CHAPTER 19. Management of the Critical Care Patient in the Emergency Department
Carol Rhoades, Reneé Semonin Holleran, Lori Carpenter and Colin Grissom
CRITICAL CARE IN THE EMERGENCY DEPARTMENT
Critical care patients remaining for extended periods of time in the emergency department (ED) have become increasingly more common over the past decades. 26 Multiple reasons for “boarding” of critical care patients in the ED have been identified. Some of these are a lack of inpatient critical care beds, the ongoing nursing shortage, and increasing ED visits despite a decrease in EDs. Ultimately, when hospital beds are full, patients cannot be transferred from the critical care units to floor beds, which results in critical care patients boarding in the ED. Other reasons that account for the increase in boarding of critical care patients in the ED are a lack of policies and procedures to facilitate patient movement from the ED to a critical care unit, lack of administrative support to improve patient flow, and lack of regionalization of health care resources to admit patients. 13
Inpatient care of the critically ill or injured patient results in different needs than the typical initial stabilization provided in the ED. Additional education, equipment, and resources are needed to ensure safe and competent critical care. Two recent studies demonstrated that hospital mortality rates increased as the length of time waiting for an inpatient critical care bed increased once an admission order to a critical care unit was received. 12. and 14.
Management of the critically ill or injured patient necessitates that the ED have skilled critical care clinicians and equipment and an area where patients can be closely monitored. Many EDs are not designed to provide this type of care and do not have the appropriate equipment for invasive monitoring. Observation units have been created in EDs to alleviate some of the pressure related to limited inpatient beds. However, there are times when these units and other areas of the ED may be used to manage critical care patients. There are many unpredictable critical conditions that can occur in patients admitted to an ED observation unit, including dyspnea, shock, cardiac arrest, and death. The focus of this chapter is to discuss the common clinical conditions and interventions needed when emergency nurses care for the critically ill or injured patient boarding in the ED. Included in this chapter is the management of the artificially ventilated patient, selected invasive lines, and sepsis.
MECHANICAL VENTILATION
Mechanical ventilation of a critically ill or injured patient can be challenging in the ED. Ventilator settings, alarms, patient positioning, and oral care are just a few of the issues that need to be addressed.
Indications for Intubation and Mechanical Ventilation
Intubation is indicated in a variety of clinical situations but generally falls into one of three main categories: failure to maintain a patent airway, inadequate oxygenation, or ineffective ventilation.
Failure, or Anticipated Failure, to Protect or Maintain a Patent Airway
The following groups of patients are at a higher risk for airway issues:
• Obtunded or comatose patients with loss of gag reflex: traumatic brain injury (TBI), overdose, anoxia, cerebral vascular accident, cerebral aneurysm, etc.
• Patients with a partial or complete obstruction: edema due to inhalation injury, neck trauma, epiglottitis, laryngeal edema, bronchospasm, foreign object aspiration, burns
• Patients receiving some pharmacologic therapy: benzodiazepine therapy for status epilepticus, sedation/paralysis for TBI to control increased intracranial pressures or to obtain diagnostic imaging in combative patients
Inadequate Oxygenation
A shunt occurs when alveoli are perfused but not ventilated, as in pneumonia, acute respiratory distress syndrome (ARDS), acute lung injury (ALI), pulmonary hemorrhage or pulmonary contusion, and atelectasis. Dead space ventilation results when alveoli are ventilated but not perfused, as in pulmonary embolus, hypotension, and low cardiac output states such as cardiogenic shock.
Diffusion abnormality is caused by the obstruction or restriction of gas exchange across the capillary-alveolar membrane, as in pulmonary edema or pulmonary fibrosis. Inadequate oxygenation can also occur because of an inability of the cells to extract oxygen, such as in sepsis, carbon monoxide poisoning, or cyanide poisoning.
Inadequate Ventilation
Inadequate ventilation may result from neurologic causes such as spinal cord injury, traumatic brain injury, overdose, and Guillain-Barré syndrome. Muscular abnormalities that result from myopathies and myasthenia gravis will contribute to the failure to ventilate. Finally, anatomic causes such as pleural effusions, hemothorax, pneumothorax, flail chest, and abdominal hypertension may impair ventilation.
Definitions
There are important definitions related to mechanical ventilation that emergency nurses should be familiar with. Box 19-1 contains a summary of these.
Box 19-1
D efinitions for M echanical V entilation
• Acute lung injury (ALI): A severe form of ARDS characterized by acute hypoxemic respiratory failure, diffuse bilateral pulmonary infiltrates on chest x-ray film, pulmonary wedge pressure <18 mm Hg and PaO 2/F iO 2 ratio of <300.
• Acute respiratory distress syndrome (ARDS): The same definition as ALI except the PaO 2/F iO 2 ratio is <200.
• Barotrauma: Damage to the lung tissue due to high airway pressures. Alveolar rupture may lead to pneumothorax, pulmonary interstitial edema, and pneumomediastinum.
• F iO 2: Fraction of inspired oxygen ranges from 0.21 (21%) to 1.0 (100%). The normal ambient air F iO 2 is 0.21.
• Functional residual capacity (FRC): The volume of air remaining in the lungs at the end of normal expiration.
• Ideal body weight (IBW): The expected weight of a person based on sex and height.
Males: IBW = 50 kg + 2.3 kg for each inch over 5 feet.
Females: IBW = 45.5 kg + 2.3 kg for each inch over 5 feet.
• I:E ratio: The ratio of inspiratory time to expiratory time. Under normal conditions the expiratory phase is passive and is twice as long as the active inspiratory phase (1:2).
• Inspiratory flow: The rate at which a breath is delivered on a ventilator. It is measured in liters per minute. The higher the flow, the faster the breath is delivered.
• Inspiratory time (T i): The time over which a tidal volume is delivered or a pressure maintained (depending on mode). Set as I:E ratio or inspiratory flow.
• Mean airway pressure: The average pressure to which the lungs are exposed over one inspiratory/expiratory cycle.
• Minute ventilation (VE): The volume of air that moves in and out of the lungs in 1 minute. It is the product of the tidal volume and respiratory rate. V E = Vt × rate.
• Peak inspiratory pressure (PIP): The measurement in the lungs at the peak of inspiration as measured on the ventilator manometer.
• PEEP: Positive end-expiratory pressure. A therapy used in mechanical ventilation to provide airway pressure at the end of expiration to increase the volume of gas remaining in the lungs at the end of expiration (FRC). Ideally it will increase the surface area of the alveoli to decrease the shunting of blood through the lungs and improve gas exchange.
• Plateau pressure: A constant pressure value that is maintained during the inspiratory phase of ventilation. It is measured by pressing the pause or hold button during mechanical inspiration.
• Sensitivity: A measure of the amount of negative pressure that must be generated by a patient to trigger a mechanical ventilator into the inspiratory phase.
• Tidal volume (Vt): The volume of air inspired or expired in a single breath during regular respiration.
• Volutrauma: The volume-related overdistention injury of alveoli inflicted by mechanical ventilation.
• V/Q: Ventilation to perfusion ratio. Normal is 0.8. A high V/Q is indicative of dead space ventilation, and a low V/Q is indicative of shunt ventilation.
• VR: Ventilatory rate. Also referred to as frequency (f).
Classification of Mechanical Ventilators
There are two types of ventilators: positive pressure and negative pressure. It is highly unlikely that negative pressure ventilation (e.g., iron lung, cuirass) would ever be used in the ED setting. There are two types of positive pressure ventilation that will be used in the ED. The ventilator type is named for the parameter that terminates the inspiratory cycle of the ventilator: volume-controlled and pressure-controlled.
Volume-Controlled, Pressure Variable
This is the most common mode of ventilation. The tidal volume (Vt) is preset and delivered during the inspiratory phase of the ventilator cycle. Depending on the compliance and resistance of the lung, the pressure required to deliver the set tidal volume will vary. The advantage of this mode is that the patient receives guaranteed minute ventilation volumes. The disadvantage is the potential for lung injury when high pressures are required to deliver the set tidal volume in patients with low lung compliance.
Modes include controlled mandatory (or controlled) ventilation, assist-control (AC) ventilation, and synchronized intermittent mandatory ventilation (SIMV).
Pressure-Controlled, Volume Variable
In this mode of ventilation, the inspiratory pressure is preset and the ventilator will deliver a breath until that pressure is reached. The tidal volume delivered to reach that pressure will vary depending on the compliance and resistance of the lung. The advantage of this mode is that it limits the distending pressure of the lung. The mean airway pressure can be manipulated by prolonging the inspiratory time, thus reducing the potential for high peak or plateau pressures. The disadvantage is that the minute ventilation volume is not guaranteed and requires more attentive monitoring to prevent hypoventilation or hyperventilation.
Modes of Ventilation
Modes include pressure control and pressure support ventilation.
Controlled Mandatory Ventilation (CMV)
Method: Delivers a set respiratory rate at a set tidal volume, overriding any respiratory effort by the patient. This may cause physical discomfort for the patient and is usually used if the patient is unconscious or has received a neuromuscular blocking agent.
Set parameters: Fraction of inspired oxygen (F iO 2), Vt, ventilatory rate (VR), positive end-expiratory pressure (PEEP), ratio of inspiratory to expiratory time (I:E) or inspiratory time (T i).
Variable parameters: Peak inspiratory pressure (PIP).
Assist-Control Ventilation
Method: The ventilator will deliver a set number of respirations at a set tidal volume. Sensitivity is set at a level to recognize the patient’s respiratory effort with delivery of an additional full tidal volume with each spontaneous respiratory effort. The sensitivity can be adjusted so that it takes a specific amount of respiratory effort to recognize the respiratory effort.
The patient receives a breath whenever he or she wants one without having to work hard for it. Patients can hyperventilate in this mode, and minute ventilation should be monitored and the patient adequately sedated if indicated.
Set parameters: F iO 2, Vt, VR, flow, PEEP, sensitivity.
Variable parameters: PIP.
Synchronized Intermittent Mandatory Ventilation
Method: A set tidal volume at a set rate is delivered every minute. This type of ventilation allows the patient to breathe spontaneously but does not provide a spontaneous breath with additional tidal volume support. Sensitivity is set to ensure that the ventilator synchronizes the tidal volume breaths with the spontaneous breaths. A similar mode, intermittent mandatory ventilation (IMV), does not synchronize with the patient’s spontaneous breaths.
Patients with ALI or ARDS will have a difficult time generating sufficient effort to open the demand valve and breathe through the endotracheal tube without ventilatory assistance.
SIMV can be used in combination with pressure support to allow a spontaneous breath attempt to trigger the ventilator to give a pressure-limited breath.
Set parameters: F iO 2, Vt, VR, I:E or Ti, PEEP, sensitivity.
Variable parameters: PIP, sensitivity.
Pressure Controlled Ventilation (PCV)
Method: There is no guaranteed minute ventilation with this mode; therefore close monitoring to prevent hypoventilation and hypoxia is required. If the VR is set too fast, auto-PEEP can develop (see discussion of complications). Sensitivity is set to recognize the patient’s respiratory effort, and a full preset pressure is delivered with each ventilatory attempt (as opposed to assist-control, where volume is the set parameter). The sensitivity can be adjusted to require a specific amount of effort to occur for the patient’s respiratory effort to be recognized.
Mean airway pressure is increased by prolonging the inspiration time. In some patients, increasing the mean airway pressure without increasing PIP may require prolonging the inspiratory time to improve the oxygen benefit.
Set parameters: F iO 2, VR, PIP, PEEP, Ti or I:E
Variable parameters: Vt, flow.
Pressure Support Ventilation (PSV)
Method: Provides inspiratory support to a spontaneously breathing patient. The patient determines the rate and with each spontaneous effort triggers the ventilator to deliver a flow to the preset pressure limit. The pressure is maintained throughout inspiration.
This is often used for ventilator weaning purposes by gradually decreasing the pressure support provided.
Set parameters: F iO 2, PIP, sensitivity, PEEP.
Continuous Positive Airway Pressure (CPAP)
Method: No volume or pressure breaths are provided. The patient breathes spontaneously at his or her own rate and own tidal volume while the ventilator maintains a constant pressure throughout the respiratory cycle. This mode is used primarily to assess the patient’s ability to ventilate and oxygenate before extubation. It is also used in patients who have no oxygenation or ventilation abnormalities but only need airway protection, as in patients who are alert and awake but have laryngeal edema or airway compression. This mode should be used with caution in patients who have the potential to decompensate neurologically or hemodynamically.
Set parameters: PEEP, F iO 2.
Variable parameters: VR, Vt.
Preventing Injury From Mechanical Ventilation
A variety of strategies have been developed to reduce ventilator-associated injuries usually caused by high plateau pressures and high inspiratory pressures. The strategy most likely to be encountered in the ED is permissive hypercapnea.
Permissive Hypercapnea
Permissive hypercapnea is a lung protective strategy that decreases alveolar ventilation to prevent lung injury due to high volumes and high pressures. It involves the use of low tidal volumes (4 to 6 mL/kg ideal body weight [IBW]) and pressure-limited ventilation. The arterial carbon dioxide pressure (PaCO 2) is allowed to rise gradually, and the pH is allowed to drop to between 7.2 and 7.25. Acidosis at this level is generally well tolerated. 20 Permissive hypercapnea is not appropriate for patients with head injuries or severe metabolic acidosis.
Inverse-Ratio Ventilation (IRV)
The normal I:E ratio is reversed so that the inspiratory phase is longer than the expiratory phase. (2:1 to 4:1). It is usually done in the pressure control mode (PC/IRV).
The longer inspiratory time lowers the peak inspiratory pressure and plateau pressure while increasing the mean airway pressure. This prevents the potentially damaging effects of cyclical opening and closing of alveoli by maintaining a constant pressure and improving oxygenation.
This form of ventilation is extremely uncomfortable and almost always requires chemical paralysis and sedation.
Other Advanced Ventilatory Strategies
Further studies are needed to determine improved patient outcomes in the following modes.
HIGH-FREQUENCY OSCILLATORY VENTILATION
High-frequency oscillatory ventilation (HFOV) is characterized by high respiratory rates, generally between 180 and 360 breaths/min, with very low tidal volumes of 1 to 3 mL/kg. In HFOV the pressure oscillates, maintaining a constant distending pressure. Gas is pushed into the lungs during inspiration and pulled out during expiration. It is used in patients who have hypoxia refractory to normal mechanical ventilation. High-frequency ventilators for the adult population are not readily available.
AIRWAY PRESSURE-RELEASE VENTILATION (BILEVEL)
Airway pressure-release ventilation (APRV) is a time-cycled, pressure-limited form of ventilation that maintains a constant positive airway pressure (similar to plateau pressure) and has a regular, brief, intermittent release of airway pressure allowing for removal of carbon dioxide. This method allows the patient to breathe spontaneously so chemical paralysis is not required.
Depending on the brand of ventilator, a modified version of APRV provides pressure support during the spontaneous respiratory effort.
Tidal volume is variable, requiring close attention to the patient’s minute ventilation to prevent hypercapnea or hypocapnia.
Selecting Ventilator Settings
Ventilator mode and settings are determined by physician preference, clinical assessment, and degree of alteration in oxygenation and/or ventilation. Under the guidance of the physician, the respiratory therapist is the most skilled and knowledgeable person to set up and monitor ventilator parameters. The emergency nurse should be familiar with the concepts and therapies used and participate in collaborative discussions on the goal of ventilatory support.
Tidal Volume (Using Volume-Controlled Ventilation)
A Vt that is too high places the patient at risk for overinflation injury. Patients with acute lung injury or ARDS should be started on a Vt of 6 mL/kg IBW. In a randomized controlled study, the ARDS Network compared patient outcomes when using 6 mL/kg IBW versus the traditional 12 mL/kg IBW. Plateau pressure was maintained at less than 30 cm H 2O, and Vt in the low-volume group was dropped as low as 4 mL/kg if necessary to meet this limitation. The low-volume group had a 22% relative reduction in mortality. 1 A Vt of 8 mL/kg IBW is appropriate for patients with chronic obstructive pulmonary disease (COPD) and asthma so that fewer breaths are given at a higher Vt to allow for a longer exhalation time.
A Vt of 8 to 9 mL/kg should be adequate for people with normal lungs. Patients with neuromuscular disease may benefit from a slightly higher Vt to prevent atelectasis.
Pressure (Using Pressure-Controlled Ventilation)
Pressure will need to be adjusted as compliance changes (i.e., increase pressure support with decreased compliance, and decrease with increased compliance). Start with a pressure support of 20 cm H 2O, and adjust to a tidal volume of 6 to 8 mL/kg.
Rate
Respiratory rates that are set too fast place the patient at risk for inadequate expiratory time. When initially selecting the rate, consider the minute ventilation and the tidal volume. The desired minute ventilation is usually 5 to 10 L/min. The initial rate will generally range from 8 to 18 breaths/min depending on the tidal volume selected and the degree of acidosis. Draw a specimen for arterial blood gas (ABG) analysis 20 minutes after changing ventilator settings. Further adjustments of the rate depend on the clinical goal and patient response. The goal may be based on a PaCO 2 range (as in traumatic brain injury) or a pH range (as in passive hypercarbia). In summary, increased rate equals increased pH and decreased PaCO 2, whereas decreased rate equals decreased pH and increased PaCO 2.
F iO 2
If the patient’s arterial oxygen pressure (PaO 2) is unknown, start with a F iO 2 of 60% to 100%. The percentage of oxygen can be weaned down while monitoring oxygen saturation levels and arterial blood gases. The F iO 2 and PEEP should be managed to maintain the PaO 2 in the middle of the normal range for the given altitude. Patients with head injuries or heart problems should have a PaO 2 at the upper end of normal. ARDS and ALI patients can tolerate a PaO 2 in the lower end of the range so that lower F iO 2 and PEEP can be used, thereby lessening the chance of oxygen toxicity. Prolonged periods with a F iO 2 greater than 0.6 (60%) are associated with lung injury; however, it should be used, if necessary, to prevent hypoxemia.
PEEP
PEEP exerts pressure in the patient’s airway, above atmospheric level, to prevent alveolar collapse by increasing the functional residual capacity (FRC). PEEP can be used in any mode of ventilation. Most patients should receive 5 cm H 2O of PEEP to prevent atelectasis. Use PEEP with extreme caution (usually only 3 cm H 2O) in COPD and asthma patients to prevent further air trapping. PEEP is used in conjunction with F iO 2 to improve oxygenation. Higher levels of PEEP are helpful to decrease F iO 2 to less than 0.6 (60%). PEEP greater than 10 cm H 2O can cause decreased venous return and hypotension. The hemodynamic effects of PEEP should be monitored closely.
I:E Ratio
The normal inspiratory/expiratory ratio is 1:2 or 1:3. Patients with obstructive airway disease, such as asthma or COPD, should have longer expiratory times of 1:4 or longer to prevent air trapping and alveolar overdistention. In this patient population, increasing the rate, which shortens the expiratory time in an attempt to lower the PaCO 2, may actually increase PaCO 2 and worsen the clinical condition. 42
Sensitivity
The sensitivity is set to recognize the patient’s spontaneous respiratory effort. It is usually set at −1 to −2 cm H 2O. A setting that is too high will cause increased patient effort, and a setting that is too low may cause overtriggering of the ventilator and hyperventilation.
PIP
The PIP alarm should be set at 10 to 15 cm H 2O higher than baseline. This will alert staff to decreased lung compliance or conditions that do not allow full exhalation. Lung compliance will often decrease with fluid resuscitation and capillary leak associated with the inflammatory response. This will increase the peak inspiratory pressure.
Management of the Patient on Mechanical Ventilation
Chapter 30 contains information about specific treatment of patients with pulmonary disease and ABG analysis. F iO 2 and PEEP are the settings used to improve oxygenation (PaO 2). It is often a delicate balance of increasing the PEEP to achieve a F iO 2 below 0.6 while maintaining the mean arterial blood pressure above 65 mm Hg. Vt and VR are the settings used to adjust PaCO 2. The emergency nurse needs to continuously monitor the patient’s heart rate, electrocardiogram (ECG) pattern, and pulse oximetry readings. End-tidal CO 2 monitoring (EtCO 2) is a useful adjunct in the assessment of ongoing endotracheal tube placement in the trachea. It is of limited value in correlating to PaCO 2 in hemodynamically unstable patients or in patients with ventilation/perfusion (V/Q) mismatch. A self-inflating resuscitation bag should be kept at the patient’s bedside at all times in the event of mechanical failure. Suction equipment should be readily available. Endotracheal tube depth should be noted on the patient’s chart and assessed whenever the patient is moved or becomes agitated, air bubbles are noted in the airway, low or high PIP alarms are activated, vocal sounds are heard, or when there is any question of tube displacement. Be aware of and document the patient’s baseline F iO 2, mode of ventilation, PIP, PEEP/pressure support and tidal volume; documentation of these should occur every 2 hours while receiving mechanical ventilation. Assess the patient for any changes. Goals of oxygenation and ventilation should be clear. If no adjustment parameters are given, the ED nurse should notify the physician when any value falls outside the desired range.
Ventilator Management
Ventilator alarms should be on at all times and set to the maximum volume. Immediately evaluate the cause of any ventilator alarm. Table 19-1 contains a summary of how to troubleshoot ventilator alarms.
| CPAP, Continuous positive airway pressure; ETT, endotracheal tube. | ||
| ∗ Remove patient from the ventilator, and manually bag with a resuscitation bag if there is any compromise. | ||
| Alarm | Possible Causes | Management |
|---|---|---|
| Apnea | Insufficient spontaneous breathing by a patient in the CPAP or pressure support mode | • Switch ventilator mode to one that provides a set rate |
| High airway pressure | ETT obstruction: sputum, kink, biting Increased compliance or resistance: circumferential burns, bronchospasm, lung collapse, pneumothorax, endobronchial intubation, worsening of lung process Anxiety/fear/pain/fighting ventilator | • Suction the airway • Treat cause of resistance • Adjust mode or settings • Rule out hypoxia before treating agitation • Chest radiography analysis • Change ventilator mode to one that is better tolerated and/or provide sedation/analgesia |
| Low airway pressure | Ventilator disconnect Leak in ventilator system Cuff leak Inadvertent extubation | • Ensure that all connections are intact and tight • Troubleshoot ETT cuff • Bag-mask device if ETT was dislodged |
| Oxygen pressure low | Oxygen cylinder is empty Cylinder valve is closed Unit not connected to the wall terminal | • Check wall and cylinder connections • Bag-mask ventilation until resolved |
Monitor for signs and symptoms of barotrauma (see complications discussed later in the chapter).
Disconnect the patient from the ventilator and ventilate with a self-inflating resuscitation bag if there is any question as to whether the patient is being adequately ventilated. Be sure that the resuscitation bag has good oxygen flow, and use a PEEP valve if the patient is PEEP dependent (requires PEEP to adequately oxygenate). If it is necessary to sedate and administer a neuromuscular blocking agent to maintain adequate oxygenation, adjust the respiratory rate to the patient’s premedication minute ventilation and repeat an ABG analysis.
Complications of Mechanical Ventilation
There are multiple complications that may occur with mechanical ventilation. The following is a discussion of some that the emergency nurse may come across in the ED.
HYPOTENSION
Positive pressure ventilation increases intrathoracic pressure and subsequently decreases venous return and cardiac output. In patients with marginal or low volume status, the decrease in venous return will cause hypotension. The greater the positive pressure applied, the more profound the hypotensive response. This is most apparent when the PEEP is greater than 10 cm H 2O. Hemodynamic status should be monitored closely with any increase in PEEP and immediately after intubation. Optimizing fluid status will lessen the degree of hypotension.
VOLUTRAUMA
Volutrauma is the overdistention injury of alveoli inflicted by mechanical ventilation. It is most closely associated with high PIP. It is thought that this damage degrades surfactant, disrupts epithelial and endothelial cell barriers, and increases cytokine levels and inflammatory cells in the lung. 16. and 55. Lung-protective ventilatory strategies should be used in all patients with ALI or ARDS.
BAROTRAUMA
Barotrauma is the damage caused to lung tissue because of high airway pressures and rupture of alveoli. This may lead to a pneumothorax, tension pneumothorax, subcutaneous emphysema, or pneumomediastinum. Symptoms include hypotension, tachycardia, decrease in arterial oxygen saturation (SaO 2), decrease in central venous oxygen saturation/mixed venous oxygen saturation (ScvO 2/SvO 2), decrease in cardiac output, decreased breath sounds, unequal chest excursion, and deviated trachea. Large tidal volumes should be avoided and PIP and plateau pressures monitored carefully.
AUTO-PEEP
Auto-PEEP, also called intrinsic PEEP, occurs when a ventilator breath is not completely exhaled before the next delivered inspiratory breath (stacking breaths). This occurs most frequently in patients with asthma or COPD who require longer exhalation times. High tidal volumes along with high respiratory rates will also cause auto-PEEP. The resultant increasing pressures will cause barotrauma, volutrauma, hypotension, and death. Assessing for auto-PEEP includes monitoring the PIP and the respiratory waveforms on the ventilator for increasing baselines. If auto-PEEP is identified, the patient should be disconnected from the ventilator and allowed to completely exhale.
OXYGEN TOXICITY
A F iO 2 of greater than 0.5 for a long duration may cause the production of oxygen free radicals that damage pulmonary epithelium; inactivate surfactant; and form intraalveolar edema, interstitial thickening, and pulmonary fibrosis. 55 The extent of injury is related to the level of F iO 2 and the duration of exposure. Using PEEP in conjunction with F iO 2, if tolerated hemodynamically, will facilitate weaning the F iO 2 to less than 0.5. With severe ARDS/ALI it may not be possible to lower F iO 2 below 50%. However, treatment of hypoxemia and hypotension takes precedence over the possibility of oxygen toxicity.
INFECTION
Ventilator-associated pneumonia (VAP) is a serious and potentially life-threatening consequence of intubation and is defined as a nosocomial pneumonia that develops after 48 hours of intubation and mechanical ventilatory support. 44 VAP is the most common and fatal nosocomial infection of critical care, affecting between 9% and 27% of intubated patients. 46 VAP doubles the risk for dying, prolongs the duration of ventilation, and increases the length of stay in the critical care unit, total hospital length of stay, and cost of hospitalization. 44. and 46. VAP may be prevented by using the following measures:
• Rigorous hand washing
• Sterile suction technique
• Avoiding the routine use of saline lavage
• Aseptic airway technique
• Bronchial hygiene
• Regular oral care
• Elevating the head of the bed 30 degrees
Summary
To provide safe and competent mechanical ventilation the emergency nurse needs to be familiar with the functioning and management of ventilators. Mechanical ventilation can support critically ill or injured patients, but when inappropriately managed, can cause unnecessary harm.
INVASIVE MONITORING
Every year the number of critically ill patients presenting to the ED increases, and so does their length of stay in the ED. The focus on early diagnosis and therapy for myocardial infarction, stroke, sepsis, and other time-dependent emergencies has called upon ED personnel to initiate monitoring and therapy that has traditionally fallen to the critical care units. Familiarity with the principles and management of hemodynamic monitoring, as well as its limitations, is essential to accurately interpreting the data obtained. The goal of hemodynamic monitoring is to initiate and guide therapy in patients at risk for tissue hypoperfusion and subsequent organ dysfunction.
General Monitoring Principles
Several general principles can be applied when preparing for and monitoring patients with invasive lines:
• A catheter is inserted into the desired location (blood vessel or brain) for direct measurement. The catheter is connected to the transducer via monitoring tubing.
• The monitoring tubing that connects the catheter to the transducer is stiff, low-compliance tubing that prevents distortion of the signal from the blood vessel or brain to the transducer.
• The transducer system (unless using fiberoptic) is fluid filled and maintained with a flush solution. The solution is usually normal saline, with or without heparin added depending on hospital protocol, and is flushed before connection to the catheter. The transducer senses the pressure signal from the blood vessel or brain, converts it to an electrical waveform, and displays it on the monitor.
• Air should be removed from the flush solution and drip chamber when the bag is spiked. This will prevent air from entering the system should the fluid level become low or the bag turned on its side.
• The flush bag is pressurized to 300 mm Hg to overcome the pressure of the system and prevent backflow of blood.
• The transducer system allows very low infusion rates into the catheter to prevent clotting (2 to 3 mL/hr). The tubing should be disabled (clamped) when connected to intracranial monitoring systems. A fast-flush on the transducer allows for bypass of the restricted flow of fluid for initial priming of the system and for clearing of blood from the system.
• The tubing should be checked and cleared of all air bubbles, including stopcock ports. Air bubbles distort the waveform and can result in inaccurate measurements.
• Open-ended (vented) stopcock caps used for zeroing should be replaced with dead-end covers. This prevents serious blood loss should the stopcock become inadvertently turned to the open position. It also helps maintain sterility.
• Connections should be tight and placed where they can be visualized regularly. Loose connections can result in serious blood loss or infection.
• Set the monitor to the appropriate scale for the pressure being measured. Generally this is a scale of 0 to 20 mm Hg or 0 to 40 mm Hg for central venous pressures (CVP) and pulmonary artery pressures (PAP), 0 to 100 mm Hg for arterial pressure readings, and 0 to 50 mm Hg for intracranial pressure monitoring.
• The transducer should be properly aligned with the reference point when zeroing. For CVP, pulmonary artery (PA) catheters, and arterial pressures this is the phlebostatic axis located at the level of the fourth intercostal space and the midway point between the anteroposterior chest walls. Transducers used for intracranial pressure monitoring are usually placed at the level of the lateral or fourth ventricle—the tragus of the ear is a good reference point. Transducers placed above the reference point will result in a falsely elevated pressure, and transducers below the reference point will result in a false low value.
• Patency of the line should be checked regularly and whenever the waveform appears dampened.
• Coagulation status should be reviewed, considered, and reversed, if necessary, before insertion of any invasive line.
Arterial Blood Pressure Monitoring
Direct arterial blood pressure monitoring is accomplished with the insertion of a catheter into an artery. Although generally inserted into the radial artery, the brachial, femoral, and dorsalis pedis arteries can also be cannulated. The catheter is attached to a fluid-filled transducer system that converts the pressure to an electrical waveform and displays it on the monitor for concurrent continuous readings. The arterial waveform is pulsatile and depicts the systolic and diastolic phases of the cardiac cycle. The dicrotic notch on the waveform separates the systolic and diastolic phases (Figure 19-1).
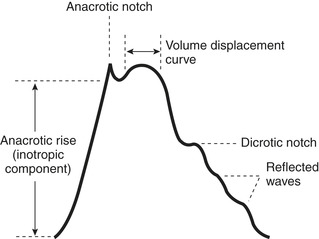 |
| FIGURE 19-1 The arterial waveform. Creation of the arterial pressure wave and acceleration of blood flow correlate with the inotropic upstrike. The rounded shoulder represents blood volume displacement and distention of the arterial walls. Normally the peak of both the inotropic and volume displacement phases are equal in amplitude. The descending limb represents diastolic runoff of blood; the dicrotic notch separates systole from diastole. Additional humps on the downslope relate to pulse waves reflected from the periphery. (From Davoric GO: Handbook of hemodynamic monitoring, ed 2, Philadelphia, 2004, Saunders.) |
The arterial pressure is determined by the cardiac output and the systemic vascular resistance (volume of blood flow versus resistance of the vessels). The relationship between pressure, flow, and volume is very complex; however, hypotension generally represents a failure of compensatory mechanisms after large-scale circulatory changes. 51 The sympathetic stress response will maintain a normal blood pressure despite declining blood volume and flow until it becomes exhausted. Blood pressure measurements are a useful screening tool and are helpful with trend assessment, but as a solitary measurement, they are of limited physiologic significance. 51
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
