Section Twenty Ophthalmic Procedures
PROCEDURE 153 Assessing Visual Acuity
PROCEDURE 154 Contact Lens Removal
PROCEDURE 156 Fluorescein Staining of Eyes
PROCEDURE 157 Ophthalmic Foreign Body Removal
PROCEDURE 158 Instillation of Eye Medications
PROCEDURE 153 Assessing Visual Acuity
CONTRAINDICATIONS AND CAUTIONS
1. Visual acuity testing should not precede treatment in patients whom have had chemical exposure to the eye. Copious saline irrigation should be performed immediately for all chemical exposures; tap water is usually the first available fluid which should be followed by a balanced salt solution buffered to a pH of approximately 7 (see Procedure 155). Visual acuity testing is performed after irrigation when chemical exposure occurs.
2. The abbreviations for right eye (oculus dexter; O.D.), left eye (oculus sinister; O.S.), and both eyes (oculi uterque; O.U.) are error prone and their use is discouraged by the Institute for Safe Medication Practices (ISMP, 2006).
EQUIPMENT
Symbol chart such a tumbling “E” chart or a picture chart (for illiterate patients or preschool children)
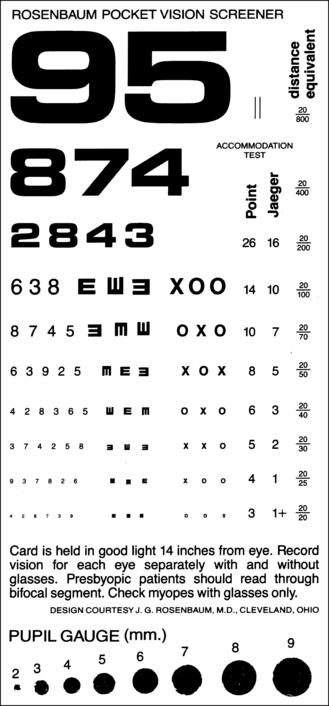
Near-vision acuity chart (Figure 153-1)
Eye spoon, patch, or opaque card to cover the eye not being tested (optional)
Marked distance of 20 or 10 feet for testing
PATIENT PREPARATION
1. Instill a topical ophthalmic anesthetic (if prescribed) to increase the patient’s comfort during the examination (optional).
2. Instruct the patient to occlude one eye during the vision test by using the eye spoon, patch, opaque card, or hand. Clean to remove copious discharge before visual acuity testing but after obtaining any necessary culture specimens. If there is discharge from the eye, use a disposable opaque card, and turn it over to the fresh surface when testing the other eye to prevent contamination. The patient should wash his or her hands after the procedure.
3. Instruct the patient not to apply excessive pressure when covering the eye because blurred vision may result.
4. Patients using a cupped hand should keep their fingers together to prevent a false reading caused by using binocular vision. The cupped hand may be a poor choice due to intentional or inadvertent peeking through the fingers.
5. Leave glasses or contact lenses in place during the examination if not contraindicated by injury. When the patient’s glasses or contact lenses are not available, document the results as “uncorrected visual acuity.”
PROCEDURAL STEPS
1. Each eye is tested separately, with and without glasses.
2. Letters and objects are of a size that can be seen by the normal eye at a distance of 6 meters (20 feet) from the chart.
3. Letters appear in rows and are arranged so the normal eye can see them at distances of 9, 12, 15 meters (30, 40, 50 feet), and so forth.
4. A person who can identify letters of the size 6 at 6 meters (20 at 20 feet) is said to have 6/6 (20/20) vision.
Standard Method: Distant Visual Acuity
1. Sit or stand the patient at a marked distance of 20 feet from the standard Snellen chart with the chart positioned at eye level.
2. Test the vision of one eye at a time. Test the unaffected eye first to serve as a control.
3. Ask the patient to read the Snellen chart starting with the top line and working down until the letters are no longer legible.
