Selected Pregnancy Complications
Early Pregnancy Bleeding
Miscarriage (Spontaneous Abortion)
Miscarriage is a pregnancy that ends as a result of natural causes before 20 weeks of gestation. A fetal weight less than 500 g also may be used to define a miscarriage.
Incidence
Etiology
Early (Before 12 Weeks of Gestation)
Late (Between 12 and 20 Weeks of Gestation)
Types of Miscarriage
Table 2-1 lists types of miscarriage and describes signs and symptoms associated with each type.
TABLE 2-1
Miscarriage: Assessment and Usual Management
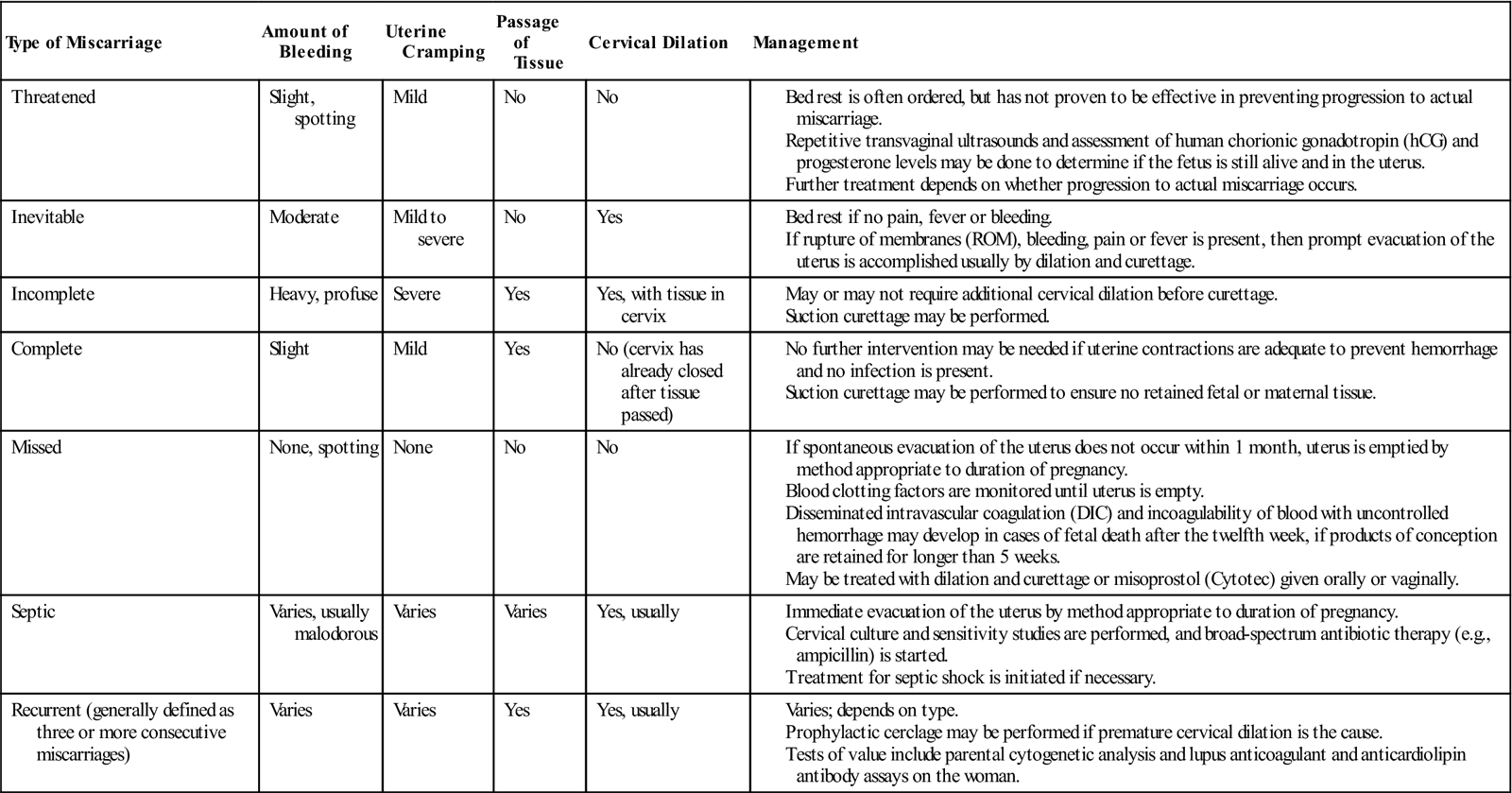
hCG: Human chorionic gonadotropin.
