Care of Patients with Coronary Artery Disease and Cardiac Surgery
Objectives
1. Discuss the causes of coronary artery disease.
2. Describe the pathophysiology of coronary artery disease.
4. Discuss the pathophysiology of myocardial infarction.
6. Develop a nursing care plan for a patient experiencing a myocardial infarction.
7. Describe the nursing care of a patient undergoing cardiac surgery.
1. Develop a teaching plan for a patient with coronary artery disease.
2. Identify signs and symptoms that indicate a patient may be experiencing a myocardial infarct.
3. Administer medications to patients experiencing cardiac disorders.
4. Collaborate with other health care providers to care for patients after cardiac surgery.
5. Contribute to discharge planning for a patient after cardiac surgery.
Key Terms
angina pectoris (ăn-JĪ-nă-PĔK-tŏr-ĭs, p. 453)
atherosclerosis (ăth-ĕr-ō-sklĕ-RŌ-sĭs, p. 451)
coronary artery bypass graft (CABG) (p. 464)
coronary insufficiency (KŎR-ō-nĕr-ē ĭn-să-FĬSH-ăn-sē, p. 452)
drug-eluting stent (stĕnt, p. 464)
infarction (ĭn-FĂRK-shŭn, p. 458)
metabolic equivalent (MET) units (p. 463)
myocardial infarction (MI) (mī-ō-KĂR-dē-ăl ĭn-FĂRK-shŭn, p. 451)
necrosis (nē-KRŌ-sĭs, p. 452)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Coronary Artery Disease
Coronary artery disease (CAD) is a progressive disease leading to narrowing or occlusion (blockage) of the coronary arteries. The coronary arteries are responsible for supplying oxygen and nutrition to the myocardium (see Figure 18-2). As the coronary vessel narrows, the patient may experience symptoms of ischemia, such as chest tightness and angina. When a sudden obstruction to blood flow through one or more major coronary arteries occurs and cuts off oxygen and nutrients to the cardiac cells, a myocardial infarction (MI) occurs.
Etiology
A major factor in the development of CAD is atherosclerosis, in which plaque containing cholesterol and lipids is laid down inside the arteries as fatty streaks. Plaque can occur in the cerebral vessels, the aorta, and arteries other than the coronaries. Atherosclerosis is one form of arteriosclerosis. Arteriosclerosis is a general term for disorders that cause thickening and loss of elasticity of the arteries.
Factors such as age (over 40), gender, and race contribute to the disease; however, these susceptibilities cannot be modified. Those who have had one or more immediate family members die of coronary artery disease during middle age are considered to be at high risk for the disorder. Postmenopausal women and women who use oral contraceptives or hormone replacement therapy are at greater risk of coronary artery disease than are women outside these categories.
Pathophysiology
The process of atherosclerosis begins during late childhood, when streaks or islands of fatty material are laid down on the inner walls of the arteries. Low-density lipoprotein (LDL) is the major contributing factor to the formation of this fatty material. Plaques accumulate, particularly where there has been irritation or inflammation of the blood vessel from smoking, hypertension, diabetes, or infection. Later, the plaques become fibrous as a result of inflammation and healing. The plaque area protrudes into the artery, decreasing the vessel’s size (Figure 21-1). When plaque areas rupture, the rough edges cause platelet clumping and clotting (thrombosis). Over time, the plaque begins to calcify, causing rigidity of the vessel wall. The further narrowing of the coronary arteries causes coronary insufficiency (decreased or insufficient blood flow). Obstruction occurs from this process and from thrombosis. Arterial spasm may contribute to deficient blood flow and consequent heart muscle damage.