4. Record the lowest line the patient is able to read, including the number of mistakes made on that line. For example, right eye, 20/20 means the patient can read the 20/20 line with no mistakes. Left eye, 20/25 –1 means the patient can read the 20/25 line with one mistake. Visual acuity is recorded as a fraction. The numerator represents the distance to the chart, and the denominator represents the distance from which a normal eye can read the lines. For example, 20/50 means that the patient can read at 20 feet what a person with 20/20 vision can read at 50 feet. If the patient is unable to read the first line of the Snellen chart at 20 feet, he or she may be placed at a distance of 10 feet from the chart and asked to read the lines. The acuity is then recorded as 10/50.
5. Repeat steps 3 and 4 for the opposite eye and for both eyes together.
Alternative Methods: Near Vision
1. Hand-held near-vision testing cards are commercially available when distance testing is not possible, such as the Rosenbaum near-vision chart. This is used for patients who are unable to stand (see Figure 153-1). The card is held 14 inches away from the patient. Attaching a 14-inch string to the card facilitates correct usage; however, patients may choose their own distance. The same procedure is used as for the Snellen chart testing.
2. If commercially prepared charts are unavailable, have the patient read a newspaper or another document with similarly-sized print and record the distance at which the patient is able to read the print.
3. Occasionally, patients who wear glasses or contact lenses carry the prescription in their wallet. This may serve as a gross baseline of visual acuity.
4. The pinhole method may be used to assess a refractive error when the patient’s glasses or contact lenses are not available. The patient reads the Snellen chart while looking through pinholes in an opaque card. If the visual acuity improves, the decreased visual acuity may be attributed to a refractive error. When there is no improvement, causes other than refractive error should be considered.
5. If the patient is unable to read the top line of the Snellen chart (vision is less than 20/200 [6/60]), the following visual tests may be performed and recorded as follows:
AGE-SPECIFIC CONSIDERATIONS
1. Use a symbol chart for illiterate patients or preschool children. Two symbol charts are available as pictures, such as Allen picture card or the Tumbling E test, with the letter E turned in four different directions. The patient is asked either to point a finger in the direction of the E bars or to identify the picture symbol printed on the chart. Follow the same procedure as for the Snellen chart.
2. Infants and young children can best be evaluated while sitting upright in the arms of their parents or caregivers.
3. Visual acuity testing for the preschool child may be inaccurate and is dependent on the cognitive development of the child. Generally, visual acuity reaches the adult level of 20/20 vision between ages 3 and 5.
4. To measure vision in infants more than 6 weeks old, assess their ability to fixate and follow a target. The human face works well as a target; in addition, brightly colored toys may be used (Olitsky & Nelson, 2004).
5. Snellen charts do not accurately test vision in older patients with complaints of faded objects and decreased vision with bright light (Miller & Magnante, 2004).
Institute for Safe Medication Practices (ISMP). (2006). ISMP’s list of error-prone abbreviations, symbols, and dose designations. Retrieved September 3, 2007, from http://www.ismp.org/Tools/errorproneabbreviations.pdf
Miller D., Magnante P. Optics of the normal eye. In: Yanoff M., ed. Ophthalmology. 2nd. St Louis: Mosby; 2004:59–67. Retrieved February 17, 2007, from URL:/das/book/view/60191306–2/1197/14.html/top
Olitsky S., Nelson L. Disorders of the eye. In: Behrman R.E., ed. Nelson textbook of pediatrics. 17th ed. Philadelphia: Saunders; 2004:2083–2126.
PROCEDURE 154 Contact Lens Removal
CONTRAINDICATIONS AND CAUTIONS
1. Never use force to remove a lens. If you have difficulty, slide the lens onto the sclera and notify the physician.
2. Look for “lost” lenses in the upper cul-de-sac of the eye. This is their most common hiding place.
3. Do not replace the lens until a physician examines the patient’s eyes.
4. If you suspect that your patient has a penetrating injury to the eye, do not manipulate the eye in any way.
5. If the eyes appear dry, instill several drops of sterile saline solution from a single-use dropper bottle and wait a few minutes before removing the lens to help prevent corneal damage.
6. Do not instill medications while the patient is wearing contact lenses. Contact lenses can combine chemically with the medication and cause eye irritation or lens damage.
7. Do not use saline solution with preservatives or tap water because they may damage the lenses.
PATIENT PREPARATION
1. Place the patient in a supine or semi-Fowler’s position.
2. Place a clean towel around the neck and across the chest.
3. Remove any glass particles with cellophane tape. Roll the tape so the adhesive is on the outside and gently touch it against the patient’s closed eye to remove glass particles.
4. Gently remove blood, dirt, or makeup from the eyelids with a cotton ball moistened with saline solution.
5. Place several milliliters of sterile saline solution in each specimen container and label the containers left and right. If a contact lens case is used, place a few drops of saline solution in each compartment. Label the container(s) with the patient’s name.
PROCEDURAL STEPS
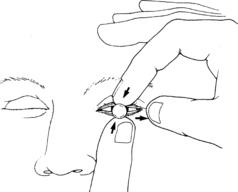
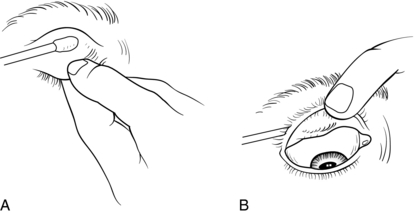
Hard Lenses
1. Lubricate the eye with artificial tears.
2. Use one thumb to pull the patient’s upper eyelid toward the orbital rim.
3. Place your other thumb on the lower lid, gently move the lids toward each other to trap the lens edge, and break the suction (Figure 154-1).
4. Cup your hand below the eye to catch the lens when it pops out.
5. Place the lens in an appropriate specimen container or contact lens case compartment.
6. Remove and care for the other lens by use of the same technique.
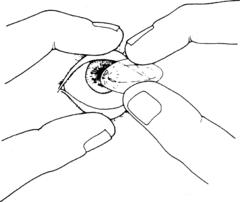
Soft Lenses
1. Lubricate the eye with artificial tears.
2. Raise the upper eyelid with your index finger and hold it against the orbital rim.
3. Lightly place your thumb on the lower lid and pull it down.
4. Have the patient look up and slide the lens down gently with the index finger of your other hand.
5. Pinch the lens together with your thumb and index finger and lift it out of the patient’s eye (Figure 154-2).
6. Place the lens in the appropriate specimen container or the contact lens case compartment.
7. Remove and care for the other lens using the same technique.
Suction Cup Removal of Hard and Soft Lenses
1. Wet the suction cup with a drop of sterile saline solution.
2. Gently pull up the patient’s upper eyelid with your index finger and pull the lower lid down with your thumb.
3. Press the suction cup gently to the center of the lens or squeeze nasal bulb syringe and gently place tip to center of lens and release slight suction to pull lens loose (Figure 154-3).
4. Pull the suction cup and the lens away from the eye in a straight line.
5. Place the lens in the appropriate specimen container or the contact lens case compartment.
6. Remove and care for the other lens using the same technique.
PROCEDURE 155 Eye Irrigation
Eye irrigation is also known as eye flushing.
CONTRAINDICATIONS AND CAUTIONS
1. Do not delay irrigation when a chemical exposure occurs. Irrigation should be initiated immediately and should be continued by caregivers before arrival at the emergency department. Until the causative agent is known, exposures should be presumed to be acid or alkaline substances (Brunette, 2006).
2. It is critical to identify the causative agent and to obtain an initial pH. In general, alkaline substances have a pH greater than 12 and acidic substances have a pH less than 2 (Brunette, 2006).
3. Lactated Ringer’s solution is preferred over normal saline. The pH of lactated Ringer’s is 6 to 7.5, which is closer to the pH of tears (7.1) than that of normal saline, which may range from 4.5 to 7 (MorTan, n.d.).
4. Use caution when a penetrating injury is present or suspected, and irrigate gently. Do not use a Morgan lens when there has been a penetrating injury or a ruptured globe is suspected or present.