Sources: Cunningham, F., Leveno, K., Bloom, S., Hauth, J., Rouse, D., & Spong, C. (2010), Williams obstetrics (23rd ed.). New York: McGraw-Hill; Gilbert, E. (2011). Manual of high risk pregnancy & delivery (5th ed.). St. Louis: Mosby.
Management
Management depends on the classification of the miscarriage and on signs and symptoms (see Table 2-1).
Postprocedure Care (Applies to Medical and Surgical Management)
 Medications are usually given after the procedure to contract the uterus and control bleeding. See the Medication Guide: Drugs Used to Manage Postpartum Hemorrhage in Appendix B.
Medications are usually given after the procedure to contract the uterus and control bleeding. See the Medication Guide: Drugs Used to Manage Postpartum Hemorrhage in Appendix B.
 Rho(D) immunoglobulin for the Rh-negative woman within 72 hours of miscarriage
Rho(D) immunoglobulin for the Rh-negative woman within 72 hours of miscarriage
 Transfusion therapy for shock or anemia
Transfusion therapy for shock or anemia
 Care of the fetus/products of conception as per hospital and state protocols
Care of the fetus/products of conception as per hospital and state protocols
Ectopic Pregnancy
An ectopic pregnancy is a pregnancy in which the fertilized ovum is implanted outside the uterine cavity. The most common site of implantation is the uterine (fallopian) tube, where approximately 95% of ectopic pregnancies occur. Other much less common implantation sites include the abdominal cavity, ovary, and cervix. Ectopic pregnancy is the leading cause of first-trimester maternal mortality and a leading cause of infertility.
Incidence
The reported incidence of ectopic pregnancy rose through 1990 in the United States. Since then, because more cases are managed medically, reliable data on the actual number of ectopic pregnancies have not been available. Improved diagnostic techniques, however, have likely resulted in the identification of more cases.
Etiology
Signs and Symptoms
 Abdominal pain (occurs in almost every case)
Abdominal pain (occurs in almost every case)
 A period that is delayed 1 to 2 weeks or lighter than usual, or an irregular period
A period that is delayed 1 to 2 weeks or lighter than usual, or an irregular period
 If the ectopic pregnancy ruptures, may see the following:
If the ectopic pregnancy ruptures, may see the following:
 Generalized, one sided, or deep lower quadrant acute abdominal pain
Generalized, one sided, or deep lower quadrant acute abdominal pain
 Signs and symptoms of shock, such as faintness or dizziness
Signs and symptoms of shock, such as faintness or dizziness
Diagnosis
Management
 Surgical management depends on the location and cause of the ectopic pregnancy, the extent of tissue involvement, and the woman’s desires regarding future fertility. Options include:
Surgical management depends on the location and cause of the ectopic pregnancy, the extent of tissue involvement, and the woman’s desires regarding future fertility. Options include:
 General preoperative and postoperative care is appropriate
General preoperative and postoperative care is appropriate
 Ultrasonography is used to confirm an extrauterine pregnancy.
Ultrasonography is used to confirm an extrauterine pregnancy.
 Blood replacement may be necessary.
Blood replacement may be necessary.
 Administer Rho(D) immunoglobulin if appropriate.
Administer Rho(D) immunoglobulin if appropriate.
 Medical management involves giving methotrexate to dissolve the tubal pregnancy. Methotrexate is an antimetabolite and folic acid antagonist that destroys rapidly dividing cells.
Medical management involves giving methotrexate to dissolve the tubal pregnancy. Methotrexate is an antimetabolite and folic acid antagonist that destroys rapidly dividing cells.
 The woman must be hemodynamically stable to be eligible for medical management.
The woman must be hemodynamically stable to be eligible for medical management.
 The woman must also be willing and able to comply with posttreatment monitoring.
The woman must also be willing and able to comply with posttreatment monitoring.
 See Box 2-1 for information regarding administration, patient and family teaching, and follow-up when ectopic pregnancy is treated with methotrexate.
See Box 2-1 for information regarding administration, patient and family teaching, and follow-up when ectopic pregnancy is treated with methotrexate.
Follow-up
β-hCG, Beta-human chorionic gonadotropin.Sources: Gilbert, E. (2011). Manual of high risk pregnancy & delivery (5th ed.). St. Louis: Mosby; Murray, H., Baakdah, H., Bardell, T., & Tulandi, T. (2005). Diagnosis and treatment of ectopic pregnancy. Canadian Medical Association Journal, 173(8), 905-912.
Nursing Considerations
 Encourage expression of feelings related to the pregnancy loss.
Encourage expression of feelings related to the pregnancy loss.
 Refer to community resources for grief or infertility support.
Refer to community resources for grief or infertility support.
 Inform the woman that vaginal intercourse must be avoided until β-hCG levels indicate that the ectopic pregnancy has completely dissolved. This could require abstaining from sexual activity for several months.
Inform the woman that vaginal intercourse must be avoided until β-hCG levels indicate that the ectopic pregnancy has completely dissolved. This could require abstaining from sexual activity for several months.
Late Pregnancy Bleeding
Placenta Previa
Placenta previa is the implantation of the placenta in the lower uterine segment such that it completely or partially covers the cervix or is close enough to the cervix to cause bleeding when the cervix dilates or the lower uterine segment effaces.
Types of Placenta Previa
When transvaginal ultrasound is used placenta previa is classified as:
Risk Factors
Signs and Symptoms
 Painless, bright red vaginal bleeding in the second or third trimester (initially small amount; may stop and recur at any time)
Painless, bright red vaginal bleeding in the second or third trimester (initially small amount; may stop and recur at any time)
 Most cases of placenta previa are diagnosed by ultrasound before bleeding occurs.
Most cases of placenta previa are diagnosed by ultrasound before bleeding occurs.
 Soft, relaxed, nontender uterus with normal tone
Soft, relaxed, nontender uterus with normal tone
 Normal (reassuring) fetal heart rate (FHR) unless a major detachment of the placenta occurs
Normal (reassuring) fetal heart rate (FHR) unless a major detachment of the placenta occurs
 Fundal height often greater than expected for gestational age
Fundal height often greater than expected for gestational age
 Fetal malpresentation common (breech and transverse or oblique lie)
Fetal malpresentation common (breech and transverse or oblique lie)
Risks Associated with Placenta Previa
Maternal
Fetal
Diagnosis
All women with painless vaginal bleeding after 20 weeks of gestation should be assumed to have a placenta previa until proven otherwise.
Management
The woman will be managed either actively or expectantly, depending on gestational age, amount of bleeding, and fetal condition.
Active Management
Cesarean birth is indicated in all women with ultrasound evidence of placenta previa.
Expectant Management
 Purpose is to allow the fetus time to mature
Purpose is to allow the fetus time to mature
 Generally the treatment of choice if:
Generally the treatment of choice if:
 Less than 36 weeks of gestation
Less than 36 weeks of gestation
 FHR tracing is normal (reassuring)
FHR tracing is normal (reassuring)
 Bleeding is mild (<250 ml) and stops
Bleeding is mild (<250 ml) and stops
 Admit to a labor and birth unit for continuous FHR and contraction monitoring.
Admit to a labor and birth unit for continuous FHR and contraction monitoring.
 Initiate large-bore (16- to 18-gauge) IV access.
Initiate large-bore (16- to 18-gauge) IV access.
 Initial laboratory tests: hemoglobin, hematocrit, platelet count, coagulation studies
Initial laboratory tests: hemoglobin, hematocrit, platelet count, coagulation studies
 Maintain a “type and screen” sample at all times in the hospital’s transfusion services department.
Maintain a “type and screen” sample at all times in the hospital’s transfusion services department.
 Administer antenatal corticosteroids if the woman is less than 34 weeks of gestation.
Administer antenatal corticosteroids if the woman is less than 34 weeks of gestation.
 Management after bleeding stops
Management after bleeding stops
 Bed rest with bathroom privileges and limited activity
Bed rest with bathroom privileges and limited activity
 Assess bleeding by checking the amount of bleeding on perineal pads, bed pads, and linens.
Assess bleeding by checking the amount of bleeding on perineal pads, bed pads, and linens.
 Monitor for signs of preterm labor.
Monitor for signs of preterm labor.
 Fetal surveillance: nonstress test (NST) or biophysical profile (BPP) once or twice weekly
Fetal surveillance: nonstress test (NST) or biophysical profile (BPP) once or twice weekly
 No vaginal or rectal examinations
No vaginal or rectal examinations
 Pelvic rest (nothing inserted in the vagina)
Pelvic rest (nothing inserted in the vagina)
 Stable condition with no vaginal bleeding for at least 48 hours before discharge
Stable condition with no vaginal bleeding for at least 48 hours before discharge
 Close supervision by family and friends at home
Close supervision by family and friends at home
 Constant access to transportation
Constant access to transportation
 Able to keep all appointments for fetal testing, laboratory assessments, and prenatal care
Able to keep all appointments for fetal testing, laboratory assessments, and prenatal care
 Discharge teaching for home care
Discharge teaching for home care
 How to assess uterine activity and bleeding
How to assess uterine activity and bleeding
 Pelvic rest and activity limitations
Pelvic rest and activity limitations
Abruptio Placentae (Placental Abruption)
Placental abruption (abruptio placentae) is the detachment of part or all of a normally implanted placenta from the uterus. The separation may be partial, marginal, or complete. Bleeding from the placental site may dissect (separate) the membranes from the decidua basalis and flow out through the vagina (70% to 80%), it may remain concealed (retroplacental hemorrhage) (10% to 20%), or both.
Risk Factors
Signs and Symptoms
See Table 2-2 for assessment of placental abruption.
 Positive Apt test (blood in amniotic fluid)
Positive Apt test (blood in amniotic fluid)
 Decreased hemoglobin and hematocrit levels
Decreased hemoglobin and hematocrit levels
 Decreased coagulation factor levels
Decreased coagulation factor levels
TABLE 2-2
Summary of Findings: Placental Abruption
| Grade 1: Mild Separation (10%-20%) | Grade 2: Moderate Separation (20%-50%) | Grade 3: Severe Separation (>50%) | |
| Bleeding (external, vaginal) | Minimal | Absent to moderate | Absent to moderate |
| Total amount of blood loss | <500 ml | 1000-1500 ml | >1500 ml |
| Color of blood | Dark red | Dark red | Dark red |
| Shock | Rare; none | Mild shock | Common, often sudden, profound |
| Coagulopathy | Rare; none | Occasional DIC | Frequent DIC |
| Uterine tonicity | Normal | Increased, may be localized to one region or diffuse over uterus; uterus fails to relax between contractions | Tetanic, persistent uterine contraction; boardlike uterus |
| Tenderness (pain) | Usually absent | Present | Agonizing, unremitting uterine pain |
| Gestational or chronic hypertension | Usual distribution∗ | Commonly present | Commonly present |
| Fetal effects | Normal fetal heart rate and pattern | Abnormal fetal heart rate and pattern | Abnormal fetal heart rate and pattern; death can occur |
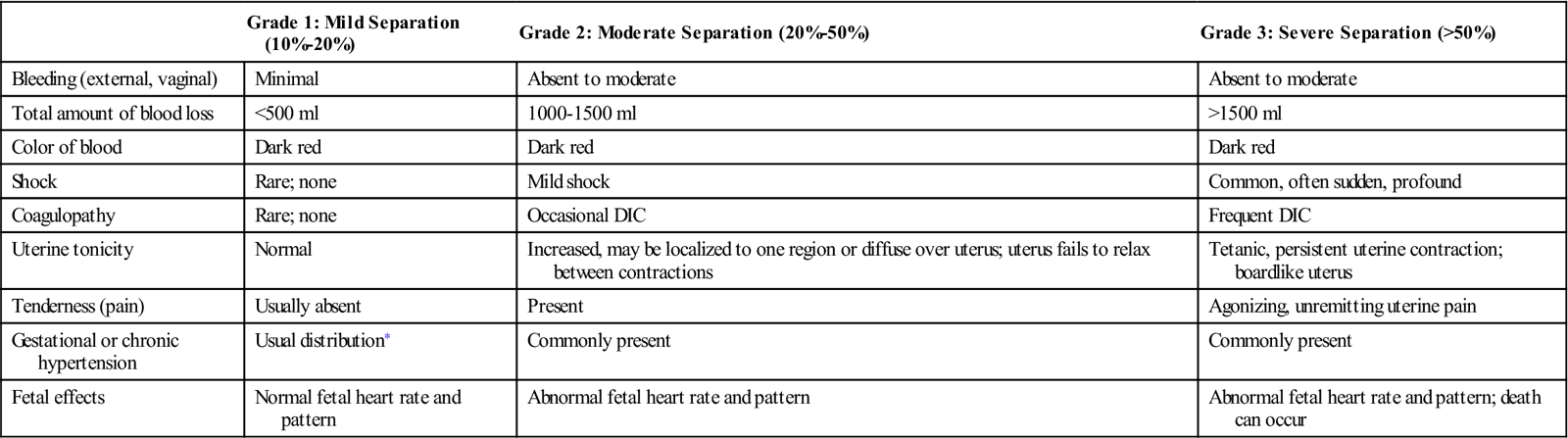
DIC, Disseminated intravascular coagulation.
∗Usual distribution refers to the usual variations of incidence seen when there is no concurrent problem.
Diagnosis
Risks Associated with Placental Abruption
Maternal
Fetal/Neonatal
Management
The woman will be managed either actively or expectantly, depending on the severity of blood loss and fetal maturity and status.
Expectant Management
Active Management
 Treatment of choice in the following situations:
Treatment of choice in the following situations:
 Vaginal birth is usually feasible and especially desirable in cases of fetal death.
Vaginal birth is usually feasible and especially desirable in cases of fetal death.
 Cesarean birth should be reserved for cases of fetal distress or other obstetric indications.
Cesarean birth should be reserved for cases of fetal distress or other obstetric indications.
 At least one large-bore (16- to 18-gauge) IV line
At least one large-bore (16- to 18-gauge) IV line
 Serial lab tests to monitor hemoglobin, hematocrit, and clotting status
Serial lab tests to monitor hemoglobin, hematocrit, and clotting status
 Continuous electronic fetal monitoring
Continuous electronic fetal monitoring
 Blood and fluid volume replacement
Blood and fluid volume replacement
 Educate woman and family on cause, treatment, and expected outcomes.
Educate woman and family on cause, treatment, and expected outcomes.
Endocrine and Metabolic Disorders
Pregestational Diabetes Mellitus
Diabetes mellitus refers to a group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both. There are four types of diabetes mellitus: type 1, type 2, other specific types (e.g., diabetes caused by genetic defects in B-cell function or insulin action, disease or injury of the pancreas, or drug-induced diabetes), and gestational diabetes. Type 1 or type 2 diabetes that existed before pregnancy is often referred to as pregestational diabetes. Of the women with pregestational diabetes, the majority (65%) have type 2 diabetes.
Etiology
Type 1 Diabetes
Type 2 Diabetes
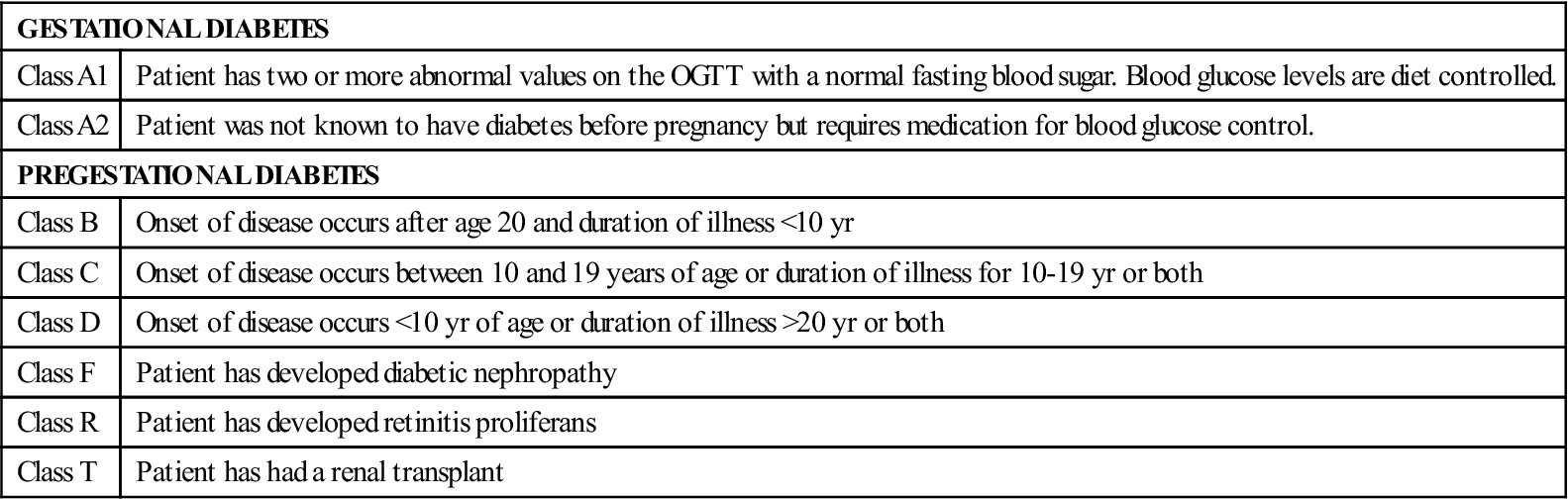
White’s Classification System for Diabetes in Pregnancy
 Developed by Dr. Priscilla White, a physician who worked with pregnant women with diabetes during the 1940s (Table 2-3)
Developed by Dr. Priscilla White, a physician who worked with pregnant women with diabetes during the 1940s (Table 2-3)
 Based on age at diagnosis, duration of illness, and presence of vascular disease
Based on age at diagnosis, duration of illness, and presence of vascular disease
 Has been modified through the years but is still frequently used to assess maternal and fetal risk
Has been modified through the years but is still frequently used to assess maternal and fetal risk
TABLE 2-3
White’s Classification of Diabetes in Pregnancy (Modified)
| GESTATIONAL DIABETES | |
| Class A1 | Patient has two or more abnormal values on the OGTT with a normal fasting blood sugar. Blood glucose levels are diet controlled. |
| Class A2 | Patient was not known to have diabetes before pregnancy but requires medication for blood glucose control. |
| PREGESTATIONAL DIABETES | |
| Class B | Onset of disease occurs after age 20 and duration of illness <10 yr |
| Class C | Onset of disease occurs between 10 and 19 years of age or duration of illness for 10-19 yr or both |
| Class D | Onset of disease occurs <10 yr of age or duration of illness >20 yr or both |
| Class F | Patient has developed diabetic nephropathy |
| Class R | Patient has developed retinitis proliferans |
| Class T | Patient has had a renal transplant |
OGTT, Oral glucose tolerance test.
Sources: Landon, M., Catalano, P., & Gabbe, S. (2007). Diabetes mellitus complicating pregnancy. In S. Gabbe, J. Niebyl, & J. Simpson (Eds.), Obstetrics: Normal and problem pregnancies (5th ed.). Philadelphia: Churchill Livingstone; Moore, T., & Catalano, P. (2009). Diabetes in pregnancy. In R. Creasy, R. Resnik, J. Iams, C. Lockwood, & T. Moore (Eds.), Creasy and Resnik’s maternal-fetal medicine: Principles and practice (6th ed.). Philadelphia: Saunders.
Risks Associated with Pregestational Diabetes
Risks increase with the duration and severity of the diabetic condition. Also pregnancy may contribute to the vascular changes associated with diabetes.
Maternal
Fetal/Neonatal
Management
Medical goal of care: Achieving and maintaining constant euglycemia through a combination of diet, insulin, and exercise. The key to an optimal pregnancy outcome is strict maternal glucose control before conception as well as throughout pregnancy. See Table 2-4 for desired blood glucose levels during pregnancy.
TABLE 2-4
Target Blood Glucose Levels during Pregnancy
| Time of Day | Target Plasma Glucose Level (mg/dl) |
| Premeal or fasting | >65 but <95 |
| Postmeal (1 hr) | <130-140 |
| Postmeal (2 hr) | <120 |
Sources: Landon, M., Catalano, P., & Gabbe, S. (2007). Diabetes mellitus complicating pregnancy. In S. Gabbe, J. Niebyl, & J. Simpson (Eds.), Obstetrics: Normal and problem pregnancies (5th ed.). Philadelphia: Churchill Livingstone; Moore, T., & Catalano, P. (2009). Diabetes in pregnancy. In R. Creasy, R. Resnik, J. Iams, C. Lockwood, & T. Moore (Eds.), Creasy and Resnik’s maternal-fetal medicine: Principles and practice (6th ed.). Philadelphia: Saunders.
Pregnancy
 Perform routine prenatal examination.
Perform routine prenatal examination.
 Determine effects of diabetes on pregnancy:
Determine effects of diabetes on pregnancy:
 Perform a baseline electrocardiogram to assess cardiovascular status.
Perform a baseline electrocardiogram to assess cardiovascular status.
 Glycosylated hemoglobin (hemoglobin A1c) (should be ≤6%)
Glycosylated hemoglobin (hemoglobin A1c) (should be ≤6%)
 24-hour urine collection for total protein and creatinine clearance
24-hour urine collection for total protein and creatinine clearance
 Urinalysis and culture: initial prenatal visit and throughout the pregnancy
Urinalysis and culture: initial prenatal visit and throughout the pregnancy
 Ideally, 55% of total calories should be carbohydrates.
Ideally, 55% of total calories should be carbohydrates.
 Large bedtime snack (at least 25 g of carbohydrate with some protein) is recommended.
Large bedtime snack (at least 25 g of carbohydrate with some protein) is recommended.
 Must be prescribed by the health care provider
Must be prescribed by the health care provider
 Best time for exercise is after meals.
Best time for exercise is after meals.
 Several types of insulin preparations are available. They differ in onset, peak, and duration of action. See Table 2-5 for further information on common insulin preparations.
Several types of insulin preparations are available. They differ in onset, peak, and duration of action. See Table 2-5 for further information on common insulin preparations.
 Done several times each day, using a glucose reflectance meter or biosensor monitor
Done several times each day, using a glucose reflectance meter or biosensor monitor
 Now considered standard of care for monitoring blood glucose levels during pregnancy
Now considered standard of care for monitoring blood glucose levels during pregnancy
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree











































































































































































































