CHAPTER 20. Epidemiology and Mechanisms of Injury
Cynthia Blank-Reid and Paul C. Reid Sr.
Epidemiology and mechanism of injury (MOI) are separate and distinct disciplines, yet they are closely intertwined in the trauma literature. Epidemiology is the branch of medicine that studies the causes, distribution, and control of disease in populations. 2 It defines the scope of injuries in terms of their incidence and identifies associated factors and determinants of specific types of injury. An understanding of MOI, the study of how energy is transferred from the environment to the individual, equips health care providers with the knowledge to anticipate injuries, diagnosis, treatments, and complications of traumatic injury. Common patterns of injury are observed with specific mechanisms, and this knowledge can assist with the rapid detection of suspected injuries. Unless death occurs immediately, the outcome of an injured person depends not only on injury severity, but also on the speed and appropriateness of treatment.
Knowledge of both epidemiology and MOI helps shape health care by allowing providers to deliver evidence-based care and understand the populations who are at risk for particular injuries and those who need to be targeted for specific prevention programs. It also provides the ability to evaluate the effectiveness of these programs over time. Nurses who care for trauma patients clearly recognize the need for prevention and control strategies to curb mortality and morbidity. Perception of trauma as preventable events rather than acts of random unexpectedness (“accidents”) is essential for the success of prevention programs. Throughout this chapter the terms trauma and injury are used interchangeably.
EPIDEMIOLOGY
The epidemiology of trauma is particularly important because of the implications for social and public policy, legislation, and injury prevention programs. Understanding the scope of any problem is central to successful planning and implementation of legal, environmental, and educational remedies. Data elements such as incidence, prevalence, age, sex, race or ethnicity, geographic distribution, and morbidity or mortality are the sources of epidemiologic surveillance and serve to quantify aggregates.
Trauma is a disease that remains a leading cause of death for Americans of all ages regardless of gender, race, or economic status. Millions of Americans are injured each year and survive. 4 Whether the injury is fatal or nonfatal, the patient and his or her family, friends, and employers will all have to face adjustments in their lives. Refer to Table 20-1, the Centers for Disease Control and Prevention’s (CDC’s) 10 leading causes of death by age-group.
| WISQARS Produced By: Office of Statistics and Programming, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. |
| Data Source: National Center for Health Statistics (NCHS), National Vital Statistics System. |
| HIV, Human immunodeficiency virus; SIDS, sudden infant death syndrome. |
 |
Trauma is the leading cause of death for children over 1 year and adults under 45 years of age. Trauma is also the main cause for loss of work years because it predominately affects a younger population who are in their prime working years. The great social, personal, and economic costs associated with traumatic injuries makes trauma a major public health problem in the United States.
Trauma in the United States
Age
For children under 1 year old, the leading cause of a fatal injury is unintentional suffocation due to choking or strangulation. Motor vehicle crashes (MVCs) are a leading cause of death throughout childhood; the incidence is particularly high in 1- to 3-year-olds, who are too frequently unrestrained passengers.
The high rate of injury for individuals 15 to 24 years of age may be caused by experimentation with drugs and alcohol in combination with poor judgment and risk-taking behaviors. The risk for MVC is higher among 16- to 19-year-olds than any other age-group. Drivers in this age-group are four times more likely than older drivers to crash, based on number of miles driven. 18 Teens are at risk because of the following:
• Inexperience: They often fail to recognize or underestimate the dangers in hazardous situations. They are more likely to speed, run red lights, make illegal turns, ride with an intoxicated driver, and drive after using alcohol or drugs. 19
The 65 and older age-group is the fastest growing segment of the U.S. population. As the U.S. population grows older, more and more people become vulnerable and are dependent on others to meet their most basic needs. Individuals more than 75 years of age have the highest death rate from injuries, which is attributed to multiple factors, including their frailer state of health and preexisting medical conditions. Age has been shown to be independently associated with increased mortality after trauma. Falls continue to be the most common cause of nonfatal and fatal injuries in adults ages 65 and older. 5 Drivers who are 65 and older have the highest death rate per mile driven except for teenage drivers. Older drivers drive less, but they are more likely to crash and die in the collision. 10. and 13. Estimates indicate that more than 40 million older adults will be licensed drivers in 2020. 4. and 22. In addition, age is a major factor in determining the risk for a cervical spine injury in auto-pedestrian injuries. Those over the age of 65 years are 12 to 14 times more likely to sustain a cervical spine injury than pediatric patients. 32
Of the 11 million people age 65 years and older who are hospitalized annually, a significant percentage (52%) of injury-related admissions are due to fractures. 4. and 22. Of interest is that medical costs for the geriatric population are 2.5 times greater than for younger patients with similar injuries; this is due to longer lengths of stay, higher incidence of complications, and more intensive care unit days. 22. and 23.
Gender
Gender, along with age variances, is related to the incidence and type of injury incurred. Males are 2.5 times more likely to be injured than females. This statistic is significant because of their participation in more hazardous activities and greater risk taking. This fact continues throughout the life span, as rates for motor vehicle (MV)–related injuries are twice as high for older men than women. 5 The pedestrian fatality rate is also more than twice as high for men as for women. 5
Race
Injury and death rates vary with race and income. The reasons for these variations are multifactorial and not completely understood. However, knowledge of the differences observed has been used to target prevention programs toward specific populations or geographic areas. For African Americans and whites, no matter what the MOI, the higher the income, the lower the death rate. The number of MVCs decreases in a depressed economy, whereas homicides and suicides increase. The highest homicide rate occurs in the African American population, the highest suicide rate is seen in whites and Native Americans and the lowest death rate occurs in Asian Americans.
African Americans have a pedestrian death rate that is 1.7 times that of whites. 5 African American men age 65 and older have one of the highest MV-related death rates when sorted by age, sex, and race. 5 Homicide is the leading cause of death for African Americans age 10 to 24 years of age. 5 The drowning rate for 5- to 14-year-old African Americans is 3.2 times higher than that of whites. 3. and 11.
Asian-Pacific and Native American women age 65 years and older have the highest death rates when sorted by age, sex, and race. 5 Homicide is the second leading cause of death for Asian-Pacific Islanders for those age 10 to 24 years. 5
Hispanics have a mortality rate 1.8 times higher than non-Hispanics if they are a pedestrian who has been injured. 5 Homicide is the second leading cause of death for Hispanics among people age 10 to 24 years. 5
Native Americans 19 years or age and younger are at greater risk for preventable injury-related deaths than are all other children and youth in the United States. They have twice the average rate of traumatic deaths than their counterparts in any other racial group. Injuries and violence account for 75% of all deaths among Native Americans in this age-group. MVCs are the leading cause of fatality followed by homicide, drowning, and fires. 4 The rates for pedestrian deaths in auto-pedestrian injuries are three times higher for Native Americans and Alaska Natives than whites. 5 The drowning rate overall for Native Americans and Alaska Natives is 1.8 times higher than that for whites; in children age 5 to 14 years the drowning rate is 2.6 times higher. 3. and 11. Native American men age 20 years and older are (1) twice as likely to die from an MVC, (2) nearly twice as likely to die from fire and burn injuries, and (3) five times more likely to drown than their counterparts in other races. They are also four times more likely to commit suicide and three times more likely to be murdered. 9
Firearm-Related Injuries
The CDC began tracking firearm injuries in the early 1960s. Firearm violence and firearm-related deaths have been increasing at a steady rate for over 40 years. 5 Firearm injury disproportionately affects young people, resulting in lives cut short or forever affected as a result of their use. Firearms (especially handguns) are effective lethal weapons with the capability to escalate often-impulsive acts of interpersonal violence or suicidal thoughts into death. The United States has wrestled with firearms and the consequences of their use and misuse for years. Compared with other industrialized countries, the firearm death rate in the United States is eight times the average rate of its economic counterparts. 21 Among all industrialized countries, more men are killed by firearms than women; however, women in the United States die at a much higher rate from firearm injuries then their counterparts in other high-income countries. 21
Alcohol
Alcohol plays a significant role in all types of trauma, including MVCs, family violence, suicides, homicides, and altercations. Alcohol alters judgment and coordination, so it frequently contributes to injury-producing events.
An alcohol-related MVC kills someone every 31 minutes and nonfatally injures someone every 2 minutes. 8. and 26. The CDC’s research has found that about 68% of the children killed in alcohol-related crashes were riding in cars driven by drivers who had been drinking. 5 One study demonstrated that child passenger restraint use decreased as the BAC of the child’s driver increased. 29
Geography and Chronology
Geographic differences exist in injury mortality. Physical environment or geographic area also characterizes injury rates. Homicides and suicides occur more often in urban areas, whereas unintentional injuries are more numerous in rural areas. Injury and death rates are greater on weekends with the peak on Saturday. More injuries are seen in July—probably as a result of summer recreational activities.