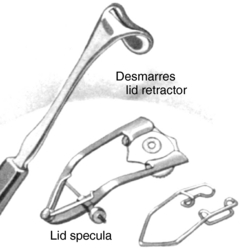
5. Paper clips have been used as modified lid retractors; however, they may chip after twisting, causing metal fragments to enter the eye (Knoop, Dennis, & Hedges, 2004).
6. If a patient has contaminated his or her eye with a cyanoacrylate adhesive (e.g., Super Glue), evaluation by an ophthalmologist is recommended. Separation of glued eyelashes and gentle traction on the eyeball can be used, but the eyelids should not be forced open. Use of other agents to dissolve the adhesive is not recommended. Irrigation is not the first line of treatment.
7. An ophthalmology consultation may be necessary, depending on the type and the duration of the exposure as well as the clinical findings.
EQUIPMENT
Sterile lactated Ringer’s solution (1000-ml intravenous [IV] bag)
18- or 20-G over-the-needle catheter with the stylet removed
Medi-Duct ocular fluid management system used with Morgan lens (optional)
Morgan lens delivery tubing (optional)
Gauze dressings or a commercially prepared eye patch
Shampoo board or sink area (optional)
Desmarres retractor (Figure 155-1)
PATIENT PREPARATION
1. Instill the prescribed topical ophthalmic anesthetic into the affected eye.
2. If a chemical exposure has occurred, obtain a baseline pH measurement of the eye by placing pH paper in the conjunctival sac.
3. Another person may need to hold the eyelids open manually or with a retractor if an irrigating lens is not used.
4. Inform the patient that the eye irrigation may cause postnasal drip. Offer tissues for use as needed.
5. Use a gown or draped towels to protect the patient from excessive dampness during the procedure.
6. Position a basin or a large bag to catch the irrigant or position the patient over a sink. Using a shampoo board under the patient’s head is another method to facilitate collection of the irrigant. Place the patient in a supine position. Place towels under the patient’s neck to increase comfort. If the Medi-Duct fluid wicking drainage collector or shampoo boards are not readily available, treatment may begin with cooperative patients sitting and leaning over a sink or basin. There is an increased tendency for the irrigating lens to fall out in this position, especially if blinking occurs or flow is rapid.
PROCEDURAL STEPS
Manual Irrigation
1. Spike the IV tubing into the IV fluid and attach the catheter or irrigating syringe device and prime the tubing.
2. Use gauze pads to hold the eyelids open for irrigation if the patient is unable to do so. A lid retractor may be used to separate the eyelids and allow irrigation.
3. Direct the flow of the irrigant onto the conjunctiva from the inner to the outer canthus, avoid directing the stream directly onto the cornea, which can be harmful (Figure 155-2).
4. Instruct the patient to roll the eyes in all directions to ensure total eye irrigation.
5. For acidic exposure, irrigate with a minimum of 1000 ml of lactated Ringer’s solution per eye. Acids (except hydrofluoric and heavy metal acids) are quickly neutralized by the proteins of the eye surface. After the eye is irrigated, acids cause no further damage (Knoop et al., 2004).
6. Irrigate alkaline injuries with a minimum of 2 L of lactated Ringer’s or normal saline solution per eye over 1 hour. Extensive irrigation is required because alkaline substances, hydrofluoric acid, and heavy-metal acids can penetrate the cornea rapidly and continue to cause damage for days (Knoop et al., 2004).
7. Measure the pH of the eye at intervals during the irrigation by placing pH paper in the conjunctival sac. Continued irrigation is needed until the pH of the tear film is neutral, 7.5 to 8 (MorTan, n.d.). The normal conjunctival pH is 7.1 (MorTan, n.d.). If the pH remains alkaline, irrigation should be continued.
8. * Evert the eyelid and remove traces of alkali by using a wet cotton-tipped applicator to swab the fornices (Figure 155-3).
