Learning outcomes
By the end of this section, you should know how to:
▪ prepare the patient for this nursing practice
▪ collect and prepare the equipment
▪ assist the medical practitioner to perform a lumbar puncture
▪ care for the patient following the procedure.
Background knowledge required
Revision of the anatomy and physiology of the brain and spinal cord, with special reference to the cerebrospinal fluid and meninges
Revision of the anatomy of the lumbar vertebrae
Revision of ‘Aseptic technique’ (seep. 381)
Revision of local policy on lumbar puncture.
Indications and rationale for lumbar puncture
Lumbar puncture is the insertion of a specialised needle into the lumbar subarachnoid space to gain access to the cerebrospinal fluid. This may be required:
▪ to obtain a sample of cerebrospinal fluid for investigative and diagnostic purposes, e.g.:
— bacteriological investigation for patients suspected of having meningitis or encephalitis
— cytological investigation for patients suspected of having a malignant tumour
▪ to identify the presence of blood in the cerebrospinal fluid following trauma or a suspected subarachnoid haemorrhage
▪ to introduce radio-opaque fluid into the subarachnoid space for radiographic investigation
▪ to identify raised intraspinal/intracranial pressure and provide relief, if appropriate, by removing some of the cerebrospinal fluid
▪ to introduce intrathecal medication such as cytotoxic agents or antibiotics (Lyndsay and Bone 2004).
The procedure may be performed on patients who are inpatients or day patients, according to their clinical status. A lumbar puncture should not be performed if raised intracranial pressure is suspected as the raised pressure might cause the brain stem tissue to herniate through the foramen magnum. This is known as ‘coning’ and could be fatal (Boon et al 2004).
Outline of the procedure
A lumbar puncture is performed by a medical practitioner using an aseptic technique. The patient is helped into the correct position. An area of skin above the 3rd, 4th and 5th lumbar vertebrae is prepared and cleansed with alcohol-based antiseptic solution prior to the administration of local anaesthesia. Once the local anaesthetic has taken effect, a special lumbar puncture needle is inserted between the 3rd and 4th, or 4th and 5th, lumbar vertebrae in order to gain access to the subarachnoid space below the spinal cord in the region of the cauda equina (Fig. 23.1). The needle is hollow with a stilette to ease introduction to the subarachnoid space. Once in position, the stilette of the needle is removed. A disposable manometer is attached to the end of the needle via a two-way tap, and the cerebrospinal fluid (CSF) is allowed to flow into the manometer to record the intraspinal pressure. A normal CSF pressure is 60–150 mmH2O. The pressure will fluctuate with respiration and heart beat. Coughing will cause the pressure to rise (Clarke 2002).
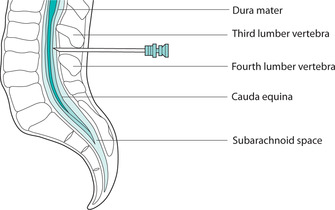 |
| FIGURE 23.1Lumbar puncture: position of the needle in relation to the vertebrae |
When the pressure recording has been completed, the manometer is occluded, and 2–3 ml of cerebrospinal fluid is allowed to flow into each of the three separate sterile specimen containers as required while still maintaining asepsis. The specimen containers should be pre-labelled, numbers 1, 2 and 3 because the first specimen may contain blood as a result of the needle being introduced. The containers should collect the specimens sequentially to avoid misinterpretation of results. The medical practitioner will note the colour, consistency and opacity of the cerebrospinal fluid as well as observing the presence or absence of blood. On completion of this stage, the needle is removed, and the puncture site is covered by a small sterile dressing or plastic sealant spray. Following this procedure, according to local policy and the patient’s clinical status, appropriate neurological observations, wound-site assessment and the monitoring of any localised pain or headache should be performed (Lindsay & Bone 2004).
The position of the patient
The correct position is important in order to ensure the success and safety of this procedure. Patients should lie on their side on a firm bed with one pillow, stretching their lumbar vertebrae by flexing their head and neck and drawing their knees up to the abdomen, holding them with their hands (Fig. 23.2). The nurse can assist by supporting the patient behind the knees and the neck, and helping to maintain the extension of the lumbar vertebrae, thus widening the intervertebral space. This will help to ensure that the insertion and correct placement of the lumbar puncture needle is safely achieved. Once the needle is in position, the medical practitioner may ask patients to straighten their legs slowly without moving the position of their back. This will reduce the intra-abdominal pressure, which can cause an abnormal reading of intraspinal pressure.
 |
| FIGURE 23.2Lumbar puncture: position of the patientFrom Lindsay & Bone 2004, with permission |
This procedure is occasionally performed with a patient sitting straddled on a chair and facing the back of the chair with his or her head resting on folded arms. This position may be chosen by the medical practitioner when performing a lumbar puncture for an obese patient with dyspnoea who may be distressed when lying flat. Whichever position is used, it is important for the patient to remain still (Tate & Tasota 2000).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