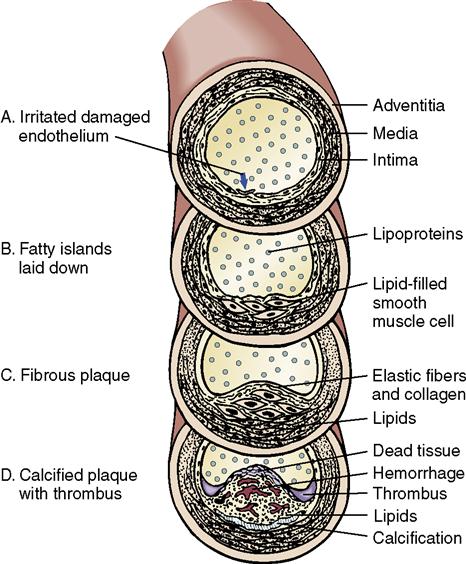
There is a proven link between hyperlipidemia or high levels of LDL and triglycerides and atherosclerosis. High levels of homocysteine and episodes of inflammation causing an elevated level of C-reactive protein (CRP) are also factors in the development of atherosclerosis.
As coronary artery disease progresses, the coronary vessels become narrower, decreasing blood supply to the myocardium. This lack of blood supply leads to ischemia and eventually necrosis (cell death) of the myocardium. If loss of muscle tissue occurs (MI), the heart muscle is unable to pump effectively and cardiac output is reduced. Cardiac dysrhythmias and death may occur if medical intervention is not obtained.
Signs and Symptoms
Signs and symptoms of coronary artery disease are related to the lack of oxygen supply to the myocardium and inability of the heart to pump blood effectively to oxygenate tissues and cells (Box 21-1). Angina pectoris, acute coronary syndrome (ACS), or sudden cardiac death may occur.
The condition is called stable angina when symptoms only appear with activity. Unstable angina occurs when symptoms occur even at rest. Acute coronary syndrome occurs when ischemic symptoms are prolonged and are not quickly relieved. It is an umbrella term for unstable angina and acute ischemic MI with or without ST-segment elevation on the electrocardiogram (ECG).
Diagnosis
Diagnosis of coronary artery disease is accomplished through tests, such as ECG, echocardiogram, cardiac stress test, cardiac angiography (cardiac catheterization), cardiac computed tomography (CT) for calcium index, or magnetic resonance angiogram.
Treatment
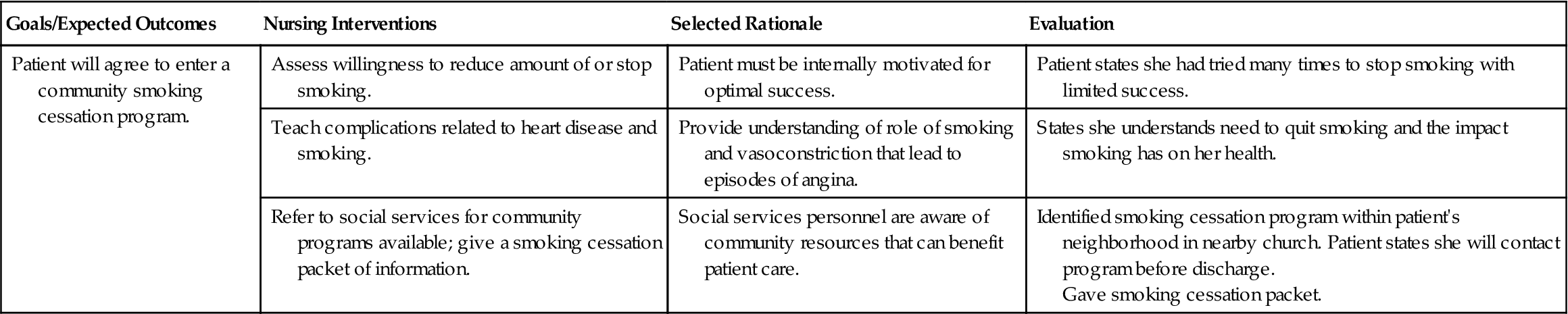
A low-fat diet, weight control, and exercise are prescribed to lower cholesterol and total lipids (American Heart Association, 2009a). If elevated cholesterol and  triglyceride levels cannot be lowered by a low-fat diet and exercise, lipid-lowering drugs are prescribed (Table 21-1). These medications are not effective alone and may not reduce cholesterol levels to a point of eliminating the risk for coronary artery disease. Several herbs and supplements have shown the ability to lower cholesterol. Advise patients to consult with their physician before taking over-the-counter medications or herbs.
triglyceride levels cannot be lowered by a low-fat diet and exercise, lipid-lowering drugs are prescribed (Table 21-1). These medications are not effective alone and may not reduce cholesterol levels to a point of eliminating the risk for coronary artery disease. Several herbs and supplements have shown the ability to lower cholesterol. Advise patients to consult with their physician before taking over-the-counter medications or herbs.
Table 21-1
Drugs Commonly Used to Treat Hypercholesterolemia
| Drug | Action | Common Side Effects | Usual Adult Dosage | Nursing Interventions |
| Bile Acid Sequestrants | ||||
| Fibric Acid Derivatives | ||||
| HMG-CoA Reductase Inhibitors (Statins) | ||||
| Cholesterol Absorption Inhibitor | ||||
| Niacin | ||||
Nursing Management
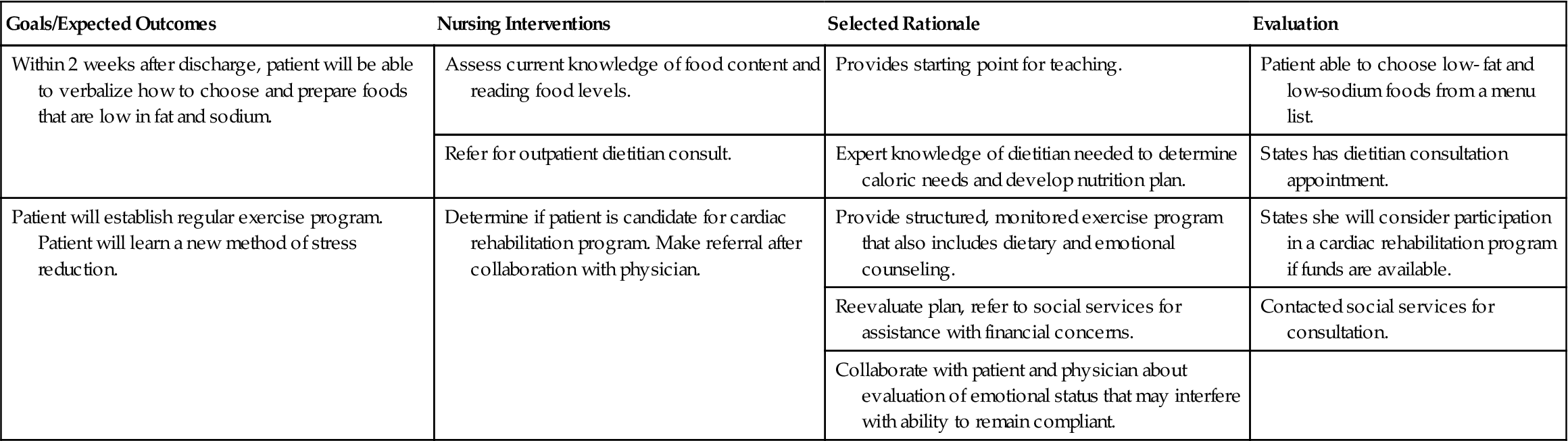
Patients should be encouraged to adopt a healthy lifestyle, including exercise and a diet low in saturated fat. Obtain a referral to a dietitian and assist the patient by reinforcing the need for changes in dietary habits. A cardiac rehabilitation program referral is very helpful. The program will help the patient choose an exercise regimen that he can manage on a long-term basis. Emphasize the importance of maintaining a normal body weight.
If the patient is on a statin drug to lower cholesterol, remind him that he needs to have blood drawn periodically to determine if the drug is effective and to monitor for serious side effects.
Angina Pectoris
Angina pectoris (chest pain) occurs when blood supply to the heart is decreased or totally obstructed. The ischemia (inadequate blood and oxygen supply) of the heart tissue causes pain. Angina may be caused by atherosclerosis or arterial spasm. The decreased blood flow is caused by atherosclerotic plaque narrowing the artery or by arterial spasm (sudden constriction). Any activity that increases the heart’s workload increases its need for oxygen. When the occluded coronary arteries cannot deliver adequate amounts of blood to meet normal needs, the patient experiences an angina attack. Attacks can be precipitated by physical exertion, emotional excitement, eating a heavy meal, exposure to cold, infection, or any disorder or activity that increases the oxygen demand and consumption or decreases the availability of oxygen to the myocardial tissue. When the patient’s angina is no longer adequately controlled by medication and the attacks become more frequent or severe, surgery may be indicated to prevent a life-threatening MI.
Signs, Symptoms, and Diagnosis
Anginal pain or discomfort may vary in individuals, but in most cases it is described as a dull pressure or ache under the sternum or pain that radiates to the neck or jaw. The pain may also radiate down one or both arms. Angina sensation is seldom sharp or stabbing. The feeling may be described as suffocating. The pain can occur between the shoulder blades. In women, there may be no chest pain, but just a tenderness to touch or a burning or tingling sensation. Patients may think they are experiencing indigestion or esophageal reflux.
There are three types of angina:
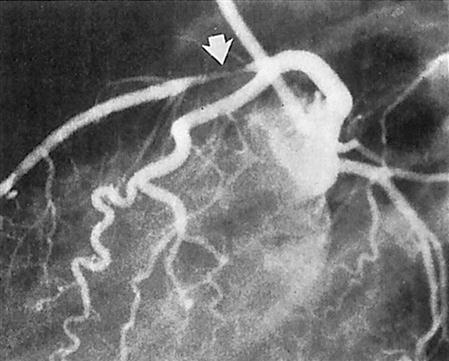
Medical diagnosis is established on the basis of history, clinical signs and symptoms, and whether rest and nitroglycerin provide relief during an acute attack. Response of the heart muscle to increased oxygen demands can be determined by exercise stress testing. Cardiac catheterization with coronary angiography may be performed (Figure 21-2). Echocardiography may be ordered to rule out a valve disorder or to evaluate left ventricular function. Laboratory levels of blood lipids will be ordered, and cardiac enzymes may be ordered to rule out an MI. An electrocardiogram is a standard diagnostic procedure.
Treatment
 The treatment of angina pectoris is mostly symptomatic, with emphasis on eliminating those factors that are known to precipitate an attack in the individual patient. With guidance and teaching, the patient may soon be able to correlate certain activities with an attack and thereby learn to avoid one whenever possible. Nitroglycerin, nitrates, calcium antagonists, and beta blockers are used in combination with drugs to lower cholesterol and prevent platelet aggregation. A low daily dose of aspirin (81 mg or 325 mg) may be prescribed for the treatment of CAD. Aspirin helps prevent clotting and may prevent a thrombus that could cause an MI. If the patient is allergic to aspirin, clopidogrel (Plavix) is prescribed. Nitroglycerin administered sublingually is the most common drug for treatment of angina. An aerosol spray and a buccal form of the drug are also available.
The treatment of angina pectoris is mostly symptomatic, with emphasis on eliminating those factors that are known to precipitate an attack in the individual patient. With guidance and teaching, the patient may soon be able to correlate certain activities with an attack and thereby learn to avoid one whenever possible. Nitroglycerin, nitrates, calcium antagonists, and beta blockers are used in combination with drugs to lower cholesterol and prevent platelet aggregation. A low daily dose of aspirin (81 mg or 325 mg) may be prescribed for the treatment of CAD. Aspirin helps prevent clotting and may prevent a thrombus that could cause an MI. If the patient is allergic to aspirin, clopidogrel (Plavix) is prescribed. Nitroglycerin administered sublingually is the most common drug for treatment of angina. An aerosol spray and a buccal form of the drug are also available.
Nursing Management
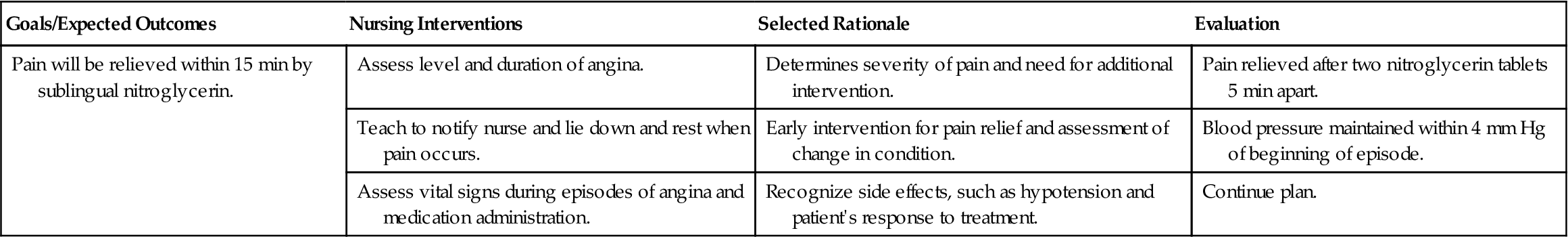
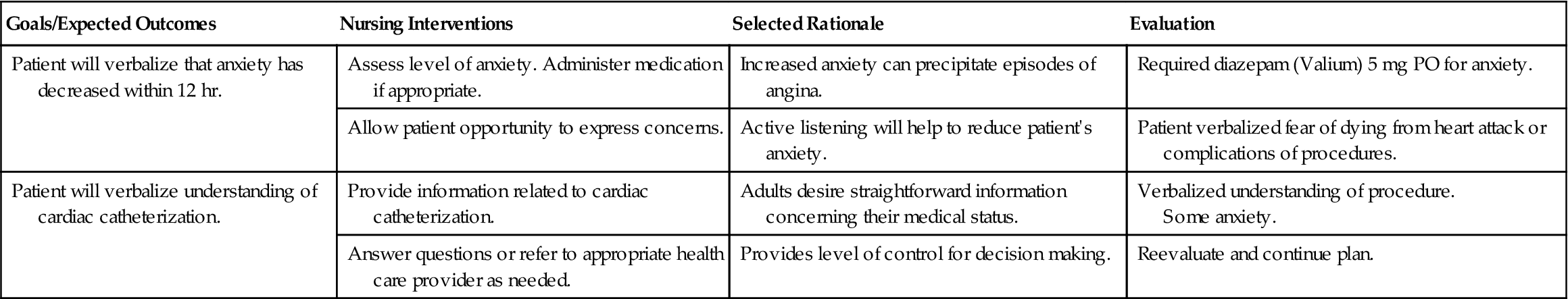
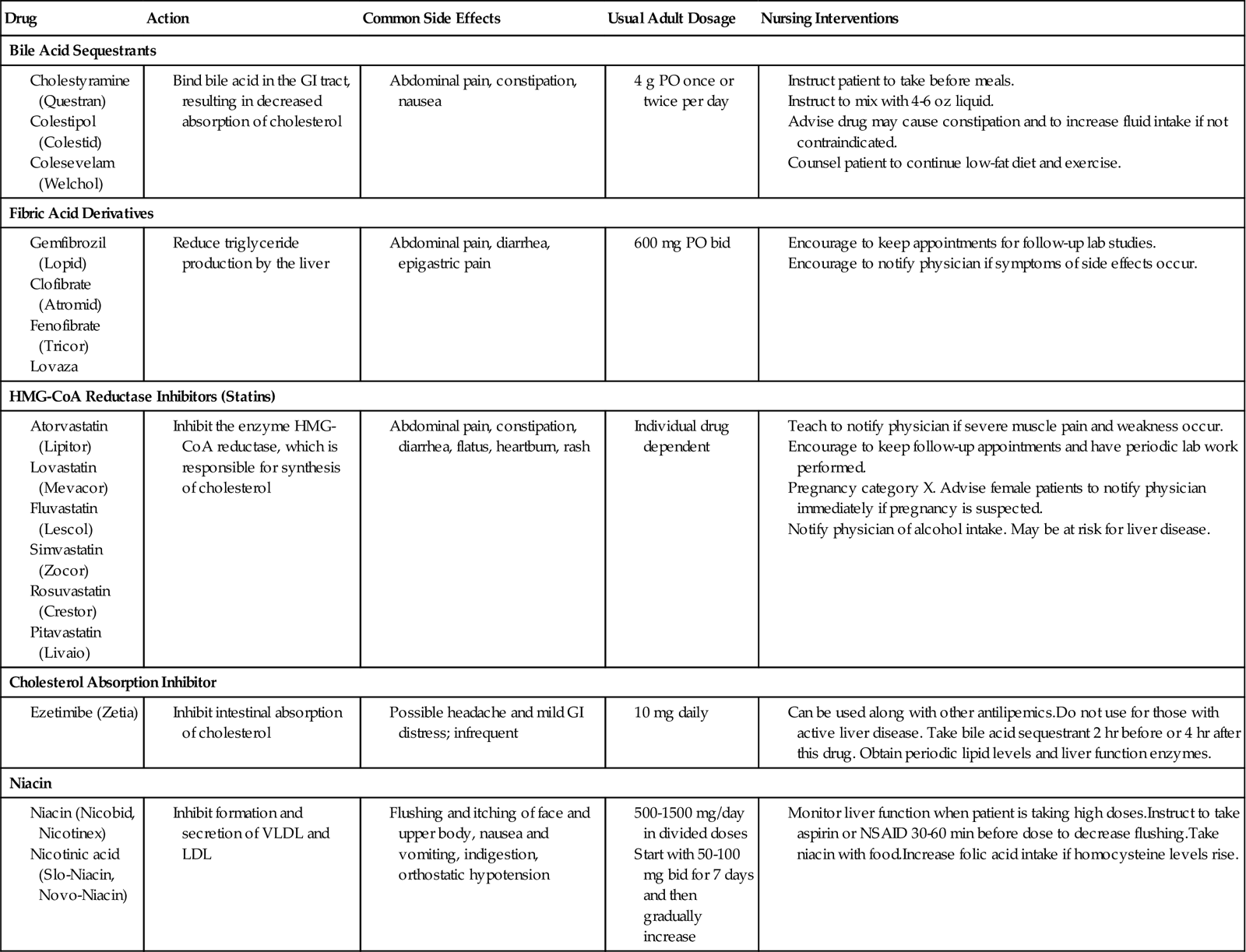
Collect data that assist in determining the type of angina the patient is experiencing. Patients with a history of angina may experience increased episodes when exposed to very cold environments. Externally cold temperatures result in vasoconstriction. The patient should be instructed to wear warm clothing when exposed to cold and may consider remaining indoors when the weather is extremely chilly. Nursing interventions for selected problems related to angina pectoris are summarized in  Nursing Care Plan 21-1.
Nursing Care Plan 21-1.
Acute Coronary Syndrome and Myocardial Infarction
If ischemia is prolonged and not quickly reversed, acute coronary syndrome (ACS) occurs. ACS includes unstable angina, non–ST segment elevation myocardial infarction (NSTEMI) and ST segment elevation myocardial infarction (STEMI). All patients with heart disease should be taught the signs of MI and be advised that the best survival rate is directly related to obtaining medical attention as quickly as possible. About 1,200,000 Americans experience an MI annually. Although males outnumber females, females die more frequently after an MI. According to the American Heart Association, heart disease is the leading cause of death among American women, claiming about 500,000 lives each year. The incidence of heart disease, including MI, continues to rise among women. Women are more likely to experience heart attacks after reaching menopause; however, poor dietary habits, sedentary lifestyle, and increased levels of stress contribute to the development of cardiovascular disease earlier in life for an increasing number of women.