9. Check the patient’s comfort level periodically. Instill additional ophthalmic anesthetic as necessary.
10. Recheck the conjunctival pH approximately 20 minutes after completion of irrigation and periodically as indicated to ensure that it remains in the normal range. Inadequate irrigation or improper swabbing of the fornices can cause delayed changes in the pH (Knoop et al., 2004).
11. Obtain a baseline visual acuity level (see Procedure 153).
12. Prepare the patient for a corneal examination to determine the extent of the injury (see Procedure 156).
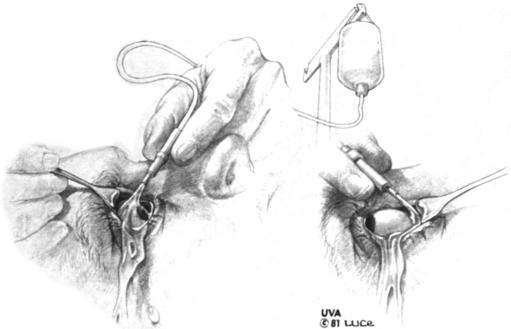
Figure 155-2 Irrigation using a Desmarres retractor.
(From Fogle, J. A., & Spyker, D. A. [1990]. Management of chemical and drug injury to the eye. In L. M. Haddad & J. F. Winchester [Eds.], Clinical management of poisoning and drug overdose [2nd ed., p. 372]. Philadelphia: Saunders.)
Irrigating or Morgan Therapeutic Lens
1. The irrigating lens fits onto the cornea like a soft contact lens and provides optimal continuous irrigation of the corneal surface while increasing patient comfort. The lens allows the patient to close the eyelids and decreases the risk of iatrogenic trauma often encountered during a difficult irrigation (Figure 155-4).
2. Spike the IV tubing into the IV fluid (lactated Ringer’s is preferred), attach the Morgan lens, and prime. Ask the patient to look downward. Grasp the upper eyelid and retract it upward. Holding the lens between the thumb and forefinger of your dominant hand, insert the upper portion of the lens under the upper eyelid with the IV fluid running. Ask the patient to look down. Retract the lower eyelid and place the lower portion of the lens onto the cornea. The insertion process is similar to that used to insert a contact lens.
3. Adjust the flow of IV fluid to a level tolerated well by the patient, and proceed with the continuous irrigation. A wide-open flow may create too much pressure and actually create more discomfort for the patient. Remind the patient to keep the eyes closed to ensure that the lenses stay in the eyes.
4. Tape the irrigation tubing to the patient’s forehead to prevent accidental dislodgement of the lens (optional).
5. See steps 4 through 10 in the Manual Irrigation section of this procedure.
6. Remove the irrigation lens with the IV fluid running. Ask the patient to look upward, retract the lower lid, lift one side of the lens to break the suction, and gently slide the lens from the cornea.
AGE-SPECIFIC CONSIDERATIONS
1. Patients with chronic diseases, such as congestive heart failure or chronic obstructive lung disease, may need accommodations for positioning during irrigation. A supine position may not be tolerated.
2. The irrigating lens (Morgan lens) has been used without difficulty on infants and young children since the dimensions of the eye change little from infancy to adulthood (MorTan, n.d.).
PATIENT TEACHING
1. Following irrigation, you may experience a burning sensation in the eyes similar to that which occurs after prolonged exposure to chlorinated water in a swimming pool. The sensation is self-limiting and usually subsides about 1 hour after tear production resumes.
2. Take analgesics as directed. A topical anesthetic cannot be used at home, because continued use prevents healing and may mask pain related to complications.
3. Return to the emergency department for increasing pain, decreasing vision, or other new symptoms. See an ophthalmologist as directed.
4. Use protective eyewear when appropriate to prevent future injuries.
5. Any functional decrease in vision of an eye (whether patched or medicated or by the injury or disease) causes monocularity to some extent with resultant loss of peripheral vision, inadequate depth perception due to loss of triangulation and a “blind spot.” All of these effects can lead to injury and you should not drive, operate machinery, or perform other risky tasks until cleared by a physician.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree