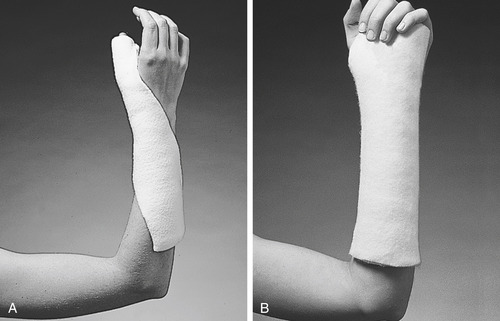 |
 |
| FIGURE 25-1 Types of splints and their indications. A, Thumb spica splint. B, Volar splint. C, Boxer splint. D, Sugar tong splint. E, Posterior splint. (Courtesy BSN Medical, Inc.) |
Air splints were used extensively when first developed because they conformed well and provided visualization of the injured extremity. However, an air splint that is not open on the distal end does not allow for neurovascular checks without deflating or unzipping the splint (Figure 25-2). An air splint should be inflated only to the point where a finger can be slipped between the splint and the skin. Excessive pressure in the splint can compromise circulation. Air splints also stick to the skin, cause irritation, and are difficult to remove in patients with excessive diaphoresis.
 |
| FIGURE 25-2 Air splint. (From Stoy W: Mosby’s EMT: basic textbook, ed 2, St. Louis, 2007, Mosby.) |
Several types of traction splints are available and are usually applied by prehospital providers. The Thomas ring splint, Sager splint, and Hare splint (Figure 25-3) are used for fractures of the midshaft of the femur or upper third of the tibia but should not be used for the hip, lower tibia or fibula, ankle, or a femur fracture with associated tibial-fibular fractures.
 |
| FIGURE 25-3 Hare traction splint. (From Marx JA, Hockberger RS, Walls RM: Rosen’s emergency medicine: concepts and clinical practice, ed 6, St. Louis, 2006, Mosby.) |
After immobilization the limb should be elevated and an ice pack applied to minimize swelling. Caution is advised because overzealous elevation may compromise arterial circulation and excessive, prolonged cold may damage tissues.
The patient should be completely disrobed and examined for anterior injuries and then logrolled to identify posterior injuries while maintaining adequate cervical spine protection. Rings should be removed if the injury involves the hand, arm, foot, or toes. Elevation and cooling measures should be maintained, and neurovascular status should be checked periodically.
Careful history should include circumstances of the injury (time and mechanism) and significant medical history, including acute and chronic alcohol use, medications, allergies, and tetanus immunization status. Time of last oral intake should be recorded, and the patient should be allowed nothing by mouth (NPO) if procedural sedation or surgical intervention is a possibility.
SOFT TISSUE INJURIES
Soft-tissue injuries generally accompany orthopedic trauma and can involve skin, muscles, tendons, cartilage, ligaments, veins, arteries, and nerves; circulation and function can be compromised from soft-tissue injury. Common injuries to the skin include abrasions, avulsions, contusions, hematomas, lacerations, and puncture wounds.
Principles of nursing care are generally the same for various soft-tissue injuries. Inspection involves checking for wounds, swelling, hematomas, and bleeding, then assessing neurovascular status. A soft, bulky dressing is applied, and swelling can be minimized with elevation and cooling measures. Radiographs are used to rule out foreign bodies and fractures. Analgesia is administered as prescribed for isolated injuries, and antibiotics are administered for significant, contaminated wounds. Written discharge instructions discuss RICE: rest, ice (e.g., apply a covered ice bag to the injury for 20 minutes every 2 to 3 hours for 24 to 48 hours), compression, and elevation. (See Chapter 11 for more specific information.)
Fingertip Injuries
Fingertip injuries are frequently seen in the ED, with the most common type being a crush injury to the distal phalanx that occurs when a heavy object falls on the finger or the digit is caught in a door. Crush injuries can also be associated with a fracture. If a hematoma forms under the fingernail, it may cause a subungual hematoma (Figure 25-4), which requires nail trephination by penetrating the fingernail over the hematoma with a nail drill, scalpel, pencil cautery, or superheated paper clip to release blood under the nail and relieve pressure. 15
 |
| FIGURE 25-4 A, Subungual hematoma. B, Subungual hematoma following trephination. (From Roberts JR, Hedges JR: Clinical procedures in emergency medicine, ed 4, Philadelphia, 2004, WB Saunders.) |
Fingertip injuries caused by a high-pressure paint or grease gun have increased in recent years. This injury occurs when a person is cleaning the gun tip and a stream of paint or grease is released into the fingertip or hand under high pressure. A pressure greater than 7000 pounds per square inch has been associated with a high amputation rate. 9 Particular attention to history and time of injury is crucial; the injury appears as a small pinhole in the fingertip but represents a serious, limb-threatening surgical emergency because material has been injected into the soft tissue of the involved limb. Treatment must not be delayed. Therapeutic intervention requires debridement of the paint- or grease-injected limb under general anesthesia.
Traumatic Amputations
Traumatic amputations occur among farm workers secondary to heavy farm machinery, in factory workers when a limb is caught by a heavy machine, and in motorcyclists when the motorcycle and driver collide with another vehicle. Other causes include snow blowers and lawn mowers. Body parts frequently amputated are digits (fingers, toes), distal half of the foot (transmetatarsal), leg (above, at, or below the knee), hand, forearm, arm, ears, nose, and penis.
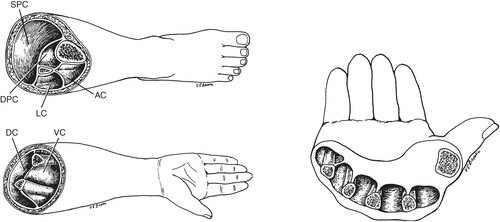
Therapeutic interventions for amputations begin with stabilization of the ABCs, including administration of high-flow oxygen, initiation of two large-bore intravenous (IV) lines, control of bleeding, and rapid transportation to a facility for definitive care. If the body part is only partially amputated, the limb should be supported and splinted in a position of anatomic function. Figure 25-5 shows anatomic hand position. A completely amputated stump should be irrigated to remove gross contamination, dressed, and elevated. Antibiotics, a tetanus booster, and tetanus immune globulin, as indicated, should be initiated in the ED.
 |
| FIGURE 25-5 Anatomic positioning of hand. (From Canale TS, Beaty JH: Campbell’s operative orthopaedics, ed 11, St. Louis, 2007, Mosby.) |
Whenever possible, the amputated part is preserved for reimplantation by wrapping it in saline-moistened gauze and placing it in a plastic bag or container. The sealed container is then placed on top of crushed ice and water. This cools the part without causing direct damage to tissue. If the amputated part is placed directly in water or on ice, cells can be damaged by water moving across the cellular membranes, including cellular freezing and death. Distilled water is not used because of its deleterious effect on tissue. Iodine should never be placed directly on the amputated part because of discoloration and its effects on tissue viability. Maintain the limb in correct anatomic position.
Reimplantation
After amputation, reimplantation may be possible. Limiting factors for successful reimplantation include availability of a reimplantation team, amount of damage to the attached and amputated parts, method of preservation of the amputated part, and time elapsed since the accident. Sharp, guillotine-like cuts have a better outcome than crush or avulsion type of injuries. Muscles can survive 12 hours of cold ischemia; bone, tendon, and skin can survive 24 hours; warm survival time is much less. 8 Predicted outcome of reimplantation is further determined by age, occupation, motivation, and general physical condition of the victim. Historically, upper extremity reimplantations are more successful than lower extremity reimplantations, and children typically have a better outcome with this type of reimplantation.
Impaling Injuries
Impaling injuries usually result from an industrial accident in which the victim falls onto a sharp, immobile object. Injuries with nails from a powered nail gun are also common. Nails used in these guns are coated with a special adhesive that can stick to tissue. Impaled objects should not be immediately removed; surgical removal may be required. Complications from this type of injury include infection and problems specific to the structures in which the object is impaled. Biologic substances such as wood carry an increased risk for infection.
Gunshot Wounds
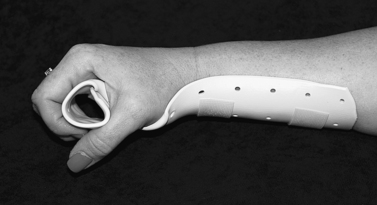
Gunshot wounds usually result from hunting or acts of violence. Tissue damage depends on the type of weapon, size of ammunition used, distance from the weapon, and part of the body injured (Figure 25-6). Tissue, bones, organs, and vessels away from the bullet’s unpredictable path may also be injured. Appearance of the entrance wound does not always reflect the amount of destruction beneath. An extremity injury may be associated with a truncal injury because of a projectile path through the chest into the arm or through the arm into the chest or because of multiple bullet wounds. (See Chapter 20 for further discussion of gunshot wounds.) Careful assessment, including neurovascular assessment of all limbs, is critical so that other wounds are not overlooked; immunization status needs to be verified. With gunshot wounds, evidence surrounding the wound site or powder burns on the hand should be carefully protected until the police can perform requisite testing. (See Chapter 16 for a detailed discussion of evidence collection and preservation.)
 |
| FIGURE 25-6 Gunshot wound fracture of radius and ulna with extensive soft-tissue damage. (From Frank ED, Long BW, Smith BJ: Merrill’s atlas of radiographic positioning and procedures, ed 11, St. Louis, 2007, Mosby.) |
Tendon and Muscle Rupture
Tendon and muscle ruptures are generally related to sports or recreation; however, metabolic disease and age may be causative factors. Runners may experience a quadriceps tear, whereas a biceps tear can occur with minimal effort in middle-age or older individuals. Surgery may be required to restore function for complete tears. For an incomplete injury, treatment usually consists of rest and intermittent application of ice for 24 to 48 hours followed by heat.
An Achilles tendon rupture can occur in start-and-stop sports in which a person steps off abruptly on the forefoot with the knee forced in extension. The patient may also report hearing a loud crack or snap or sensation of something striking their posterior ankle. This causes sharp pain extending from the heel into the back of the leg, sudden inability to use the foot, and obvious deformity. A clinical tool to assist in the diagnosis is the Thompson test: the patient lies supine on the examination table with the feet hanging off the edge; the examiner squeezes each calf bilaterally and observes for plantar flexion. If a complete rupture has occurred, there is minimal or no foot movement (a positive Thompson’s sign). A splint in plantar flexion should be applied and the patient prepared for surgery. 3
Crush Injuries
Crush injuries frequently occur in industrial settings (e.g., arm caught in the wringer of an industrial washing machine, press, or conveyor; limbs or trunk caught between equipment). Injury may involve only the distal end of a digit or large areas of the body. Depending on the extent of damage, orthopedic, surgical, neurosurgical, or vascular-surgical intervention may be required.
Complications from crush injuries depend on the mechanism of injury and extent of tissue damage. With significant tissue necrosis, systemic crush syndrome can develop, characterized by myoglobinuria, extracellular fluid loss, acidosis, increased potassium, renal failure, shock, and cardiac disruption. 15
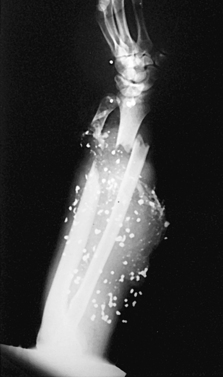
Compartment Syndrome
Compartment syndrome occurs when swelling or compression-restriction causes pressure in the muscle compartment to rise to the point that microvascular circulation is interrupted. The resulting tissue ischemia threatens limb survival. Compartment syndrome is associated with severe soft-tissue injuries and fractures, casts, or a pneumatic antishock garment (PASG). Prolonged pressure directly on a limb, frostbite, or snakebite can also lead to compartment syndrome. It usually occurs in compartments of the lower leg and forearm (Figure 25-7). Symptoms develop 6 to 8 hours after injury but may be delayed 48 to 96 hours. Symptoms include deep, throbbing pain out of proportion to the original injury that is not relieved by narcotics, pain with passive flexion, decreased mobility of digits, paresthesia, coolness, pallor, and tenseness of overlying skin. Pulses may be absent, decreased, or palpable with compartment syndrome.
 |
| FIGURE 25-7 Cross-section anatomy of calf, forearm, and hand showing fascial compartments (From Matsen FA III: Compartmental syndromes, New York, 1980, Grune & Stratton.) |
Irreversible tissue damage occurs within 4 to 6 hours of ischemia; therefore prompt physician notification is essential. The limb is positioned level with the heart, and neurovascular function is assessed hourly, or more often if indicated, to identify changes. Diagnosis is made by measuring compartment pressure with a syringe or catheter device (Figure 25-8). Pressures greater than 30 to 60 mm Hg usually require fasciotomy. 11 A high index of suspicion is necessary when caring for injured comatose patients who cannot verbalize increasing pain or paresthesia. 7
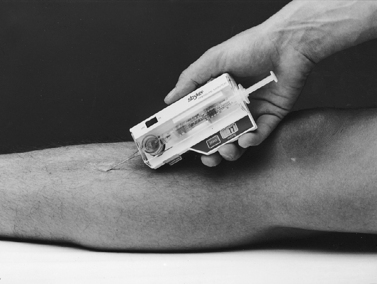 |
| FIGURE 25-8 The Stryker 295 intracompartmental pressure monitor. (Courtesy Stryker Surgical, Kalamazoo, Mich.) |
Peripheral Nerve and Artery Injury
The most common causes of peripheral nerve and artery injuries are lacerations, penetrating wounds, fractures, and dislocations. Joints are well innervated and vascularized, so they are especially prone to nerve or artery damage. Familiarity with major nerves and arteries is necessary for assessment of tissue injuries.
