CHAPTER 23. Thoracic Trauma
Nancy J. Denke
Chest trauma is a significant source of morbidity and mortality, accounting for 20% to 25% of trauma-related deaths in adults. Two thirds of these deaths occur before the patient reaches the hospital because of major disruption of the airway, impaired breathing, or lethal alterations in circulation (injury to the heart and/or great vessels). The incidence has increased markedly over the last 100 years because of high-speed vehicular travel and interpersonal violence. In children, thoracic trauma commonly occurs as part of multisystem injury, with 90% of childhood thoracic traumas being blunt injuries. 13 Chest trauma can result from either penetrating or blunt trauma, causing a spectrum of injuries ranging from a simple rib fracture to severe vital organ injuries. Mechanism of injury, force, trajectory, type of weapon, angle of impact, proximity to the patient, secondary factors such as fire, and overall physical attributes of the patient determine degree and type of injury. The physical nature of the chest wall allows for considerable elastic recoil; therefore the severity of thoracic trauma may need to be assessed, focusing on the potential for underlying damage based on mechanism of injury, rather than on the initial appearance of the patient.
Blunt trauma to the chest is more common than penetrating injury, accounting for more than 90% of thoracic injuries. 9 Blunt trauma may be caused by motor vehicle incidents, falls, exploding tires, or any mechanism where the force of impact (particularly sudden deceleration, compression, or a direct blow) causes internal structural damage to the chest wall, parenchyma, pleura, diaphragm, heart, trachea, and/or great vessels. Penetrating injuries are a result of direct application of a mechanical (e.g., projectile) force to tissue or organs and the energy that is transferred from the object to the body tissues. The velocity of the penetrating projectile is the single most important factor that determines the severity of the wound. 9 Blunt and penetrating injuries may be sustained in all types of trauma; therefore anticipation is key to the prompt management of patients with chest trauma.
Thoracic injury and treatment have been described for centuries; however, it was not until the end of World War II that a chest tube connected to underwater seal drainage became standard treatment for many thoracic injuries. Endotracheal intubation, anesthesia, and chest x-ray examinations developed in the nineteenth and early twentieth centuries, and advances in the past 50 years, such as improved ventilatory assistance, antibiotics, blood gas analysis, and specialized nursing care, have increased survival in patients with thoracic injuries. Despite these advances, mortality rates for thoracic trauma remain second only to brain and spinal cord injuries. 19
Thoracic trauma requires systematic assessment for potentially lethal injuries followed by rapid intervention to prevent unnecessary complications and death. Eighty-five percent of patients with thoracic trauma can be managed by simple lifesaving treatments that do not require surgical interventions. This chapter discusses assessment and treatment of various thoracic injuries. Understanding the anatomy and physiology is essential.
ANATOMY AND PHYSIOLOGY
The thoracic cavity skeleton includes the sternum, ribs, costal cartilages, and thoracic vertebrae. The thorax is fairly mobile and expands easily to accommodate respiratory efforts. The ribs are elastic arches of bone that attach posteriorly to thoracic vertebrae and anteriorly to the sternum. Seven upper ribs are joined directly to costal cartilages, whereas ribs 8, 9, and 10 interface indirectly with the sternum through fusion of costal cartilage. Ribs 11 and 12 do not interface with the sternum. Beneath each rib lies a neurovascular bundle, containing an intercostal nerve, artery, and vein. The sternum has three parts: the manubrium, the body (corpus), and the xiphoid process (tip). The diaphragm forms the inferior border of the thorax, whereas the superior border is continuous with structures of the neck.
Internal thoracic structures are composed of organs and structures of the pulmonary, cardiovascular, and gastrointestinal systems (Figure 23-1). Pulmonary structures are located in the pleural space, whereas cardiovascular and gastrointestinal structures are located in the mediastinum, a cavity between the two pleural spaces.
 |
| FIGURE 23-1 Chest and anatomic landmarks. (From Seidel HM, Ball JW, Dains JE et al: Mosby’s guide to physical examination, ed 6, St. Louis, 2006, Mosby.) |
Pulmonary System
Lungs are cone-shaped organs above the diaphragm that extend approximately 11⁄2 inches above the clavicles. Each lung is located in a cavity lined with a serous membrane called the pleura. The visceral pleura covers the lungs, whereas the parietal pleura covers the rib cage, diaphragm, and pericardium. A potential space between these layers is the pleural cavity. Pleural cells secrete pleural fluid that separates the lungs but allows membranes to remain in contact and move without creating friction.
Normal breathing occurs through the processes of ventilation, which moves air in and out of the lungs, and respiration, which exchanges gases across alveolar-capillary membranes. During inspiration, phrenic nerve stimulation causes the diaphragm to contract and pull downward. As the diaphragm pulls downward, external intercostals pull the chest wall out, which enlarges the thoracic cavity. As lung capacity increases, intrathoracic pressure becomes negative (i.e., lower than atmospheric pressure). This negative intrathoracic pressure draws air into the lungs. During expiration this process is reversed as the diaphragm relaxes and moves up. Intercostal muscles compress the chest so that the lungs recoil passively. Intrathoracic pressure becomes more positive as lung capacity diminishes. Increasing positive intrathoracic pressure forces air out of the lungs. 9
Cardiovascular System
The heart is located in the mediastinum positioned with the right ventricle anteriorly beneath the sternum. The pericardium, a three-layered sac that surrounds and protects the heart, is a fibrous envelope separated from the heart by the pericardial space, a potential space between the parietal pericardium and the visceral pericardium, or epicardium. The pericardium contains pericardial fluid (5 to 30 mL) that minimizes friction during cardiac contraction. The outer parietal pericardium is the fibrous pericardium, which attaches to the sternum, great vessels, and diaphragm to hold the heart in place. The heart itself is composed of three layers: the epicardium (the outermost layer of the heart), the myocardium (the middle, voluminous muscular layer), and the endocardium (the innermost layer of tissue that lines the chambers of the heart).
Four muscular chambers, two atria and two ventricles, contract rhythmically as they fill and empty with blood. The right atrium and ventricle receive deoxygenated blood from the body and pump the blood to the lungs for oxygenation. Oxygenated blood then enters the left side of the heart, which sends blood to the systemic circulation. The left heart is a high-pressure system; the right heart a low-pressure system. Valves separate chambers to prevent regurgitation of blood back into the atria and ventricles. Cardiac function and output depend on contractility, heart rate, preload (volume achieved during diastolic filling of the ventricles), and afterload (force or resistance against which the heart must pump to eject blood).
The thoracic aorta carries oxygenated blood to various tissues. Three anatomic parts of the aorta are recognized: ascending aorta, aortic arch, and descending aorta. The aortic arch is attached to the pulmonary artery by the ligamentum arteriosum. Near the ligamentum, a portion of the aorta branches off to form the left subclavian artery. At this point of the aorta, just distal to the ligamentum, the aorta is relatively immobile and is at increased risk for disruption. More than 85% of aortic injuries caused by acceleration or deceleration forces occur at this site.
Also in the mediastinum are the trachea, located posterior to the heart; the esophagus, posterior to the trachea; the phrenic nerve; and the diaphragm. Other thoracic cavity structures include the thymus gland in the anterior mediastinum behind the sternum and the subclavian and common carotid arteries.
PATIENT ASSESSMENT
The patient with obvious or suspected chest trauma must be promptly assessed because injury to thoracic structures may produce life-threatening alterations in ventilation and perfusion within minutes. Rapid assessment and intervention to support airway, breathing, and circulation (ABCs) are crucial. Protection of the cervical spine occurs simultaneously with assessment of airway patency. Assessment of rate, depth, and effort of breathing performed in conjunction with auscultation of breath sounds and inspection for symmetry and chest wall integrity is performed to identify overt and subtle injuries to the thorax. Supplemental oxygen is administered with a 100% nonrebreather mask or bag-mask device to maintain adequate oxygenation and ventilation. Life-saving interventions required during the initial patient assessment may include application of a three-sided occlusive dressing for an open pneumothorax or needle thoracentesis (decompression) for a tension pneumothorax. Assessment of circulation is performed with palpation of the central and peripheral pulses for quality, rate, skin color/temperature, and capillary refill. Obvious external bleeding is controlled with direct pressure. Internal bleeding is initially managed with replacement of intravascular volume; two large-bore intravenous lines should be established and warmed crystalloids (0.9% normal saline or lactated Ringer’s) infused at a rapid rate. Boxes 23-1 and 23-2 highlight initial and secondary assessment of the patient with thoracic trauma. Therapeutic interventions are listed in Box 23-3.
Box 23-1
Get Clinical Tree app for offline access

I nitial A ssessment of T horacic T rauma
AIRWAY WITH CERVICAL SPINE PROTECTION
BREATHING
Spontaneous breathing
Rise and fall of the chest
Rate and pattern of breathing (such as shortness of breath, paradoxical chest wall movement, respiratory stridor)
Use of accessory muscles, diaphragmatic breathing, or both
Skin color (such as cyanosis)
Integrity of the soft tissues and bony structures of the chest wall (such as sucking chest wound, subcutaneous emphysema, upper abdominal injury)
Bilateral breath sounds
Tracheal deviation and jugular venous distention are considered late signs of airway compromise
CIRCULATION
Skin color, temperature, and moisture
Heart sounds
Vital signs
Blood pressure in upper extremities (equal or asymmetric)
Extremity pulses (equal, diminished, or absent)
ADDITIONAL CONSIDERATIONS
Pattern of abrasions or bruising
Wound size and location
Box 23-2




S econdary A ssessment of T horacic T rauma
Assess pain.
Obtain patient history.
Identify mechanism of injury.
Determine time of the injury.
Determine what the patient remembers about the event.
Box 23-3
T herapeutic I nterventions for T horacic T rauma
Maintain patent airway.
Promote adequate ventilation.
Provide high-flow oxygen.
Assist ventilations.
Prepare for intubation.
Cover open chest wound.
Assist with chest tube insertion or needle thoracentesis (decompression).
Monitor bleeding from chest.
Prepare for autotransfusion.
Initiate two large-bore intravenous lines.
Facilitate essential imaging—ultrasonography, radiography, computed tomography.
Monitor cardiac rhythm continuously.
Monitor blood pressure, respiratory rate and effort, pulse oximetry, and level of consciousness every hour or more often if indicated by patient condition.
Document urine output and patient response to therapeutic interventions.
Facilitate surgical intervention.
The focused assessment sonography for trauma (FAST) examination has become an integral component of the initial assessment for patients with both blunt and penetrating trauma to the thorax and/or abdomen. It is a rapid noninvasive diagnostic study that can be performed at the bedside. (Table 23-1 describes strengths and limitations of the FAST examination.) The subxiphoid view obtained in this four-view study allows for the most rapid identification of pericardial injury. The interpretation is straight-forward: a positive subxiphoid examination is defined as “detection of pericardial fluid on the cardiac window.”23 The absence of fluid in the pericardial region represents a negative examination. The sensitivity of the FAST examination for detecting blood in the pericardial space has been reported at 96% to 100%. 10 Bedside ultrasonography is also being used to detect the accumulation of blood and air in the pleural space. Ultrasonography has been reported to have a higher sensitivity and specificity in detecting pneumothorax than chest radiography. 24
| CT, Computed tomography; DPL, diagnostic peritoneal lavage. | |
| Strengths | Limitations |
|---|---|
• Rapid (2-3 minutes) • Portable • Noninvasive • Can be done serially • Sensitive and specific for free fluid that is equal to a DPL or CT • Inexpensive | • Does not identify the source of bleeding or injuries that may not cause a hemoperitoneum • Limited in detecting <250 mL of peritoneal fluid • Poor diagnostic tool for identifying hollow viscus or retroperitoneal injury • Operator dependent • Obesity and subcutaneous air may interfere with the examination |
SPECIFIC THORACIC INJURIES
Thoracic injuries include injuries of the chest wall, pulmonary system, cardiovascular system, and esophagus. Acuity is determined by the effect of the injury on ventilation and circulation.
Chest Wall Injuries
Rib Fractures
The exact incidence of rib fractures is unknown, but experts estimate a regional trauma center can expect 10% of all trauma admissions to have rib fractures. Fractures result from a direct or indirect blunt force or crush injury. Motor vehicle crashes (MVCs) and falls are the most common mechanisms of injury associated with rib fractures in the adult population. In the pediatric population, rib fractures are commonly the result of intentional injury in younger children, with recreational/athletic injuries being more common in the older pediatric population.
Rib fractures may occur in a single rib or multiple ribs and occur most often in the fourth through tenth ribs. These fractures are not considered life-threatening but can be associated with potentially life-threatening injuries to the underlying organs (most commonly the lungs). The patient often experiences pain/tenderness at the fracture site, so respirations are shallow (splinted) to avoid moving the chest wall. Fragments of fractured ribs can also act as penetrating objects, leading to the formation of a hemothorax or a pneumothorax. Subcutaneous emphysema or crepitus may also be present. Chest radiographs assist with diagnosis but are only 70% sensitive for detecting rib fractures. Fractures that separate the sternum from costal cartilage are not evident on a radiograph.
Fractures of the first and second ribs are rare due to the protection granted to them by the clavicle. Significant blunt force is required to fracture these ribs; therefore associated injuries to the underlying structures, the great vessels, and brachial plexus must be considered. Other injuries associated with upper rib fractures include injuries to the clavicles, scapulae, trachea, and lungs. Lower rib fractures (9 through 12) are associated with injuries to the spleen, liver, kidneys, or other abdominal contents, depending on location of the fracture(s).
Treatment for most rib fractures is focused on the prevention of complications. Good pulmonary toilet, coughing, and deep breathing, in conjunction with use of an incentive spirometer and early mobilization, are recommended to prevent complications, including pneumonia or atelectasis. The use of binders or “strapping” is to be avoided in all patients. Patients with multiple rib fractures are usually admitted for observation. Those with severe injuries (eight or more fractured ribs, massive flail injury) may require internal fixation with plates and screws.
Pain management is essential because even one or two rib fractures can cause respiratory splinting, resulting in atelectasis and pneumonia. Oral, transdermal, or intravenous analgesia is available for many patients. Administration of an opioid in conjunction with a nonsteroidal antiinflammatory drug (NSAID) can provide some of the best analgesia; but the use of NSAIDs must be done with caution in older adults and should not be used until other injuries that may be associated with bleeding are ruled out. Monitoring the older adult patient for respiratory depression when giving opioids is also of utmost importance. Intercostal blocks provide complete analgesia allowing normal inspiration and coughing without the risks of respiratory depression. These blocks may be placed in the thoracic or high-lumbar positions, typically provide relief up to 12 hours, and can be repeated as needed. They are minimally invasive and provide a great deal of pain relief locally.
Older adult patients with rib fractures are at greater risk for complications because of diminished vital capacity that occurs with aging. Impaired ventilation worsens in all patients during the first few days after injury secondary to increasing chest wall edema and decreasing compliance. In an older adult patient with rib injury and diminished capacity, serial assessment is essential to prevent complications. Patients with decreased pulmonary function from asthma or chronic obstructive pulmonary disease also require careful ongoing assessment, in conjunction with good pulmonary toileting, because vital capacity in this population is also decreased.
Children have thin chest walls, and their bony thorax is more cartilaginous. Consequently, energy is easily transmitted to underlying thoracic structures without fracturing ribs. When rib fractures do occur in children, concurrent thoracic and abdominal injuries may be severe. 13
Flail Chest
A flail chest is defined as fractures in two or more adjacent ribs in two or more places, or bilateral detachment of the sternum from costal cartilage (Figure 23-2). Mechanically a significant force diffused over a large area (i.e., the thorax) is usually required to create multiple anterior and posterior rib fractures. 4 Flail chest is usually associated with a fall, massive crush injury, or high-speed MVC. Flail chest commonly occurs in older adults secondary to their weakened structural components. A flail chest creates a free-floating, unstable segment that moves in opposition to normal chest wall movement. The flail segment moves in when the patient inspires and out with exhalation. The loss of coordinated chest wall movement results in hypoventilation of both lungs followed by atelectasis and eventually hypoxia. This injury is usually associated with an underlying pulmonary contusion that further compromises ventilation because of loss of pulmonary compliance, increased airway resistance, and decreased gas diffusion.
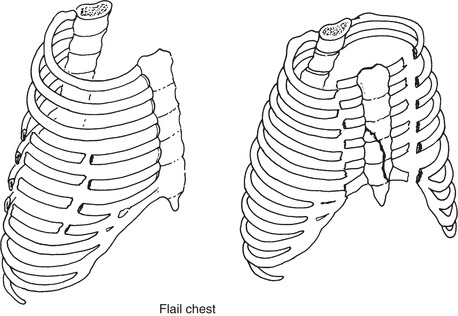 |
| FIGURE 23-2 Fracture of several adjacent ribs in two places with lateral flail or central flail segments. (From Marx J, Hockberger RS, Walls R: Rosen’s emergency medicine: concepts and clinical practice, ed 6, St. Louis, 2006, Mosby.). |
Diagnosis of flail chest is often made by direct observation—the affected area moves paradoxically from the rest of the chest. Muscular splinting of the chest immediately after injury may, however, mask a flail chest until hours later when intercostal muscles become fatigued and paradoxical movement becomes obvious, causing this diagnosis to be missed or delayed. 1. and 4. Paradoxical chest wall movement will not be demonstrated in the mechanically ventilated patient. Palpation of the chest wall may indicate abnormal motion and crepitus. The patient complains of pain and difficulty breathing. Plain chest radiographs may not be helpful because many times fractures are not visible. A computed tomography (CT) scan of the chest can provide significant information as to the number of ribs that are fractured and even early diagnosis of a pulmonary contusion; if there is any suspicion of involvement of the great vessels a CT angiography (CTA) should be performed. Blood gas analysis illustrates the severity of the hypoventilation caused by both the pulmonary contusion and the pain of the rib fractures and can be helpful as a baseline in assessing the need for mechanical ventilation. These values can also assist in the management of pain in these patients. 1
Treatment consists of ensuring adequate oxygenation, judicious fluid administration, and pain management. Fluids are limited because of associated pulmonary contusion and potential development of acute respiratory distress syndrome (ARDS). Intubation and mechanical ventilation are not required for all patients, but patients should be monitored carefully for any change in respiratory status that indicates a need for more aggressive management (i.e., changes in respiratory rate, arterial oxygen tension, and work of breathing). 1 Patients who require mechanical ventilation are usually managed with continuous positive end-expiratory pressure (PEEP); continuous positive airway pressure (CPAP) may successfully be used for some patients. Patient-controlled analgesia (PCA) pumps, oral/transdermal/intravenous pain medications, intercostal blocks, and indwelling epidural catheters form the mainstay of current pain management. Surgical stabilization is rarely used. 4 Although surgical management of patients with severe flail chest is at present controversial, surgical stabilization has been indicated in specific clinical situations, such as when the patient fails to wean from the ventilator once a partial resolution of the pulmonary contusion is achieved, or in patients with deteriorating pulmonary function despite aggressive clearance of bronchial secretions and adequate analgesia.
Sternal Fracture
With the increased use of seat belts, shoulder restraints, and air bags in motor vehicles, there has been a decrease in the number of sternal fractures. Sternal fractures occur when tremendous force is applied to the chest, as with steering wheel impact, sporting injuries in which direct thoracic impact is sustained, or falls. Sternal fractures secondary to cardiac compressions during basic life support measures, or even stress fractures (as in weight lifters) do occur, but rarely. Occurrence is more common in the older adult population due to their inelastic/weakened bony thorax. The most common site of fracture is the junction of the manubrium and body of the sternum (angle of Louis, adjacent to the second intercostal space). 6 In addition to pain, a sternal fracture has significant potential for underlying cardiac and pulmonary injury, including pulmonary contusion, blunt cardiac injury, and pericardial tamponade.
The patient may experience dyspnea and localized pain with movement and may hypoventilate to avoid chest wall movement. Chest wall ecchymosis, sternal deformity, or crepitus may also occur. Treatment includes pain relief (as described above), a baseline electrocardiogram (ECG) to evaluate potential blunt cardiac injury, and serial patient examinations. If the fracture is displaced, operative reduction may be required. If cardiac symptoms are present, an echocardiogram may be obtained to evaluate myocardial performance. No surgical intervention is usually required. Patients are treated symptomatically.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
