Section 2. Autonomic nervous system
2.1 Autonomic nervous system – overview 58
2.2 Adrenergic pharmacology 59
2.3 Cholinergic pharmacology 74
2.1. Autonomic nervous system – overview
The ANS regulates:
▪ contraction and relaxation of smooth muscle
▪ all exocrine and some endocrine glandular secretions
▪ the heart beat
▪ some steps in metabolism.
The ANS has two main branches:
▪ The sympathetic nervous system (SNS).
▪ The parasympathetic nervous system (PSNS).
Nervous transmission is electrical but at synapses transmission is chemically mediated by substances called neurotransmitters.
▪ The SNS is stimulated in conditions of fight and flight and uses the neurotransmitter noradrenaline( NA; norepinephrine). Fibres that release NA are termed adrenergic.
▪ The PSNS functions in relatively peaceful conditions such as when resting and digesting. It uses the neurotransmitter acetylcholine( ACh). ACh-releasing fibres are termed cholinergic.
Both branches of the ANS generally serve the same internal organs but produce opposite effects. If one division stimulates certain muscles to contract or a gland to secrete, the other division usually inhibits that action.
Sweat glands and most of the blood vessels have only sympathetic innervation.
The motor unit of the ANS is a two-neurone chain. There is a preganglionic neurone with its cell body in the brain or spinal cord. The axon from this neurone synapses with a postganglionic motor neurone in a ganglion outside the central nervous system (CNS). The postganglionic axon from this neurone extends to the effector organ.
Neurotransmitters released by the ANS:
▪ All preganglionic fibres are cholinergic (release ACh).
▪ All postganglionic parasympathetic fibres are cholinergic at their effectors.
▪ Sympathetic postganglionic fibres release NA but those innervating the sweat glands of the skin, some blood vessels and the external genitalia release ACh.
▪ The adrenal medulla releases adrenaline (epinephrine) (85%) and NA (15%).
ACh and NA may be excitatory or inhibitory, depending on the type of transmitter on the target organ.
Drug action in the ANS may involve:
▪ agonists or antagonists at adrenergic or cholinergic receptors
▪ release, storage or synthesis of neurotransmitters
▪ re-uptake pumps or enzymes inactivating neurotransmitters.
2.2. Adrenergic pharmacology
A basic plan of the autonomic nervous system is shown in Figure 2.1 and a comparison of transmission in the somatic and autonomic nervous systems is shown in Figure 2.2.
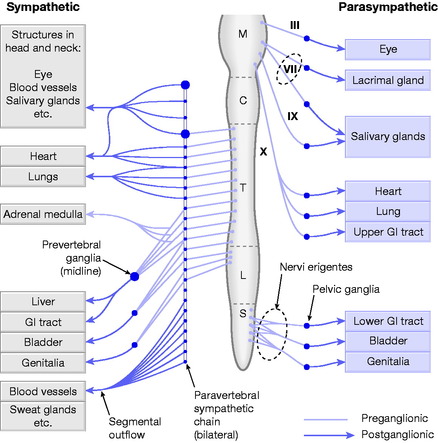 |
| Fig. 2.1 Basic plan of the autonomic nervous system. C = Cervical; GI = Gastrointestinal; L = Lumbar; M = Medullary; S = Sacral; T = Thoracic. Reproduced with permission from Rang & Dale’s Pharmacology, 6th edn, by H P Rang, M M Dale, J M Ritter et al, 2007, Churchill Livingstone, Edinburgh. |
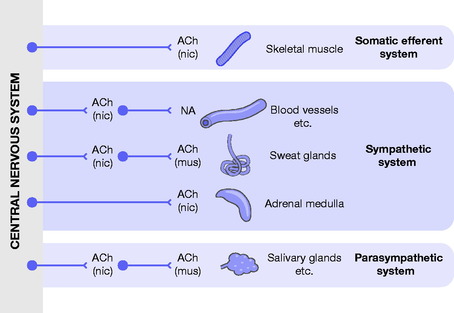 |
| Fig. 2.2 Transmission in the autonomic and somatic nervous systems. The main two types of acetylcholine (ACh) receptor, nicotinic acid (nic) and muscarinic (mus) are indicated. NA = noradrenaline (norepinephrine). Reproduced with permission from Rang & Dale’s Pharmacology, 6th edn, by H P Rang, M M Dale, J M Ritter et al, 2007, Churchill Livingstone, Edinburgh. |
The effects of SNS stimulation
These effects are many and varied and will affect the whole body. You have to think of yourself when you are very frightened or nervous – before an exam or interview for example – to imagine what these effects are. Some effects of stimulation of the SNS and the PSNS are shown in Table 2.1. Anatomical differences are shown in Table 2.2.
| Target organ/system | Parasympathetic effects | Sympathetic effects |
|---|---|---|
| Eye (iris) | Constricts pupil | Dilates pupil |
| Lens of eye | Accommodation | Slight relaxation of ciliary muscle |
| Glands (nasal, lacrimal, salivary, gastric, pancreatic) | Mostly stimulates secretory activity | Mostly inhibits secretory activity |
| Sweat glands | No effect | Stimulates sweating (but via acetylcholine and muscarinic receptor) |
| Adrenal medulla | No effect | Stimulates secretion of adrenaline (epinephrine) and noradrenaline (norepinephrine) |
| Arrector pili muscles attached to hair follicles | No effect | Stimulates contraction – hairs stand on end and goose pimples occur |
| Heart | Decreases rate | Increases rate |
| Decreases force | Increases force | |
| Atrioventricular node | Decreases speed of conduction | Increases automaticity |
| Bladder | Causes contraction of smooth muscle in the bladder wall, relaxes the urethral sphincter and promotes voiding | Causes relaxation of smooth muscle of bladder wall; constricts urethral sphincter and inhibits voiding |
| Lungs | Constricts the bronchioles | Dilates bronchioles and mildly constricts blood vessels |
| Digestive tract | Increases peristalsis and secretion by digestive organs. Relaxes sphincters and allows movement of food along tract | Decreases activity of glands and muscles of digestive tract Constricts sphincters |
| Liver | No effect | Stimulates the release of glucose into the bloodstream |
| Gall bladder | Causes contraction and release of bile | Relaxation and no release of bile |
| Kidney | No effect | Causes vasoconstriction; decreases urine output Promotes renin secretion |
| Blood vessels | Little or no effect | Constricts most blood vessels and increases blood pressure Constricts vessels in skin and abdominal viscera to divert blood to the muscles, brain and heart Dilates vessels of skeletal muscle during exercise |
| Blood coagulation | No effect | Increases coagulation |
| Cellular metabolism | No effect | Increases metabolic rate |
| Adipose tissue | No effect | Stimulates fat breakdown |
| Mental activity | No effect | Increases alertness |
| Penis | Causes erection | Causes ejaculation |
| PSNS | SNS |
|---|---|
| Fibres emerge from the brain (cranial nerves III, VII, IX, X) and sacral spinal cord (S2–S4) | Fibres emerge from thoracolumbar region of SC (3 cervical, 11 thoracic, 4 sacral and 1 coccygeal) |
| Long preganglionic fibres | Short preganglionic fibres |
| Short postganglionic fibres | Long postganglionic fibres |
| Ganglia in effector organs | Ganglia close to spinal cord |
The body is being prepared for an emergency where it may have to exert much physical activity and all the results of SNS stimulation are towards these ends.
The heart
▪ An increase in heart rate (positive chronotropic effect).
▪ An increase in the force of contraction (positive inotropic effect).
The respiratory system
▪ Increase in the rate and depth of breathing.
▪ Dilates the bronchioles.
The circulation
▪ Dilation of blood vessels where a good blood supply is needed – the coronary vessels, skeletal muscle and the lungs.
▪ Increase in blood pressure.
The gastrointestinal tract
▪ A decrease in motility.
▪ A reduction in secretion of enzymes.
The liver
▪ An increase in gluconeogenesis (manufacture of new glucose).
▪ Blood glucose levels increased and may result in glycosuria in severe stress.
The kidney
▪ Renin secretion leads to an increase in blood pressure.
▪ Vasoconstriction reduces urinary output.
The skin
▪ Increased sweating.
▪ Piloerection – goose pimples.
The eye
▪ Dilation of the pupil.
Skeletal muscle
▪ Toned up.
▪ This may be overdone, so that when nervous a tremor results.
Adrenal gland
▪ Stimulates secretion of adrenaline (epinephrine) and noradrenaline (norepinephrine).
Bladder
▪ Contracts the urethral sphincter and inhibits voiding.
Other effects
▪ Increased blood coagulation.
▪ Stimulates lipolysis (fat breakdown).
▪ Increased alertness.
It is the neurotransmitter noradrenaline( NA) that is having all these sympathetic effects on the body.
Body cells have receptors for NA and when the NA fits into the receptor the cell is turned on and the sympathetic effects above are produced.
The NA fits the receptor like a key fits a lock. The molecule is just the right shape to fit.
Noradrenaline storage
Mostly stored in vesicles in nerve endings. Release occurs when a nervous impulse arrives at the synapse.
Degradation of noradrenaline
This is not by an enzyme in the synapse but by uptake into the cells and degradation by an enzyme in the neuronal mitochondria called monoamine oxidase( MAO). Circulating NA is destroyed by the enzyme catechol- O-methyltransferase (COMT).
The adrenergic receptor
▪ There are two major classes of adrenergic receptor on cell membranes – alpha-adrenergic receptors and beta-adrenergic receptors.
▪ Organs that respond to adrenaline (epinephrine) display one or both types of receptor.
There are subtypes of each receptor – α 1 and α 2, β 1, β 2 and β 3. The effects of stimulation of these different receptor subtypes are shown in Table 2.3 on pages 75–77.
▪ α 1 Receptors are found on blood vessels where stimulation causes vasoconstriction, an increase in total peripheral resistance and an increase in blood pressure. NA is most potent at the α 1 receptor.
▪ The distinction between β 1 and β 2 receptors is an important one as β 1 receptors are found mostly in the heart where they are excitatory and are responsible for the positive chronotropic (increased rate) and positive inotropic (increased force) effects of catecholamines. β 1 Receptors have approximately equal affinity for adrenaline (epinephrine) and NA.
▪ β 2 Receptors are responsible for smooth muscle relaxation in many organs e.g. bronchiolar relaxation in the respiratory tract and vasodilation in skeletal vascular beds. β 2 Receptors have a higher affinity for adrenaline (epinephrine) than NA.
Most organs have a predominance of one type of receptor. Blood vessels in skeletal muscle have both α 1 and β 2 receptors but the latter predominate. Some organs may have one type of receptor almost exclusively – for example, the heart predominantly has β 1 receptors.
The importance of the autonomic nervous system in the control of such a wide range of the body’s vital functions has led to the development of many pharmacological agents, both naturally occurring and synthetic, that may modulate its action.
Catecholamines
You may hear adrenaline (epinephrine) and NA referred to as catecholamines. This is a term used for chemical compounds derived from the amino acid tyrosine and containing catechol and amine groups. The most abundant catecholamines are adrenaline (epinephrine), NA and dopamine.
Receptor selectivity
Receptor subtypes within the SNS producing specific effects has allowed the development of both agonists to stimulate, and antagonists to block, these effects. Some of the drugs developed show selectivity for certain subtypes of receptor.
 Beta 2 agonists such as salbutamol are important as bronchodilators.
Beta 2 agonists such as salbutamol are important as bronchodilators.Cardioselective beta blockers are important in ischaemic heart disease.
Adrenaline (epinephrine) acts on all adrenergic receptors and so increases heart rate and force while also causing brochodilation. It can cause peripheral vasoconstriction (alpha receptor) or vasodilation (β 2 receptor). Adrenaline (epinephrine) is discussed in more detail later.
Adrenergic agonists
Adrenaline (epinephrine) and NA are relatively nonselective. Other drugs have been developed for their ability to be more potent at one type of receptor.
Alpha receptors
There are two main types of alpha receptor, α 1 and α 2.
α 1 Receptors
α 1 Stimulation produces:
Contraction of all types of smooth muscle except the gastrointestinal tract. This affects vascular smooth muscle and includes the large arteries and veins as well as the small ones.
This results in:
▪ reduced vascular compliance
▪ increased central venous pressure
▪ increased peripheral resistance
▪ all leading to an increase in systolic and diastolic blood pressure.
Some vascular beds e.g. cerebral, coronary and pulmonary are little affected.
Baroreceptor reflexes are activated by the increased arterial pressure and this may cause a reflex bradycardia.
▪ Dilation of the pupil.
▪ Contraction of the gastrointestinal sphincters and decreased peristalsis resulting in a slowing of digestion.
▪ Contraction of the external sphincter and relaxation of the detrusor muscle in the bladder leading to retention of urine.
▪ Increased blood sugar levels.
▪ Contraction of the piloerector muscles resulting in ‘goose flesh’.
Phenylephrine stimulates the α 1 receptor and is valuable to raise blood pressure in hypotension and circulatory shock. NA (see below) may be used for its alpha agonist properties.
α 1 Stimulation of the nasal blood vessels will cause vasoconstriction and so decongestion. Ephedrine nasal drops may be used but rebound congestion may occur when the drug is stopped.
α 2 Receptors
Not as important clinically. Stimulation of the α 2 receptor causes inhibition of transmitter release (including NA and ACh from autonomic nerves).
A drug such as clonidine that stimulates the receptor leads to a decrease in blood pressure. It may also be used to treat hot flushes in the menopause and migraine.
Beta receptors
There are two main subtypes of beta receptor, β 1 and β 2. There is also a β 3 receptor that is not important clinically.
β 1 Receptors
Located on the myocardium, adipocytes (fat cells), sphincters and smooth muscle of the gastrointestinal tract and renal arterioles.
β 1 Stimulation results in:
▪ Increased rate and force of the heartbeat i.e. positive inotropic and chronotropic effect. This is the result of an increased influx of calcium into cardiac fibres. Stronger cardiac contractions lead to a more complete ventricular emptying and an increase in cardiac work and oxygen consumption. Overall cardiac efficiency is reduced.
▪ The increased cardiac output may lead to a rise in systolic blood pressure.
▪ Increased lipolysis in adipose tissue leading to increased blood lipids.
▪ Decreased digestion and intestinal motility.
▪ Release of renin into the renal blood, resulting in the formation of angiotensin II. This is a powerful vasoconstrictor.
Clinical applications
As positive inotropes in:
▪ Circulatory and cardiogenic shock – dopamine and dobutamine are cardiac stimulants and act on β 1 receptors in cardiac muscle. They increase the contractility of the heart with little effect on the rate.
▪ Cardiac arrest – adrenaline (epinephrine).
β 2 Receptors
Located on the smooth muscle of the bronchioles, skeletal muscle, mast cells, the uterus and in liver cells.
β 2 Stimulation leads to relaxation of most kinds of smooth muscle.
▪ Within the respiratory tract producing bronchodilation.
▪ In the vascular system vasodilation is particularly marked in skeletal muscle.
▪ Relaxation of uterine smooth muscle.
▪ Powerful inhibition of gastrointestinal tract smooth muscle contraction is produced by both α and β receptors.
Clinical applications
▪ Asthma and chronic airflow limitation as in chronic obstructive pulmonary disease – salbutamol is a β 2 agonist.
▪ Relaxation of the uterus in preterm labour – ritodrine.
Adrenaline (epinephrine)
For medical use adrenaline (epinephrine) is prepared synthetically. It is not effective orally as it is destroyed by the acid in the stomach.
Clinical effects
▪ Increased cardiac output.
▪ Rise in systolic blood pressure due to the increased output of blood from the heart.
▪ Low doses may decrease the total peripheral vascular resistance and so decrease blood pressure.
▪ The diastolic blood pressure shows little change as adrenaline (epinephrine) produces an increase in the force and rate of the heartbeat (β 1 effect).
▪ Vasoconstriction only in the skin and in the splanchnic area (mixed α and β 2 effects) and vasodilation in arteries in muscle (β 2 effect).
▪ Renal artery constriction is greater with adrenaline (epinephrine) than NA.
▪ Relaxation of smooth muscle, including powerful bronchodilation. Relieves all known allergic and histamine-induced bronchoconstriction.
▪ Stabilisation of the mast cell.
▪ Rise in blood glucose due to mobilisation of glucose from the tissues, increased release of glucagon and decreased release of insulin.
Clinical applications
▪ Cardiac arrest.
▪ Anaphylaxis.
▪ Acute severe asthma.
▪ Some specialist local anaesthetics may contain 1:100 000 parts of adrenaline (epinephrine) to enable them to remain longer at the site of injection.
Route of administration
Adrenaline (epinephrine) cannot be administered orally as it is destroyed in the stomach.
Anaphylaxis – by intramuscular injection. Adrenaline 1:1000, 0.5 ml (500 micrograms) is given by emergency practitioners to an adult. A self-administered EpiPen® has 300 micrograms of adrenaline (epinephrine). The dose may be repeated in 5 minutes depending on response.
In a cardiac arrest situation adrenaline 1:10 000 (100 micrograms per ml) is used. A dose of 10 ml is usually given by a central line.
Side effects
Include anxiety, tremor, tachycardia, arrhythmias, hypertension, pulmonary oedema, nausea, vomiting, sweating and dizziness.
Noradrenaline (norepinephrine)
Its most important action is to produce widespread vasoconstriction and thus a rise in systolic and diastolic blood pressure (alpha effect).
Clinical applications
Used in the treatment of various kinds of shock associated with a very low blood pressure.
Although a satisfying rise in blood pressure can be obtained by vasoconstriction, this reduces the blood flow to certain organs, particularly the kidneys.
 Both adrenaline (epinephrine) and NA may produce a spontaneous firing of the Purkinje fibres, causing them to exhibit pacemaker activity and resulting in ventricular extrasystoles which increase the susceptibility of the ventricular muscle to fibrillation.
Both adrenaline (epinephrine) and NA may produce a spontaneous firing of the Purkinje fibres, causing them to exhibit pacemaker activity and resulting in ventricular extrasystoles which increase the susceptibility of the ventricular muscle to fibrillation.These effects are more likely with adrenaline (epinephrine) than NA.
Adrenoreceptor antagonists
These drugs block the action of the natural ligand – NA – in the SNS. Most are selective for the alpha or beta receptor.
Alpha-adrenoreceptor antagonists
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