Nerve injury may also occur from compression caused by prolonged PASG use or skeletal traction. Resolution of symptoms depends on the type of injury and length of time before compression is corrected. Partial nerve injury may be caused by a contusion that causes temporary paralysis and sensory deficit. Complete and total disruption of the nerve causes loss of all functions and usually requires surgical repair. Nerve evaluation and repair of an isolated injury may be done on an outpatient basis. Table 25-1 describes the assessment of common peripheral nerve injuries.
| Nerve | Frequently Associated Injuries | Assessment Findings |
|---|---|---|
| Radial | Fracture of humerus, especially middle and distal thirds | Inability to extend thumb in “hitchhiker’s sign” |
| Ulnar | Fracture of medial humeral epicondyle | Loss of pain perception in tip of little finger |
| Median | Elbow dislocation or wrist or forearm injury | Loss of pain perception in tip of index finger |
| Peroneal | Tibia or fibula fracture; dislocation of knee | Inability to extend great toe or foot; may also be associated with sciatic nerve injury |
| Sciatic and tibial | Infrequent with fractures or dislocations | Loss of pain perception in sole of foot |
Axillary, brachial, radial, and ulnar arteries are the major arteries in the arms. Femoral, popliteal, anterior tibial, posterior tibial, and peroneal arteries are major arteries in the leg. High-impact and rapid-deceleration mechanisms are most likely to cause arterial injury. Assessment should evaluate pulse quality, skin color and temperature, capillary refill, bleeding, hematoma formation, and presence of bruits.
Arterial injuries may be difficult to discover; 10% to 15% of significant arterial disruptions can have detectable distal pulses. 12 A Doppler ultrasound should be used for pulses that are difficult to palpate. Evaluation may require angiography; however, injury in association with an open fracture may be evaluated during surgery. Arterial injuries may not require repair if existing collateral circulation prevents ischemia. Complications of undiagnosed arterial disruptions include thrombosis, arteriovenous fistula, aneurysm, false aneurysm, and tissue ischemia with resultant limb dysfunction. 8
Strains
A strain is a weakening or overstretching of a muscle at the point of attachment to the tendon. Strains may occur as a result of almost any type of movement, from twisting the ankle to wrenching forces caused by an MVC or violent muscle contraction. Strains are most often associated with athletic injuries.
A patient with a first-degree or mild strain complains of local pain, point tenderness, and slight muscle spasms. Therapeutic interventions include a compression bandage, intermittent elevation of the limb above heart level for 12 hours, application of a cold pack for the same period, and light weight bearing on the injured part.
With a second-degree strain the patient has local pain, point tenderness, swelling, discoloration, and inability to use the limb for prolonged periods. Therapeutic interventions include a compression bandage, elevation, and intermittent cold pack application for 24 hours; analgesia; and light weight bearing.
Severe strains (third-degree) cause complete disruption of the muscle or tendon. This disruption can cause a small avulsion fracture that can be seen on x-ray films. The patient complains of local pain, point tenderness, swelling, and discoloration. The patient often describes a “snapping noise” at the time of injury. Therapeutic interventions include a compression bandage or splints, elevation, and cold pack application for 24 to 72 hours; analgesia; and no weight bearing for 48 hours. Surgery may be required if a complete rupture occurs at the tendon-bone attachment site.
Sprains
Mechanism of injury for sprains may be the same as for strains, but a sprain is usually the result of more traumatic force. A sprain occurs when a joint exceeds its normal limit and damages ligaments. The patient may have a history of a popping or snapping sound. Sprains often occur in ankles, knees, and shoulders. In children, epiphyseal disruption is more common than ligamentous injury. A mild sprain (first-degree) produces slight pain and slight swelling. Therapeutic interventions include a compression bandage, elevation, intermittent cold pack application for 12 hours, and light weight bearing. A moderate sprain (second-degree) causes pain, point tenderness, swelling, and inability to use the limb for more than a brief period. Therapeutic interventions include compression bandage, elevation, intermittent cold pack application for 24 hours, and light weight bearing with crutches. A stirrup ankle brace is commonly applied to the ankle to prevent inversion and eversion of the ankle, but allow flexion and extension.
A severe sprain (third-degree) involves torn ligaments, which cause pain, point tenderness, swelling, discoloration, and inability to use the limb. Therapeutic interventions include a splint or cast, elevation, intermittent cold pack application for 48 hours, and light to no weight bearing with crutches (lower extremity injury).
Knee Injuries
Knee injuries are a common form of soft-tissue injury in which rotation or excess flexion strains or tears the medial meniscus, collateral ligament, or cruciate ligament. Symptoms include swelling, ecchymosis, effusion, pain, and tenderness. Therapeutic interventions include a compression bandage, knee immobilizer, or cylinder cast; elevation of the injured limb; intermittent cold pack application to the injured area for the first 24 hours; and non–weight bearing with crutch walking. If the injury is a ligament tear, surgical repair within 24 to 48 hours of injury is recommended.
FRACTURES
A fracture is a disruption or break in the bone. Patients may arrive in the ED with angulation, deformity, pain, regional and point tenderness, swelling, immobility, and/or crepitus. Other findings might include bony fragment protrusion, impaired neurovascular status, and occasionally shock.
Fractures are divided into two general categories: closed and open. With closed or simple fractures, the bone is broken but the skin is intact. Open or compound fractures are characterized by bone protrusion or puncture wounds in which the bone punctures the skin or a foreign object penetrates the skin and bone, causing a fracture. Table 25-2 describes etiology for various types of fractures with illustrations for each type in Figure 25-9.
| Type | Etiology |
|---|---|
| Transverse fracture | Sharp, direct blow |
| Oblique fracture | Twisting force |
| Spiral fracture | Twisting force while foot is firmly planted |
| Comminuted fracture | Severe direct trauma causes more than two fragments |
| Impacted fracture | Severe trauma, causes bone ends to jam together |
| Compression fracture | Severe force to top of head, sacrum, or os calcis (axial loading) forces vertebrae together |
| Greenstick fracture | Compression force; usually occurs in school-age children |
| Avulsion fracture | Forceful contraction of a muscle mass; causes a bone fragment to break away at the insertion point |
| Depressed fracture | Blunt trauma to a flat bone; usually associated with significant soft-tissue damage |
 |
| FIGURE 25-9 Types of fractures. A, Transverse fracture. B, Oblique fracture. C, Spiral fracture. D, Comminuted fracture. E, Impacted fracture. F, Compression fracture. G, Greenstick fracture. H, Avulsion fracture. I, Depressed fracture. |
Open fractures are considered contaminated and require prophylactic antibiotic therapy. These fractures are graded by severity, then further categorized by wound size, amount of soft-tissue damage, injury to the periosteum, and vascular damage. Most open fractures require surgical debridement. A greater potential for shock exists with open fractures because of the potential for significant blood loss; closed injuries are more likely to tamponade and limit blood loss. 7 General nursing care includes fracture immobilization and establishing IV access for fluid replacement, antibiotics, analgesia, and anesthesia. Wound care includes irrigation with normal saline, covering with a dry sterile dressing, and verification of tetanus immunization status.
After evaluation of ABCs, specific limb injury assessment should be completed, followed by immobilization, elevation, and ice packs. Repeated neurovascular assessments are essential to identifying changes secondary to swelling. History should be obtained to determine mechanism of injury. The emergency nurse should also be alert for signs of abuse when the injury does not match the history. Understanding patterns of injury also facilitates assessment and identification of less obvious injuries.
When a limb suffers significant trauma, a fracture should be suspected until proven otherwise by radiologic studies. Radiography should include both anterior and lateral views because fractures may appear from only one angle. 4 Joints above and below the injury should be included in all radiographic evaluations.
Open fractures and certain closed fractures require surgical intervention. Ideally, patients with open fractures should have surgery within 8 hours of the injury. 5 The patient should be kept NPO and prepared for surgery. IV lines are inserted, and consent should be obtained before narcotics are administered. Prophylactic broad-spectrum antibiotics are given as soon as possible for open fractures and vascular injuries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