MECHANISM OF INJURY
Trauma is now recognized as a disease process with MOI as part of its etiology. Strong assessment skills are essential for health care providers because treatment of trauma patients is contingent on identifying all injuries. Unfortunately, even when the clinician has strong assessment skills some injuries go undetected if the “index of suspicion” is not sufficient. Understanding MOI and maintaining a high index of suspicion enable caregivers to predict and locate occult injuries more quickly and save time initiating essential treatment. Injury should be considered present until definitively ruled out in the hospital setting.
Human beings are exposed to potential injury in multiple forms during the course of a normal day. Injury, defined as trauma or damage to a part of the body, occurs when an uncontrolled or acute source of energy makes contact with the body and the body cannot tolerate exposure to it. Energy originates from numerous sources, including kinetic (motion or mechanical), chemical, electrical, thermal, and radiation. Absence of heat and oxygen causes injuries such as frostbite, drowning, or suffocation. Kinetic energy is defined as energy that results from motion. 14.22. and 24. The majority of traumatic injuries are caused by absorption of kinetic energy. Box 20-1 defines essential concepts for understanding mechanisms of injury.
Box 20-1




Get Clinical Tree app for offline access
E ssential C oncepts for M echanisms of I njury
| Acceleration | Increase in velocity or speed of a moving object. |
|---|---|
| Acceleration-deceleration | Increase in velocity or speed of object followed by decrease in velocity or speed. |
| Axial loading | Injury occurs when force is applied upward and downward with no posterior or lateral bending of the neck. |
| Cavitation | Creation of temporary cavity as tissues are stretched and compressed. |
| Compression | Squeezing inward pressure. |
| Compressive strength | Ability to resist squeezing forces or inward pressure. |
| Deceleration | Decrease in velocity or speed of a moving object. |
| Distraction | Separation of spinal column with resulting cord transection, seen in legal hangings. |
| Elasticity | Ability to resume original shape and size after being stretched. |
| Force | Physical factor that changes motion of body at rest or already in motion. |
| High velocity | Missiles that compress and accelerate tissue away from the bullet, causing a cavity around the bullet and the entire tract. |
| Inertial resistance | Ability of body to resist movement. |
| Injury | Trauma or damage to some part of the body. |
| Kinematics | Process of looking at an accident and determining what injuries might result. |
| Kinetic energy | Energy that results from motion. |
| Low velocity | Missiles that localize injury to a small radius from center of the tract with little disruptive effect. |
| Muzzle blast | Cloud of hot gas and burning powder at the muzzle of a gun. |
| Shearing | Two oppositely directed parallel forces. |
| Stress | Internal resistance to deformation, or internal force generated from application load. |
| Tensile strength | Amount of tension tissue can withstand and ability to resist stretching forces. |
| Tumbling | Forward rotation around the center; somersault action of the missile can create massive injury. |
| Yaw | Deviation of bullet nose in longitudinal axis from straight line of flight. |
Severity of trauma depends on the wounding agent. There are three major classifications of traumatic disease: blunt injury, penetrating injury, and thermal injury. Energy transfer can result in any one of these individual categories or in any combination of these wounding forces.
Kinematics
Kinematics is the process of looking at an event and determining what injuries are likely to occur given the forces and motion involved. Physics is the foundation on which kinematics is based. Understanding essential laws of physics is the first step toward understanding kinematics.
Newton’s First Law of Motion
Newton’s first law of motion states that a body at rest remains at rest and a body in motion remains in motion unless acted on by an outside force. Pedestrians struck by a vehicle, blast injury patients, and people with gunshot wounds (GSW) are examples of stationary objects set in motion by energy forces. Moving objects interrupted or acted on to stop their motion are illustrated by people falling from a height, vehicles hitting a tree, or vehicles braking to a sudden stop. 14. and 24.
Law of Conservation of Energy
Newton’s Second Law
Newton’s second law states that force equals mass multiplied by acceleration or deceleration. 14
Kinetic Energy
Patient Assessment
Initially trauma patients may not appear seriously injured because of strong compensatory mechanisms that maintain adequate vital signs. All members of a trauma team must anticipate injuries by recognizing potential patterns of injury related to the energy and force of the trauma. Assessment, resuscitation, and stabilization efforts based on this knowledge enable health care providers to evaluate hidden or internal injuries based on these predicted patterns. Health care providers should correlate reported mechanisms to actual or potential injuries. Patients, family, and friends may have reasons to fabricate, falsify, or deny the actual event. Consequently, injuries identified in the examination may not correspond to the reported mechanism. Eliciting a careful history of the injury during initial assessment is vital. Accurate information, especially about MOI, can reduce morbidity and mortality in many circumstances.
When assessing a trauma patient, the emergency nurse should identify mechanisms associated with major force or energy transfer (e.g., pedestrian hit by vehicle traveling faster than 20 mph, falls from more than 20 feet, MVC with major vehicular damage, speed change of more than 20 mph, vehicle rollover, ejected occupant, death of occupant). Some injuries are significant because of potential complications, such as two or more long bone fractures; flail chest; penetrating trauma to the head, neck, chest, abdomen, or groin; and any combination of these patterns with burns over the head, face, or airway. 14. and 22. Patients with significant injuries require close monitoring for complications or changes in hemodynamic stability.
Certain questions elicit valuable information regarding the MOI and are helpful in assessing potential injuries. When a MV is involved, asking the following questions is important:
• What type of vehicle was the patient driving (large or small)?
• What was the estimated speed at the time of the crash?
• Were seat belts or restraint devices used? Were the devices applied appropriately? Were air bags installed, and did they deploy?
• Where was the patient in the vehicle (driver, front passenger, or rear-seat passenger)? If ejected, how far was the patient thrown or found from the vehicle?
• How much damage was done to the vehicle? Where was the majority of damage? Was there intrusion into the passenger space? How much?
• Was there any steering wheel deformity?
If the patient was involved in a fall, the following questions should be asked:
• What was the approximate height of the fall?
• Were any objects struck during the fall?
• What was the surface where the patient landed?
• In what position was the patient found after the fall?
With penetrating injury the following questions should be asked:
Patients with penetrating trauma must be assessed for other types of trauma such as falls or assaults. Patients may be exposed to more than one wounding force.
A detailed history is not always possible and is often impractical. Valuable information can be obtained from family members, prehospital personnel, police, firefighters, bystanders, or eyewitnesses; however, these resources are often overlooked or are unavailable in a hectic emergency department (ED). Management of life-threatening injuries must take priority over obtaining a detailed history; however, every effort should be made to obtain as much historical data as possible.
After airway/cervical spine protection, breathing, circulation, and neurologic function have been assessed and supported, a rapid head-to-toe assessment should be performed. Patients with penetrating trauma are generally easier to assess than those with blunt trauma because injuries are usually focused in one area. Surface trauma may or may not be present with blunt injuries; therefore assessment tends to be more difficult. During the secondary survey, injuries can be found by systematically examining the patient who is completely undressed. Maintaining a high index of suspicion for probable injuries based on certain MOIs and performing a detailed physical assessment will minimize the risk for missed injuries.
Blunt Injury
Blunt trauma is characterized as an injury with no opening in the skin or communication to the outside environment. Definitive diagnosis of blunt trauma is challenging. The extent of injuries is not always obvious; however, these injuries may indeed be life-threatening. Depending on the tissue injured and properties associated with this tissue, certain diagnostic studies are more helpful than others. Air-filled organs, such as lungs and bowel, are subject to blast and compressive injuries. Crush injuries to solid organs (e.g., liver and spleen) may present with minimal external signs of injury, but because energy associated with blunt trauma is transmitted in all directions, organs and tissues can rupture or break if pressure is not released. 14. and 22.
Examples of blunt force events include MVCs, falls, contact sports, and assaults. Direct impact causes the greatest injury. Injuries result when energy is released on impact with the body. Various body tissues respond differently; tissue may move and displace with impact or rupture from the force.
Forces commonly associated with blunt trauma include acceleration, deceleration, shearing, and compression forces. Acceleration injuries occur when velocity (speed) is transferred to a stationary or slower-moving object; deceleration injuries occur when velocity or forward momentum is abruptly stopped. Shearing injuries occur when two oppositely directed parallel forces are applied to tissue. Compression injuries occur with a squeezing inward pressure applied to tissues. An example of these forces is seen with blunt injury to the thoracic aorta. Rapid deceleration causes the aorta to bend and stretch. Shearing damage occurs when stretching forces exceed vessel elasticity. Shearing damage causes the aorta to dissect, rupture, tear, or form an aneurysm. 28
MOTOR VEHICLE COLLISIONS
Before a collision the occupant and vehicle are moving at the same speed. At the time of collision the vehicle and the occupant decelerate to a speed of zero, but at different rates. Deceleration forces are transferred to the body in three points of collision (Figure 20-1). 14. and 22. The first collision occurs when the vehicle strikes another object. As the vehicle stops, the driver or occupant continues to move forward. The second collision occurs when the driver or occupant strikes the steering column, windshield, restraint system, or another structure in the car. The body stops; however, internal organs continue to move until they collide with another organ, cavity wall or structure or they are restrained suddenly by vasculature, muscles, ligaments, or fascia—the third collision point. A fourth collision may occur when unsecured objects in the vehicle collide with the occupant (e.g., unrestrained passengers, bottled drinks, sports equipment). Different damage occurs with each collision; therefore each collision point must be considered separately to avoid missed injuries.
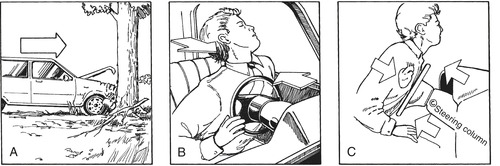 |
| FIGURE 20-1 The three collisions of a motor vehicle collision. A, Auto hits tree. B, Body hits steering wheel, causing broken ribs. C, Heart strikes chest wall, causing blunt cardiac injury. |
One way to estimate injuries in a MVC is to look at the vehicle. Because this is not possible in the ED, the emergency nurse should ask prehospital providers about vehicular damage—interior and exterior. Some prehospital personnel take instant photographs (i.e., digital), allowing hospital providers to see vehicular damage firsthand. The picture can then become a permanent part of the medical record.
Frontal Impact
Frontal impact occurs when the front of a vehicle impacts another object (e.g., another vehicle, tree, bridge abutment). The first collision results in damage to the front end. The more severe the damage and the faster that the vehicle was traveling, the greater the probability for severe injury due to the amount of energy transferred.
Multiple injuries may occur when a person comes to a sudden stop. The use of restraints does reduce the energy absorbed by the body, minimize direct contact with nonyielding interior structures, and prevent ejection from the vehicle. Interior structures, such as the windshield, steering wheel, dashboard, or instrument panel, injure the occupants when direct contact is made. After the vehicle stops, occupants in the front seat continue to move down and under, or up and over, the dashboard.
Down and Under
One path an occupant may travel after a frontal impact is down and under. The occupant continues forward movement downward into the steering column or dashboard. The person’s knees impact the dashboard; however, the upper legs absorb most of the energy. This mechanism may cause patellar dislocations, midshaft femur fractures, and posterior dislocations or fractures of the acetabulum or femoral head (Figure 20-2). When one of these injuries is identified, the patient should be carefully evaluated for the other associated injuries.
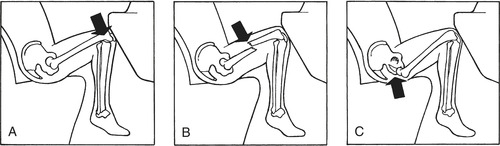 |
| FIGURE 20-2 Down and under pathway. A, Dislocation of the knee. B, Fracture of the femur. C, Dislocation from the acetabulum. |
Up and Over
Continued forward motion from a frontal collision can carry the body up and over, so the head, chest, and/or abdomen strike the steering column, dashboard, or windshield. Head injuries, such as contusions and scalp lacerations, skull fractures, facial fractures, cerebral hemorrhage, or cerebral contusions can occur.
The brain does not stretch easily, so if one part of the brain moves in one direction, the rest follows. The skull stops suddenly after striking the steering wheel, windshield, or another stationary object, but the brain continues to move forward and strikes the inside of the skull. 14. and 22. This area of the brain is compressed and may sustain ecchymosis, edema, or contusion. This type of injury is called a “coup injury,” and it occurs when the damaged area forms directly at the site of contact. As this injury is occurring, the other side of the brain continues to move forward and may be disrupted and shear away from tissue and vascular attachments (Figure 20-3). A contrecoup injury occurs on the side opposite the direct contact because of the movement of the brain within the skull (recoil or “bounce-back”). This impact can cause two separate injuries, shear injury and compression injury, to the same organ, the brain.
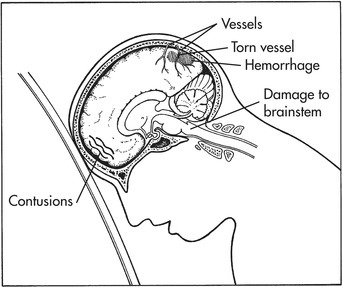 |
| FIGURE 20-3 Brain injury. |
When the head collides with an object, injury to the cervical spine can also occur. The spiderweb effect of a broken windshield suggests the possibility for cervical spine injury. If prehospital providers report a spiderweb effect, caregivers must maintain a high index of suspicion for a spinal injury.
Chest injuries occur when the thorax is compressed against the steering column. Injuries include fractured ribs and sternum, anterior flail chest, blunt cardiac injury, and pulmonary contusion. Thoracic vertebral injuries occur as energy travels up or down the thoracic spine; however, these injuries are less common because the thoracic vertebrae are so well protected.
Compression injuries to the abdomen may result in ruptured hollow organs (e.g., the stomach or intestines) that spill their contents into the abdominal cavity, whereas fractured or lacerated solid organs (e.g., the liver and spleen) are associated with significant blood loss. Organs in the abdominal cavity are attached to the abdominal wall by the mesentery, ligaments, and vasculature. As organs continue their forward motion, attachments can be torn or lacerated.
The steering column is often referred to as a modern-day battering ram and can be the most lethal part of a vehicle. 14. and 22. When steering wheel deformity is reported, the index of suspicion for neck, face, thoracic, or abdominal injuries should increase significantly. Injuries caused by this collision may or may not be readily visible. Lacerations of the chin and mouth, contusion and ecchymosis of the neck, traumatic tattooing of the chest and abdomen, and bruising of the chest and abdomen may be obvious or subtle. Internal occult injuries may be secondary to compression forces, shearing forces, and displacement of kinetic energy. 14. and 22.
Certain organs are more susceptible to shear injuries because of ligamentous attachments (e.g., liver, spleen, bowel, kidneys, and aortic arch). Compression forces commonly injure the lungs, diaphragm, heart, and bladder. Respiratory distress in trauma patients may be caused by injuries such as a pneumothorax, flail chest, and pulmonary contusion. A diaphragmatic hernia or a ruptured diaphragm can also cause respiratory distress and is characterized by bowel sounds in the chest. If a trauma patient has a contused chest wall, a blunt cardiac injury should be considered.
In frontal and lateral impacts a mechanism sometimes called the “paper bag effect” leads to pneumothorax. The driver or occupant sees the collision about to happen, inhales deeply, and holds his or her breath. The glottis closes and seals the lungs. As the chest impacts, the lungs burst like paper bags (Figure 20-4).
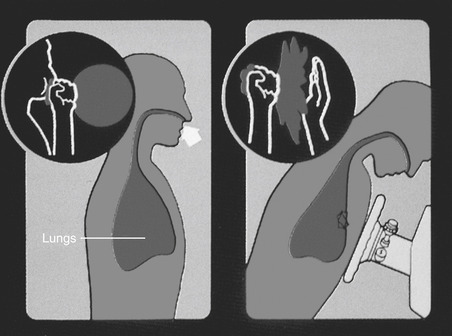 |
| FIGURE 20-4 Compression of lung against closed glottis by impact on anterior or lateral chest wall produces effect like that of compressing a paper bag when opening is closed tightly by hands: the paper bag ruptures, and so does the lung. (From National Association of Emergency Medical Technicians: PHTLS: prehospital trauma life support, ed 6, St. Louis, 2007, Mosby.) |
Frontal impacts are also characterized by extremity injuries. Fractures of the lower extremities, ankles, and feet occur when the occupant extends the feet or are secondary to vehicle intrusion into the passenger compartment. An unrestrained back-seat passenger doubles the risk for injury to front-seat occupants during frontal impact.
Rear Impact
Rear-impact collisions occur when a stationary object or a slower-moving object is struck from behind. Initial impact accelerates the slower-moving or stationary object and may force the vehicle into a frontal collision. When the vehicle suddenly decelerates, hyperextension of the neck may occur, especially when headrests are not properly positioned. Neck ligaments may be strained or torn. If the vehicle strikes another object or is slowed by the driver applying the brake, rapid forward deceleration occurs. The crash then involves two points of impact, rear and frontal, which increases the chance for occupant injuries. Injuries common to each mechanism must be assessed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
