Care of Patients with Peripheral Nerve and Degenerative Neurologic Disorders
Objectives
1. Compare and contrast the pathophysiology of Parkinson’s disease and myasthenia gravis.
2. Discuss treatments for Parkinson’s disease.
3. Describe the nursing care needed for the patient with Parkinson’s disease.
4. Explain why multiple sclerosis might be difficult to diagnose.
5. Devise a home care plan for the patient with multiple sclerosis.
6. Compile a nursing care plan for the patient with Guillain-Barré syndrome.
7. Identify the differences between Huntington’s disease and amyotrophic lateral sclerosis.
8. Illustrate the signs and symptoms of myasthenia gravis.
9. Compare and contrast the complications of Parkinson’s disease with those of myasthenia gravis.
1. Teach a newly diagnosed patient about the medications for Parkinson’s disease.
2. Teach a patient about the diagnostic tests that might be ordered if multiple sclerosis is suspected.
Key Terms
bradykinesia (brā-dē-kĭ-NĒ-zē-ă, p. 552)
chorea (kă-RĒ-ă, p. 562)
demyelination (dĕ-MĪ-ĕ-lĭ-nā-shŭn, p. 557)
diplopia (dĭ-PLŌ-pē-ă, p. 562)
hyperesthesia (hī-pĕr-ĕs-THĒ-zē-ă, p. 560)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
 Parkinson’s Disease
Parkinson’s Disease
Parkinson’s disease (PD) is named after James Parkinson, who first described the syndrome in 1871. PD is considered a major health problem because of its crippling effects. It is a progressive disorder, beginning rapidly at first and then advancing more slowly. It affects more men than women and occurs most frequently after age 60. Approximately 1 million people in the United States are affected with PD, and about 50,000 people in the United States are diagnosed with PD each year.
Etiology
The specific cause of PD is unknown, but it involves degeneration of the dopamine-producing neurons in the substantia nigra of the midbrain, and the presence of Lewy bodies (cytoplasmic inclusions). Genetic susceptibility and environmental toxins appear to play a role. The most common type of PD is idiopathic, that is, the primary or specific cause is not known. Secondary PD can be drug induced, especially by reserpine-type antihypertensives such as methyldopa, phenothiazines, some tranquilizers such as the butyrophenones (e.g., haloperidol [Haldol]), some antiemetics, methamphetamine, and a few other drugs. These drugs block the uptake of dopamine at the receptors in the brain cells, and so may induce PD symptoms. Pesticide and herbicide exposure is largely implicated as a cause of PD.
Pathophysiology
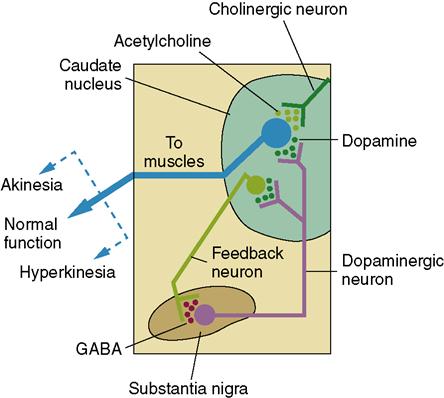
PD affects the extrapyramidal system, in particular the motor structures in the basal ganglia. This is the part of the brain that controls balance and coordination. The basal ganglia are gray matter that is scattered throughout the white matter of the cerebrum beneath the cerebral cortex. Stimulation of the basal ganglia causes muscle tone in the body to be inhibited and allows refined voluntary movements. Two neurotransmitters accomplish this action: dopamine and acetylcholine (ACh) (see Table 22-4 for the action of the common neurotransmitters). ACh-producing neurons transmit excitatory messages throughout the basal ganglia. Dopamine inhibits the function of these neurons so that there can be control of voluntary movement (Figure 25-1). There is usually a balance between these neurotransmitters. The degenerative changes in the basal ganglia lead to a decrease in dopamine. The ACh-secreting neurons remain active, creating an imbalance between excitatory and inhibitory neuronal activity. The excessive excitation of neurons prevents a person from controlling or initiating voluntary movements.
Signs and Symptoms
The onset of PD is gradual and may involve only one side of the body initially. A triad of symptoms is characteristic of PD: tremor, bradykinesia, and rigidity. The first, tremor, occurs when the body is at rest, decreases when there is voluntary movement, and is absent when the patient is asleep. The tremor is most often a “pill-rolling” motion of the thumb against the fingers. This is when there is a circular rubbing of a finger or two as if rolling a piece of string or fuzz into a “pill.” If the patient suffers stress and emotional tension, the tremor becomes more pronounced.
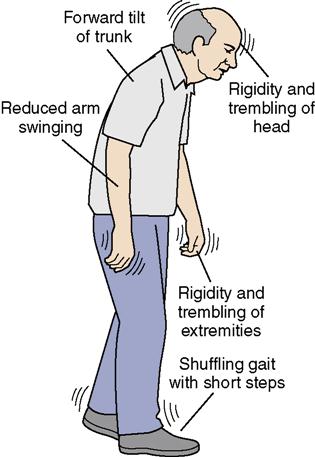
Bradykinesia (condition exhibiting slow movement and speech) produces poor body balance, a characteristic gait, and difficulty initiating movement. The gait is shuffling, with short steps that become quicker (Figure 25-2). There is decreased swinging of the arms when walking. A foot may drag or may be stiff, producing a limp. Earlier in the disease process, the patient may lean slightly to one side, propel forward uncontrollably, or fall backward. In advanced stages there is a stiff, bent-forward posture when walking.
The third symptom is rigidity affecting the skeletal muscles and contributing to postural changes and difficulty in movement. Postural changes affect coordination and balance. The face becomes blank or masklike in appearance with little or no expression. Speech becomes low in tone, monotonous sounding, and slow; enunciation becomes difficult due to the decreased dopamine and the excitatory response from the increased acetylcholine. Drooling may occur. The patient may experience decreased tearing, constipation, incontinence, excessive perspiration, heat intolerance, and decreased sexual ability. PD does not usually affect intellect; however, a percentage of patients do develop a dementia similar to that of Alzheimer’s disease. Mood disturbance does occur, and depression is a problem. Stress tends to make symptoms worse.
Diagnosis
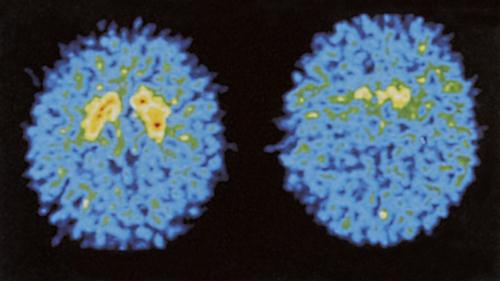
The characteristic symptoms of the disease are used to diagnose the disorder. Laboratory tests usually reveal findings within normal ranges. However, magnetic resonance imaging (MRI) scans of the brain may be performed to rule out other neurologic disorders. Single-photon emission computed tomography (SPECT) can display the reduced uptake of dopamine (Figure 25-3).
Treatment
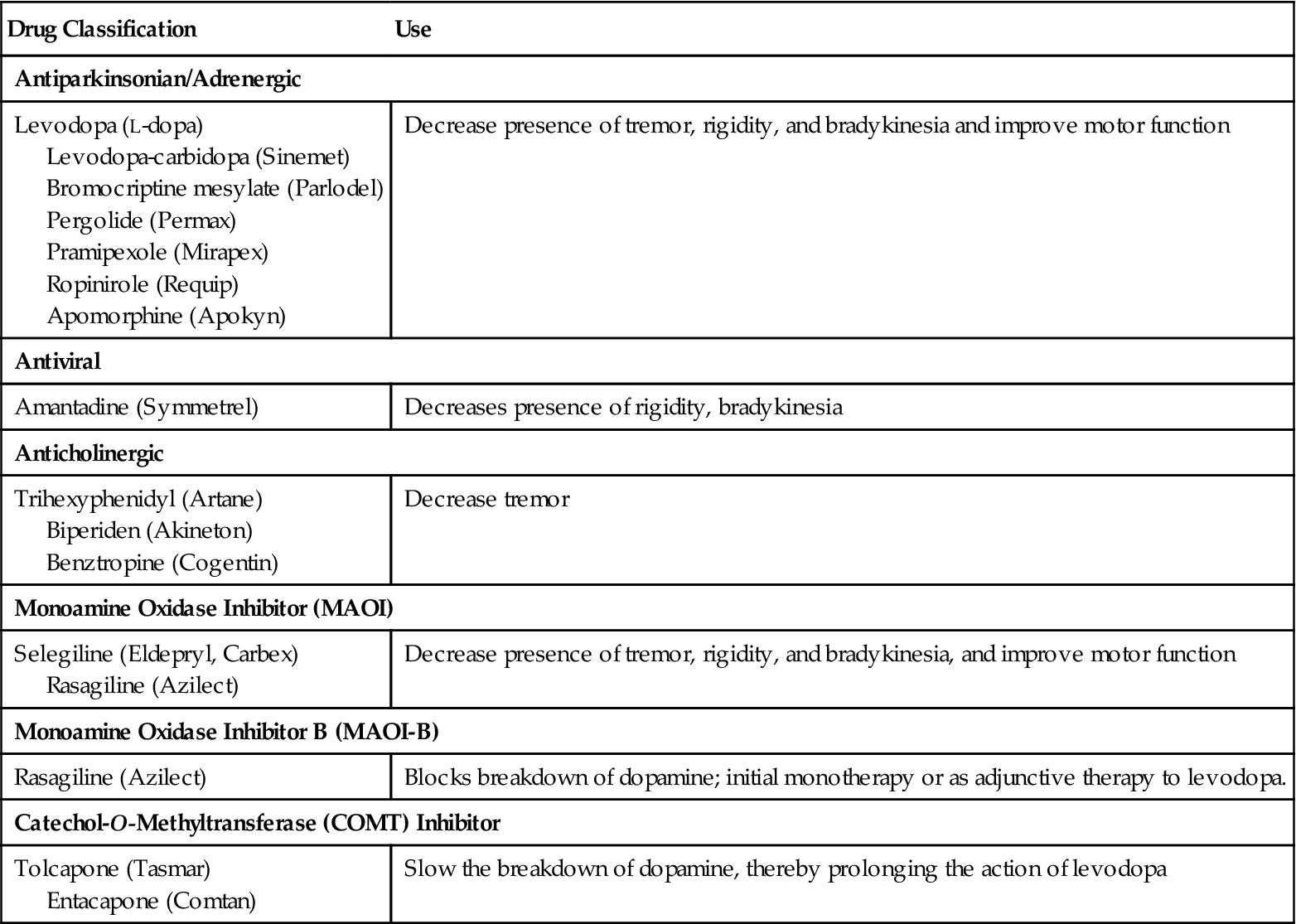
Treatment of PD usually includes drug therapy, physical therapy, and considerable emotional support. Drug therapy aims to provide dopamine to the basal ganglia and thus reduce symptoms. Anticholinergics, dopamine agonists, and monoamine oxidase inhibitor (MAOI) drugs are used to control symptoms. MAOIs block the metabolism of dopamine, leaving more dopamine in circulation.
In the early stages of the disease when disability is not evident, selegiline (Eldepryl), a drug that increases dopamine’s action, may be given. When disability is present, L-dioxyphenylalanine (L-dopa, or levodopa) or a combination of levodopa and carbidopa (Sinemet) is given. Sinemet is given in increasing doses until control of the symptoms is achieved; however, side effects can be troublesome (Box 25-1) Various drugs are used either alone or in combination with L-dopa (Table 25-1).
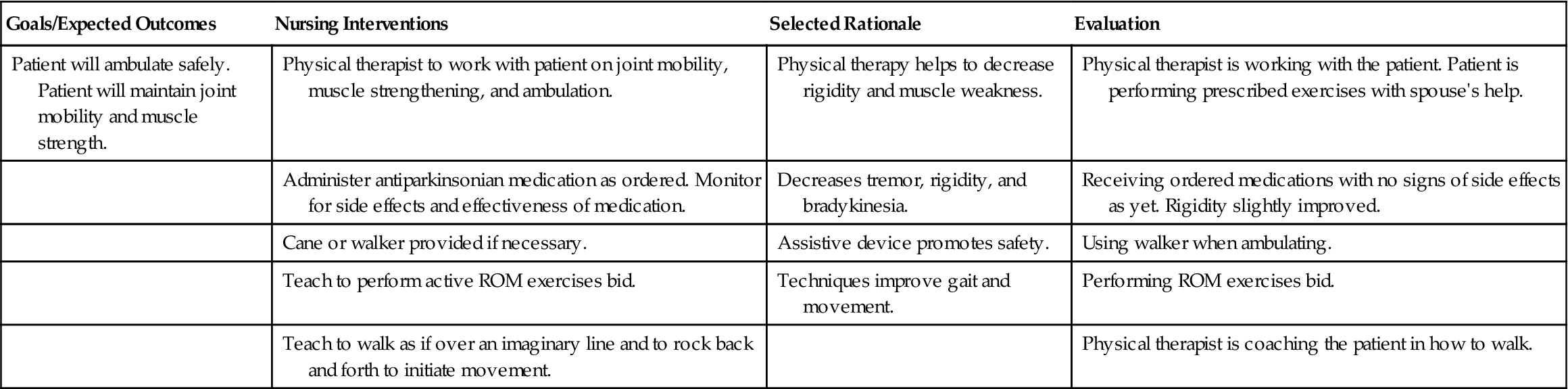
 Table 25-1
Table 25-1
Drugs Commonly Used for Patients with Parkinson’s Disease
| Drug Classification | Use |
| Antiparkinsonian/Adrenergic | |
| Levodopa (L-dopa) Levodopa-carbidopa (Sinemet) Bromocriptine mesylate (Parlodel) Pergolide (Permax) Pramipexole (Mirapex) Ropinirole (Requip) Apomorphine (Apokyn) | Decrease presence of tremor, rigidity, and bradykinesia and improve motor function |
| Antiviral | |
| Amantadine (Symmetrel) | Decreases presence of rigidity, bradykinesia |
| Anticholinergic | |
| Trihexyphenidyl (Artane) Biperiden (Akineton) Benztropine (Cogentin) | Decrease tremor |
| Monoamine Oxidase Inhibitor (MAOI) | |
| Selegiline (Eldepryl, Carbex) Rasagiline (Azilect) | Decrease presence of tremor, rigidity, and bradykinesia, and improve motor function |
| Monoamine Oxidase Inhibitor B (MAOI-B) | |
| Rasagiline (Azilect) | Blocks breakdown of dopamine; initial monotherapy or as adjunctive therapy to levodopa. |
| Catechol-O-Methyltransferase (COMT) Inhibitor | |
| Tolcapone (Tasmar) Entacapone (Comtan) | Slow the breakdown of dopamine, thereby prolonging the action of levodopa |
Surgical Treatment
Stereotactic neurosurgery may be done if the drug therapy fails to assist the patient with PD symptoms. In one such procedure the area in the thalamus that is causing the involuntary movements is destroyed. Microsurgical procedures such as pallidotomy improve rigidity and bradykinesia (Clarke, 2007; WebMD, 2010b).
Other procedures with some success in relieving symptoms include transplanting tissue from the adrenal medulla into the brain, or implanting fetal tissue or stem cells. Stem cells are transplanted into the caudate nucleus of the brain. This is still experimental, but the procedure has shown substantial clinical improvements in motor function (Susman, 2010).
Deep brain stimulation (DBS) uses electrode implants to provide electrical shocks that control tremors by blocking them. The device that delivers the shocks can be adjusted as the patient’s symptoms change or worsen (National Institute of Neurological Diseases and Stroke, 2007). There has been considerable success with DBS, but it is expensive at $10,000 for the implant unit and another $8000 every few years for battery replacement.
Depression is frequent in Parkinson’s patients, but most respond well to a selective serotonin reuptake inhibitor (SSRI) antidepressant.
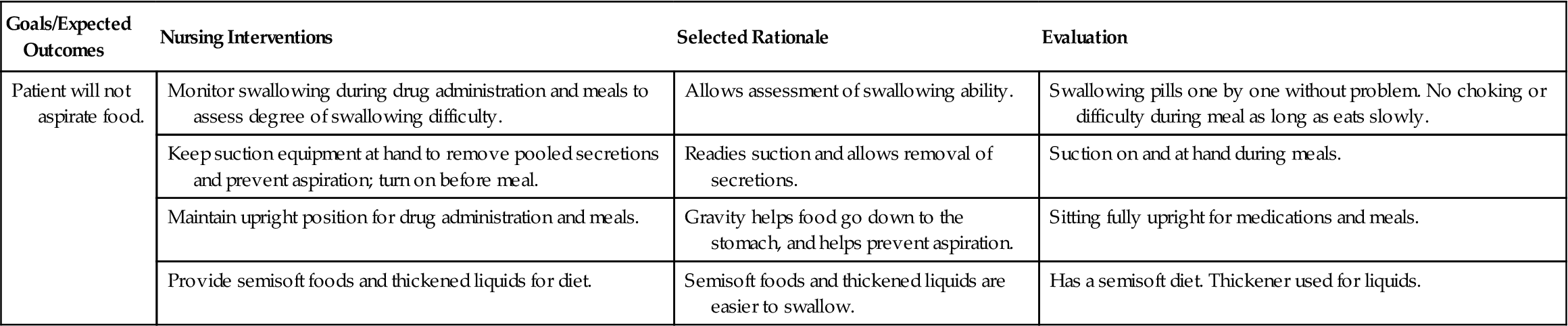
Complications
Dysphagia may develop and mobility becomes severely limited as the disease progresses. Problems of immobility occur (see Chapter 9). Constipation, urinary incontinence, and insomnia are also common.
Nursing Management
Assessment (Data Collection) and Nursing Diagnosis
A thorough history is gathered and a physical examination is performed for the patient who has or is thought to have PD. Nursing Care Plan 25-1 contains the common nursing diagnoses, expected outcomes, and specific interventions for the patient with PD.
Planning, Implementation, and Evaluation
Nursing care focuses on preventing complications of PD, drug therapy, enhancing voluntary movement, and safety. Constipation is a problem and requires the addition of fiber to the diet and an increase in fluids to at least 3000 mL per 24 hours.  Grasping coins or other objects may help decrease tremors because it is an intentional action. Walking may be improved by having the patient think about imaginary lines across the pathway on which to walk. Imagining stepping over something helps prevent “freezing” when walking. Teach the patient to consciously assume correct posture. Not using a pillow when resting helps prevent flexion of the spine. Learning to sleep prone also is beneficial for posture correction. The physical therapist will institute an exercise program to help the patient maintain muscle function and promote joint mobility.
Grasping coins or other objects may help decrease tremors because it is an intentional action. Walking may be improved by having the patient think about imaginary lines across the pathway on which to walk. Imagining stepping over something helps prevent “freezing” when walking. Teach the patient to consciously assume correct posture. Not using a pillow when resting helps prevent flexion of the spine. Learning to sleep prone also is beneficial for posture correction. The physical therapist will institute an exercise program to help the patient maintain muscle function and promote joint mobility.
Remember that the PD patient needs extra time to finish tasks. A warming tray can be used to keep food hot during meals so that the patient can take rest periods while eating. Considerable patience and understanding are necessary to help the patient deal with the frustration of deteriorating body control and inability to do things that he formerly could easily do. Degeneration of cognitive skills occurs in the late stages of PD.
Falls are common, and safety is a major factor. Using a cane or walker will increase stability and decrease the incidence of falls. Leg braces or foot braces may help to maintain balance. Loose carpets should be removed from the home. Grab bars should be installed in the shower and tub; a raised toilet seat should also be installed. Patients with tremor must be cautioned against carrying hot liquids, as spills may cause burns. Chapter 22 discusses measures to help with the problems typical of many neurologic disorders. Patient and family teaching is an important part of nursing care for patients with PD.