Chapter 2 Hypertensive disorders
RELEVANT ANATOMY AND PHYSIOLOGY
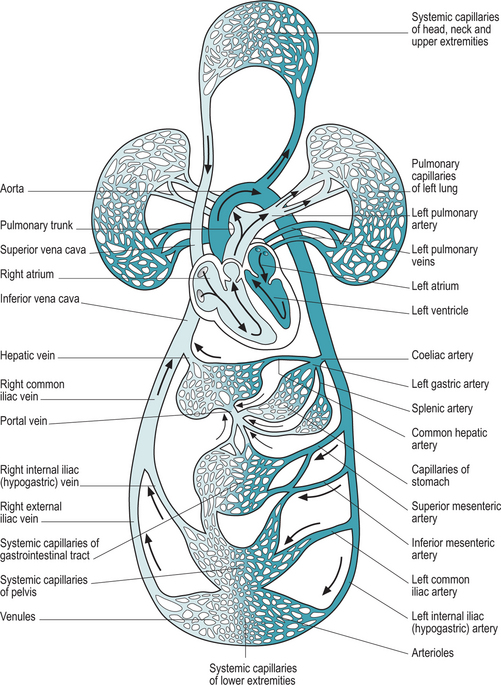
Blood pressure is the force that drives the cardiovascular system. It is the result of the contraction of the heart on blood, forcing it through the blood vessels. The anatomy of the cardiovascular system is shown in Figure 2.1.
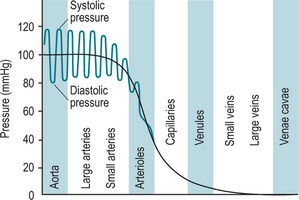
The heart is composed of four chambers separated into a right and left side by a continuous septum. The right atrium receives deoxygenated blood from the body and directs the blood into the right ventricle where it is pumped out by a muscular contraction of the ventricular wall to the lungs. Here the blood is oxygenated and carbon dioxide is removed. The blood then leaves the respiratory system and is returned to the left atrium where it is passed down to the highly muscular left ventricle. The heart contracts and the blood is moved forcibly out into the largest artery in the body, the aorta, and directed to all parts of the body to transport oxygen, along with other chemicals, to body cells. The pressure of the expulsion of blood from the ventricles on the walls of the blood vessels is the force known as blood pressure. Blood then moves through the circulatory system from the initial area of high pressure to areas of decreasing pressure as shown in Figure 2.2.
Blood pressure is dependent on two factors:
Viscosity is the ‘thickness’ of the blood, i.e. the ratio of blood cells and other solids such as proteins to the fluid part of blood – plasma. In conditions such as dehydration, the blood contains a high proportion of solids, and is less easy to move along the blood vessels. Resistance, due to friction along the vessel walls, will be increased. Where solids such as red blood cells are decreased, resistance is also decreased.
Control of blood pressure
Hormonal regulation
Several hormones are involved in the regulation of blood pressure:
HYPERTENSION IN THE GENERAL POPULATION
It is thought that at least 18% of the UK population suffers from hypertension; the majority, at least 95%, of unknown cause (Beevers et al 2001). Hypertension is present in 1–6% of women of childbearing age (Magee 2001). Hypertension has been termed the ‘silent killer’ because the sufferer commonly has no symptoms and is only diagnosed through screening or when the disease manifests itself in a complication of the disorder. Hypertension is present in up to 10% of all pregnancies either as a pre-existing disease (5–15% of the total) or as a disorder specific to pregnancy, pre-eclampsia (Lloyd 2003). Diagnosing and treating the hypertensive diseases of pregnancy is very challenging and may involve a balancing act between the health of the mother and the maturity of the fetus.
Pathophysiology of hypertension
Essential hypertension
Although the exact cause of essential hypertension is not known, it is probable that many interrelated factors contribute to increased blood pressure. Normal blood pressure is dependent on a balance between cardiac output and peripheral resistance as described above. Most people with essential hypertension have a normal cardiac output but a raised peripheral resistance. The reason for this is unclear. Factors that may contribute to this may include a familial tendency, diet, obesity, insulin resistance, fetal development and neurovascular anomalies (Beevers et al 2001). Whatever the cause, the result is an inappropriate decrease in the diameter of the arterioles resulting in increased peripheral resistance. As a result, cardiac rate and/or stroke volume increases to produce a blood pressure sufficient to overcome this resistance and get sufficient blood with gases and nutrients to the cells of the body to enable metabolism to take place.
Secondary hypertension
Secondary hypertension is the result of an identifiable abnormality which causes increased peripheral resistance (Gutierrez & Petersen 2002). For example, renal disease may result in decreased renal perfusion stimulating the kidneys to release increased amounts of renin; an adrenal tumour or hyperthyroidism will stimulate increased amounts of catecholamines. Inappropriately increased levels of renin or catecholamines will cause vasoconstriction and thus increase peripheral resistance. Cardiac output will increase in order to raise blood pressure sufficiently to get sufficient gases and nutrients to all the cells of the body.
Diagnosis
Diagnosis of hypertension is made when resting blood pressures >140 mmHg systolic and/or 90 mmHg diastolic are observed (Box 2.2).
Lifestyle changes
Drug therapy
HYPERTENSION IN PREGNANCY AND CHILDBIRTH
Overview
Hypertensive disorders occur in up to 10% of all pregnancies and contribute significantly to both maternal and fetal mortality and morbidity rates (Lloyd 2003). Caring for the pregnant women with hypertension is a considerable challenge for the multidisciplinary team. As in the general population, there are seldom any signs or symptoms of hypertension and as the midwife is the primary care giver in the majority of pregnancies, she must be alert for this condition. Screening early in pregnancy will identify women with pre-existing hypertension. Ongoing examination throughout pregnancy will identify women developing pregnancy-induced hypertension or pre-eclampsia. However, hypertension may be a late sign of pre-eclampsia and thus the health of both mother and fetus may be compromised before the condition is detected.
Relevant physiological changes in the cardiovascular system in pregnancy
During pregnancy, the cardiovascular system must meet the increasing demands of both the pregnant woman and the growing fetus. In the heart, cardiac output will increase by up to 40% during the first and second trimesters of pregnancy (Murray 2003). Both stroke volume and heart rate will contribute to this. The raised cardiac output enables blood to flow through the added circulation formed in the enlarging uterus and placental bed, and also to meet the extra needs of other organs of the mother’s body.
Blood vessels increase in number and length to supply the placenta. Vasodilation occurs as a result of the action of the hormone progesterone on the smooth muscle of the vessel walls. Plasma volume increases by up to 50% and the number of blood cells by up to 18% during pregnancy to compensate for the apparent loss in blood volume resulting from the presence of extra blood vessels and vasodilation (Blackburn 2002). A resultant lowering of blood pressure in mid-pregnancy may contribute to feelings of lightheadedness and fatigue in the mother. The disproportionate increase in plasma volume over the number of blood cells and proteins present in circulating blood may result in the loss of fluid to the interstitial fluid compartment in the capillary bed, giving rise to generalized oedema in many pregnant women.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree